Abstract
Background
Neoadjuvant systemic therapy (NST) is standard for locally advanced breast cancer and is now frequently considered for those with early-stage and node-positive disease. We aimed to evaluate the treatment course and outcomes in patients with disease progression during NST.
Methods
Patients diagnosed with unilateral stage I–III breast cancer between 2005 and 2015 with documented local-regional progression while receiving NST, by clinical examination and/or imaging after two or more cycles of chemotherapy, were identified from a prospective database, stratified by receipt of surgery and outcomes analyzed.
Results
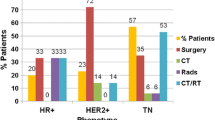
Of 6362 patients treated with NST during the study period, 124 (1.9%) developed disease progression. At a median live follow-up of 71 months, 23.4% were alive without disease and 70.2% had died from breast cancer. Median overall survival (OS) time for patients with progression was 26 months and median distant disease-free survival (DFS) was 14 months. Triple-negative breast cancer was associated with a higher likelihood of death (p < 0.001) and development of distant metastasis (p = 0.002). Among patients who had surgery (104, 89.3%), 40 (38.5%) developed local-regional recurrence, 67 (64.4%) developed distant metastasis, and 69 (66.3%) died from breast cancer. Median OS and median distant DFS in this subgroup was 31 and 16 months, respectively.
Conclusions
High rates of local-regional and distant failure were seen following disease progression while receiving NST. This suggests aggressive tumor biology and the need to study novel systemic therapies. Poor survival outcomes despite surgical management highlight the importance of careful patient selection when considering operative intervention after progression while receiving NST.


Similar content being viewed by others
References
Rastogi P, Anderson SJ, Bear HD, Geyer CE, Kahlenberg MS, Robidoux A, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26(5):778–85.
Bear HD, Anderson S, Smith RE, Geyer CE Jr, Mamounas EP, Fisher B, et al. Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2006;24(13):2019–27.
Fisher B, Bryant J, Wolmark N, Mamounas E, Brown A, Fisher ER, et al. Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol. 1998;16(8):2672–85.
Esserman LJ, Berry DA, DeMichele A, Carey L, Davis SE, Buxton M, et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 TRIAL—CALGB 150007/150012, ACRIN 6657. J Clin Oncol. 2012;30(26):3242–9.
Kuerer HM, Newman LA, Smith TL, Ames FC, Hunt KK, Dhingra K, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17(2):460–9.
Caudle AS, Gonzalez-Angulo AM, Hunt KK, Pusztai L, Kuerer HM, Mittendorf EA, et al. Impact of progression during neoadjuvant chemotherapy on surgical management of breast cancer. Ann Surg Oncol. 2011;18(4):932–8.
Caudle AS, Gonzalez-Angulo AM, Hunt KK, Liu P, Pusztai L, Symmans WF, et al. Predictors of tumor progression during neoadjuvant chemotherapy in breast cancer. J Clin Oncol. 2010;28(11):1821–8.
Raphael J, Paramsothy T, Li N, Lee J, Gandhi S. A single-institution experience of salvage therapy for patients with early and locally advanced breast cancer who progress during neoadjuvant chemotherapy. Breast Cancer Res Treat. 2017;163(1):11–9.
Myller S, Ipatti P, Jääskeläinen A, Haapasaari KM, Jukkola A, Karihtala P. Early progression of breast cancer during neoadjuvant chemotherapy may predict poorer prognoses. Acta Oncol. 2020;59(9):1036–42.
Zheng Y, Ding X, Zou D, Zhang F, Qin C, Yang H, et al. The treatment option of progressive disease in breast cancer during neoadjuvant chemotherapy: a single-center experience. Cancer Biol Ther. 2020;21(8):675–87.
American Cancer Society. Breast cancer: facts & figures 2019–2020. 2019 [cited 2020 Dec 16]. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf.
Boughey JC, McCall LM, Ballman KV, Mittendorf EA, Ahrendt GM, Wilke LG, et al. Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (Alliance) Prospective Multicenter Clinical Trial. Ann Surg. 2014;260(4):608–14 (discussion 614–6).
Houssami N, Macaskill P, von Minckwitz G, Marinovich ML, Mamounas E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer. 2012;48(18):3342–54.
Abraham HG, Xia Y, Mukherjee B, Merajver SD. Incidence and survival of inflammatory breast cancer between 1973 and 2015 in the SEER database. Breast Cancer Res Treat. 2021;185:229–38.
Liu J, Chen K, Jiang W, Mao K, Li S, Kim MJ, et al. Chemotherapy response and survival of inflammatory breast cancer by hormone receptor- and HER2-defined molecular subtypes approximation: an analysis from the National Cancer Database. J Cancer Res Clin Oncol. 2017;143(1):161–8.
Lund MJ, Trivers KF, Porter PL, Coates RJ, Leyland-Jones B, Brawley OW, et al. Race and triple negative threats to breast cancer survival: a population-based study in Atlanta, GA. Breast Cancer Res Treat. 2009;113(2):357–70.
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492–502.
Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL. Racial and ethnic disparities in cancer survival: the contribution of tumor, sociodemographic, institutional, and neighborhood characteristics. J Clin Oncol. 2018;36(1):25–33.
Warner ET, Tamimi RM, Hughes ME, Ottesen RA, Wong YN, Edge SB, et al. Racial and ethnic differences in breast cancer survival: mediating effect of tumor characteristics and sociodemographic and treatment factors. J Clin Oncol. 2015;33(20):2254–61.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
Nanda R, Liu MC, Yau C, Shatsky R, Pusztai L, Wallace A, et al. Effect of pembrolizumab plus neoadjuvant chemotherapy on pathologic complete response in women with early-stage breast cancer: an analysis of the ongoing phase 2 adaptively randomized I-SPY2 trial. JAMA Oncol. 2020;6(5):676–84.
Schmid P, Cortes J, Pusztai L, McArthur H, Kümmel S, Bergh J, et al. Pembrolizumab for early triple-negative breast cancer. N Engl J Med. 2020;382(9):810–21.
Cortes J, Cescon DW, Rugo HS, Nowecki Z, Im SA, Yusof MM, et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): a randomised, placebo-controlled, double-blind, phase 3 clinical trial. Lancet. 2020;396(10265):1817–28.
Mittendorf EA, Zhang H, Barrios CH, Saji S, Jung KH, Hegg R, et al. Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): a randomised, double-blind, phase 3 trial. The Lancet. 2020;396(10257):1090–100.
Brackstone M, Palma D, Tuck AB, Scott L, Potvin K, Vandenberg T, et al. Concurrent neoadjuvant chemotherapy and radiation therapy in locally advanced breast cancer. Int J Radiat Oncol Biol Phys. 2017;99(4):769–76.
von Gruenigen VE, Daly BJ. Futility: clinical decisions at the end-of-life in women with ovarian cancer. Gynecol Oncol. 2005;97(2):638–44.
Buyx AM, Friedrich DR, Schöne-Seifert B. Ethics and effectiveness: rationing healthcare by thresholds of minimum effectiveness. BMJ. 2011;342:d54.
Masuda N, Lee SJ, Ohtani S, Im YH, Lee ES, Yokota I, et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med. 2017;376(22):2147–59.
Von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med. 2019;380(7):617–28.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Benjamin Smith has received prior research funding from Varian Medical Systems, and has current royalty and equity interest in Oncora Medical. Funda Meric-Bernstam is a consultant for AbbVie, Aduro BioTech Inc., Alkermes, AstraZeneca, DebioPharm, eFFECTOR Therapeutics, F. Hoffman-La Roche Ltd, Genentech Inc., IBM Watson, Infinity Pharmaceuticals, Jackson Laboratory, Kolon Life Science, OrigiMed, PACT Pharma, Parexel International, Pfizer Inc., Samsung Bioepis, Seattle Genetics Inc., Tyra Biosciences, Xencor, and Zymeworks, and is a member of the Advisory Committee for Immunomedics, Inflection Biosciences, Mersana Therapeutics, Puma Biotechnology Inc., Seattle Genetics, Silverback Therapeutics, Spectrum Pharmaceuticals, and Zentalis. She has also undertaken sponsored research for Aileron Therapeutics, Inc. AstraZeneca, Bayer Healthcare Pharmaceutical, Calithera Biosciences Inc., Curis Inc., CytomX Therapeutics Inc., Daiichi Sankyo Co. Ltd, Debiopharm International, eFFECTOR Therapeutics, Genentech Inc., Guardant Health Inc., Klus Pharma, Takeda Pharmaceutical (formerly Millennium Pharmaceutical), Novartis, Puma Biotechnology Inc., and Taiho Pharmaceutical Co., and has received honoraria from Chugai Biopharmaceuticals. Kelly Hunt is a member of the Medical Advisory Board of Armada Health and Merck & Co., and has received research funding to her institution from Cairn Surgical, Eli Lilly and Company, Lumicell, and OncoNano Medicine. Leisha C. Elmore, Henry M. Kuerer, Carlos H. Barcenas, Makesha V. Miggins, Anthony Lucci, Abigail S. Caudle, and Mediget Teshome have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elmore, L.C., Kuerer, H.M., Barcenas, C.H. et al. Clinical Course of Breast Cancer Patients with Local-Regional Progression During Neoadjuvant Systemic Therapy. Ann Surg Oncol 28, 5477–5485 (2021). https://doi.org/10.1245/s10434-021-10444-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10444-w