Abstract
Background
Esophagectomy has major effects on health-related quality of life (HR-QoL). Postoperative complications might contribute to a decreased HR-QOL. This population-based study aimed to investigate the difference in HR-QoL between patients with and without complications after esophagectomy for cancer.
Methods
A prospective comparative cohort study was performed with data from the Netherlands Cancer Registry (NCR) and Prospective Observational Cohort Study of Esophageal-Gastric Cancer Patients (POCOP). All patients with esophageal and gastroesophageal junction (GEJ) cancer after esophagectomy in the period 2015–2018 were enrolled. The study investigated HR-QoL at baseline, then 3, 6, 9, 12, 18, and 24 months postoperatively, comparing patients with and without complications as well as with and without anastomotic leakage.
Results
The 486 enrolled patients comprised 270 patients with complications and 216 patients without complications. Significantly more patients with complications had comorbidities (69.6% vs 57.3%; p = 0.001). No significant difference in HR-QoL was found over time between the patients with and without complications. In both groups, a significant decline in short-term HR-QoL was found in various HR-QoL domains, which were restored to the baseline level during the 12-month follow-up period. No significant difference was found in HR-QoL between the patients with and without anastomotic leakage. The patients with grades 2 and 3 anastomotic leakage reported significantly more “choking when swallowing” at 6 months (ß = 14.5; 95% confidence interval [CI], − 24.833 to − 4.202; p = 0.049), 9 months (ß = 22.4, 95% CI, − 34.259 to − 10.591; p = 0.007), and 24 months (ß = 24.6; 95% CI, − 39.494 to − 9.727; p = 0.007) than the patients with grade 1 or no anastomotic leakage.
Conclusion
In general, postoperative complications were not associated with decreased short- or long-term HR-QoL for patients after esophagectomy for esophageal or GEJ cancer. The temporary decrease in HR-QoL likely is related to the nature of esophagectomy and reconstruction itself.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Curative treatment for patients with esophageal cancer usually consists of (neo)adjuvant chemo(radio) therapy and surgery. These treatments often are accompanied by side effects and complications.1,2 Surgeons strive to improve postoperative results by prehabilitation, Enhanced Recovery After Surgery (ERAS) programs, and minimally invasive surgery.3,4,5 However, more than 60% of esophagectomy patients still experience postoperative complications.1,6 A complicated postoperative course often is accompanied by an increase in anxiety and depression, impeding patients’ recovery from surgery.7,8 Complications also are related to a decreased survival.9
Several studies have investigated the impact of postoperative complications on health-related quality of life (HR-QoL) for cancer patients.10,11 Overall, cancer patients were found to report worse long-term HR-QoL after postoperative complications. A systematic review and meta-analysis have been performed encompassing 50 studies investigating the impact of complications on long-term HR-QoL after cardiac, thoracic, gastrointestinal (GI), and vascular surgery. A negative effect of postoperative complications on patients’ HR-QoL 12 months after operation was found.11
Few studies have investigated long-term HR-QoL of patients with and without complications after an esophagectomy.12,13,14,15 Overall, an impaired short- and long-term HR-QoL has been reported by patients with postoperative complications versus patients without postoperative complications. Also, the occurrence of anastomotic leakage has been associated with worse short-term HR-QoL.15 However, these studies either did not include a baseline measurement, were performed before the implementation of minimally invasive surgery, did not include information on (neo)adjuvant treatment, or were conducted in a single center with a limited number of patients.12,13,14,15
This study aimed to investigate the difference in short- and long-term HR-QoL for patients with and without a complicated postoperative course after multimodality treatment for esophageal and gastroesophageal junction (GEJ) cancer in a nationwide cohort. We hypothesized that postoperative complications negatively influence short- and long-term HR-QoL.
Methods
Study Design
A population-based prospective comparative cohort study was performed with data from the Prospective Observational Cohort Study of Esophageal-Gastric Cancer Patients (POCOP) study and the Netherlands Cancer Registry (NCR).
Prospective Observational Cohort Study of Esophageal-Gastric Cancer Patients Database
The POCOP is a nationwide Dutch, population-based, observational cohort study of patient-reported outcome measures data from cancer patients, including those with esophageal or gastric cancer. The POCOP aims to gain insight into the quality-of-life course experienced by cancer patients.16 The inclusion of patients started in December 2015 in AMC, and during the period from 2016 to 2019, an additional 53 medical centers joined the POCOP study. All the patients with esophageal or gastric cancer in the 54 participating medical centers are asked to participate in the POCOP study irrespective of whether they receive curative treatment or palliative treatment.
Among other forms, the patients in the study complete the validated European Organization for Research and Treatment of Cancer (EORTC) quality-of-life questionnaires at baseline before initiation of treatment, after 3, 6, 9, 12, 18, and 24 months, then annually thereafter.17 The POCOP study included 261 patients in 2016, 741 patients in 2017, 1423 patients in 2018, and 2065 patients in 2019. The rationale and design of the POCOP study have been described elsewhere.16
The inclusion criteria for the POCOP specified patients with a diagnosis of esophageal or gastric cancer. For the current study, the inclusion criteria specified patients with esophageal and GEJ cancer who underwent an esophagectomy during the period of 2015–2018. The exclusion criteria ruled out patients who underwent surgery for recurrent disease, patients who underwent salvage or palliative surgery, patients with a recurrence, patients undergoing a colon or jejunal interposition, and patients who had no reconstruction performed or required emergency surgery.
Informed consent was collected by the POCOP, and the Privacy Review Board of NCR approved this study. The POCOP study adheres to the required rules and regulations.16 Ethical approval for this study was not required under Dutch law. This manuscript was composed using the STROBE checklist.18
The Netherlands Cancer Registry
The NCR manages data from all cancer patients in the Netherlands. This database stores patient, tumor, and treatment information such as gender, age at diagnosis, tumor type and stage, diagnostic data, information on (neo)adjuvant treatment and surgery, postoperative morbidity and mortality, and the hospital in which the patient was treated. All hospitals are required by Dutch law to provide this information to the NCR. The NCR does not register the severity of postoperative complications (Clavien-Dindo grade), nor does it subdivide pulmonary morbidity into separate pulmonary complications. The clinical outcome data of the NCR cancer patients were combined with the POCOP patient-reported outcome measures for research purposes.
Multimodality Treatment Including Esophagectomy with Curative Intent
The patients with an advanced (≥cT2N0 or cT1N+) esophageal or GEJ carcinoma usually have been treated with chemoradiotherapy according to the CROSS (ChemoRadiotherapy for Oesophageal cancer Followed by Surgery Study) scheme.19 In selected cases (e.g., > 2 cm involvement of the stomach), perioperative chemotherapy (previously the MAGIC (Medical Research Council Adjuvant Gastric Infusional Chemotherapy trial), and increasingly during this study period, the FLOT scheme (Fluorouracil, Leucovorin, Oxaliplatin and doceTaxel)) has been administered.20,21 After neoadjuvant therapy, a transthoracic or transhiatal esophagectomy with a one- or two-field lymphadenectomy and gastric conduit reconstruction using a cervical or intrathoracic anastomosis has been performed by an open, minimally invasive, or hybrid approach.
Postoperative Complications
The postoperative complications included in the NCR database comprise pulmonary complications, anastomotic leakage, cardiovascular complications, chyle leakage, wound abscess or infection, recurrent laryngeal nerve palsy, thromboembolic complication, and other neurologic complications. Pneumonia was defined as a new or progressive lung infiltration confirmed by radiologic imaging in combination with at least two of the following clinical manifestations: leukocytosis or leukopenia, fever ( > 38 °C), and purulent secretion.22 Anastomotic leakage was divided into grades 1–3 according to the Esophageal Complications Consensus Group (ECCG)23 as follows: grade 1 (a leakage without the need for a therapy change except for dietary changes), grade 2 (a local leakage requiring an intervention other than surgery), and grade 3 (a leakage requiring surgery). The severity of other complications, such as those categorized by the Clavien-Dindo classification,24,25 is not registered in the NCR database. The definitions of the postoperative complications used in the NCR can be found in Table S1.
Outcomes: Quality of Life According to EORTC Questionnaires
The validated cancer-specific European Organisation of Research and Treatment of Cancer (EORTC) QLQ-C30 and the tumor-specific EORTC QLQ-OG25 questionnaires were used for this study.26,27 The EORTC QLQ-C30 HR-QoL domains were global health (calculated from two questions with response categories ranging from 1 (very poor) 7 (excellent), five functioning scales (physical, role, social, and cognitive and emotional functioning) calculated from 15 questions with response categories ranging from 1 (not at all) to 4 (very much), and scores for nine symptoms (fatigue, nausea and vomiting, pain, dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial difficulties) calculated from 13 questions with response categories ranging from 1 (not at all) to 4 (very much).26
The EORTC QLQ-OG25 questionnaire contains 25 questions assessing 16 HR-QoL domains (body image, reflux, dysphagia, pain and discomfort, odynophagia, anxiety, problems with eating, problems with eating with others, trouble with swallowing of saliva, dry mouth, trouble with taste, choking when swallowing, trouble with talking, trouble with coughing, worrying about weight loss, and problems with hair loss). All the questions of the EORTC QLQ-OG25 questionnaire had response categories ranging from 1 (not at all) to 4 (very much).27 The 31 HR-QoL domain scores were linearly transformed into scores ranging from 0 to 100. Missing data were managed according to the EORTC scoring manual.26,27 According to this scoring, a higher score in the global health and functioning domains represents better global health and functioning, and a higher score in the symptom domains represents more symptomatology.
Statistical Analysis
The chi-square test and Fisher's exact test were used for categorical variables to compare baseline characteristics between the groups. The Shapiro-Wilk test was used to check the distribution pattern of continuous variables. For continuous variables, a Mann-Whitney U test was used if the variable was not normally distributed (median with an interquartile range [IQR]), and Student’s t test was used if the variable was normally distributed (mean ± standard deviation).
To examine the difference in HR-QoL over time between patients with and without postoperative complications after an esophagectomy, linear mixed-models analysis was performed. To correct for multiple testing, a Bonferroni correction was performed by multiplying the p value by the number of tests performed. If a p value lower than 0.05 was reached after linear mixed-models analysis and correction for multiple testing, a univariable linear regression analysis was performed for each follow-up time separately to determine the follow-up point at which the difference in HR-QoL between the patients with and without postoperative complications was significant. We did not perform multivariable analyses to adjust for possible a priori differences because our goal was to investigate the difference in HR-QoL in a naturally occurring population.
Univariable linear regression analysis and Bonferroni correction for multiple testing were performed to examine the change in HR-QoL between baseline, short-term (3, 6, and 9 months), and long-term (12, 18, and 24 months) follow-up evaluations for patients with postoperative complications and patients without postoperative complications separately.
A subgroup analysis was performed to compare the HR-QoL between patients with and without anastomotic leakage, and between patients with grade 2 or 3 anastomotic leakage and those with grade 1 or no anastomotic leakage over time using linear mixed-models analyses. In addition, a separate analysis was performed to investigate the HR-QoL for patients with either a cervical or an intrathoracic anastomosis. Given the small number of patients with anastomotic leakage (n = 83) and grade 2 or 3 anastomotic leakage (n = 54), a stringent p value lower than 0.001 was chosen as statistically significant in the linear mixed-models analysis. A p value lower than 0.05 was chosen as statistically significant in all other analyses.
Because the minimally important change in mean scores representing clinical relevance varies between HR-QoL domains,26,28 a cutoff point of 10 points is most likely the upper bound for most HR-QoL domains. Therefore, in the current study, a mean HR-QoL score difference or change of more than 10 points was considered clinically relevant.
Results
Patient and Tumor Characteristics
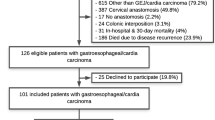
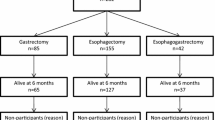
The study enrolled 486 patients after an esophagectomy (Table 1). The response rate of the POCOP study was 69.6% at baseline and decreased to 12.5% at 24 months. However, these percentages were based on all the included patients (i.e., the patients undergoing palliative treatment, definitive chemoradiotherapy, primary surgery, or neoadjuvant treatment and surgery). The decrease in response rate was partially attributable to the death of part of this patient population. The exact response rate of the current study population at baseline could not be calculated because such detailed information was not registered separately. However, compared with baseline, the response rates of the current study population were 81.9% at 3 months, 77.7% at 6 months, 68.1% at 9 months, 60.9% at 12 months, 42.0% at 18 months, and 23.3% at 24 months of follow-up evaluation.
The majority of the included patients in this study were male (79.8%), and the median age was 66 years (IQR, 60–70 years). Most of the patients were treated with neoadjuvant therapy (90.9%). Postoperative complications occurred for 55.6% (n = 270) of all the patients (Table 2). Among the most frequent complications were pulmonary complications (22.6%), anastomotic leakage (17.1%), and cardiac complications (11.3%). Of patients with anastomotic leakage, 27.7% had grade 1, 41% had grade 2, 24.1% had grade 3, and 7.2% had an unknown grade anastomotic leakage.
The patients with complications had significantly more comorbidities in general (69.6% vs 57.3%; p = 0.001) and pulmonary comorbidities in particular (14.8% vs 5.6%; p = 0.004). Significantly more minimally invasive esophagectomies (86.7% vs 71.3%; p = 0.008) and more cervical anastomoses (37.8% vs 20.8%; p = 0.002) were performed in the group with postoperative complications. The patient, treatment and tumor characteristics are presented in Table 1.
Comparison of HR-QoL Between the Patients with and Without Postoperative Complications
After linear mixed-models analyses and Bonferroni correction for multiple testing, none of the HR-QoL domains were found to differ significantly at baseline or 3, 6, 9, 12, 18, and 24 months after operation between the patients with and without postoperative complications (Tables 3 and S2).
Change in HR-QoL for the Patients with No Postoperative Complications
A univariable linear regression analysis of the HR-QoL domains was performed between baseline and the 3-, 6-, 9-, 12-, 18-, and 24-month follow-up evaluations for the patients without postoperative complications (Table S3). In eight HR-QoL domains (“trouble with coughing” [at 6 and 9 months], “role functioning,” “fatigue” and “trouble with taste” [at 3 and 6 months], “physical functioning,” “dyspnea,” “appetite loss,” and dry mouth [at 6 months]), a significant and clinically relevant decline in short-term HR-QoL scores compared with baseline was found, which had recovered to the baseline level at the 12-month follow-up evaluation (Fig. 1).
Change in health-related quality of life (HR-QoL) for patients without postoperative complications. A A significant decline in short-term HR-QoL score compared with baseline was found in the following eight HR-QoL domains, which had recovered to baseline level at the 12-month follow-up visit: “physical functioning” (at 3, 6, and 9 months, p < 0.001), “role functioning” (at 3 and 6 months, p < 0.001), “fatigue” (at 3 and 6 months, p = 0.002), “trouble with coughing” (at 3 months, p = 0.047; at 6 and 9 months, p ≤ 0.001), “dyspnea” (at 6 months, p < 0.001), “appetite loss” (at 6 months, p < 0.001), “dry mouth” (at 6 months, p = 0.004), and “trouble with taste” (at 3 months, p = 0.005; at 6 months, p < 0.001). B,C In three HR-QoL domains, the HR-QoL score either remained significantly impaired (“reflux,” p = 0.001) or improved significantly (“emotional functioning,” p = 0.003; “diarrhea,” p < 0.001) during a long-term follow-up period compared with baseline. D,E,F In four HR-QoL domains, the short-term HR-QoL score improved compared with baseline, and remained significantly improved (“dysphagia” and “odynophagia,” p ≤ 0.001) or became significantly impaired (“anxiety,” p < 0.001) during the long-term follow-up period, or recovered to baseline level during the short-term follow-up period (“trouble talking,” p = 0.001).
Change in HR-QoL for the Patients with Postoperative Complications
A univariable linear regression analysis of the HR-QoL domains was performed between baseline and the 3-, 6-, 9-, 12-, 18-, and 24-month follow-up evaluations for the patients with postoperative complications (Table S4). In 10 HR-QoL domains (“role functioning” and “dyspnea” [at 3, 6, and 9 months], “trouble with coughing” [at 6 and 9 months], “social functioning,” “fatigue,” “appetite loss,” “dry mouth,” “trouble with taste,” “diarrhea,” and “trouble talking” [at 6 months]), scores denoting clinically relevant and significantly more impaired short-term HR-QoL compared with baseline were found, which had recovered to baseline level at the 12-month follow-up evaluation (Fig. 2).
Change in health-related quality of life (HR-QoL) for patients with postoperative complications. A A significant decline in short-term HR-QoL score compared with baseline was found in the following 12 HR-QoL domains, which recovered to baseline level during the 12-month follow-up period: “role functioning” (at 3 and 6 months, p < 0.001; at 9 months, p = 0.027), “social functioning” (at 3 months, p = 0.010; at 6 months, p < 0.001; at 9 months, p = 0.035), “fatigue” (at 6 months, p < 0.001), “dyspnea” (at 3 and 6 months, p < 0.001; at 9 months, p = 0.006), “appetite loss” (at 6 months, p < 0.001), “diarrhea” (at 6 months, p < 0.001; at 9 months, p = 0.007), “eating” (at 6 months, p = 0.021), “reflux” (at 9 months, p = 0.013), “dry mouth” (at 6 months, p < 0.001), “trouble with taste” (at 6 months, p < 0.001), “trouble with coughing” (at 6 and 9 months, p < 0.001), and “trouble talking” (at 6 months, p < 0.001). B A significant decline in the “physical functioning” score was found during the follow-up visits at 3, 6, and 9 months (p < 0.001) and at 12 months (p = 0.045), which had recovered to baseline level at the 18-month follow-up visit. C In the following five HR-QoL domains, an improved HR-QoL score compared with baseline was found at all the follow-up times: “odynophagia” (at 3 months, p = 0.001; at 6 months, p = 0.029; at 9, 12, 18, and 24 months, p < 0.001), “anxiety” (at 9, 12, 18, and 24 months, p < 0.001), “pain and discomfort” (at 3 months, p = 0.006), “problems with hair loss,” p < 0.001), and“dysphagia” (at 24 months, p < 0.001).
HR-QoL After Anastomotic Leakage
The HR-QoL scores were compared between the patients with anastomotic leakage (n = 83) and the patients without anastomotic leakage (n = 360) over time. After linear mixed-models analysis and Bonferroni correction, no p value below 0.001 was found in any of the domains (data not shown). The HR-QoL scores also were compared between the patients with severe (grade 2 or 3) anastomotic leakage (n = 54) and the patients with grade 1 or no anastomotic leakage (n = 432) over time (Table S5). After linear mixed-models analysis and Bonferroni correction, a significant difference in HR-QoL over time was found in the “choked when swallowing” domain (p < 0.001; Table 4). After univariable linear regression analysis and correction for multiple testing, the patients with grade 2 or 3 anastomotic leakage showed significantly more reported problems with “choking when swallowing” than the patients with grade 1 or no anastomotic leakage in follow-up evaluations at 6 months (mean difference, 14.5; 95% CI, − 24.833 to − 4.202; p = 0.049), 9 months (mean difference, 22.4; 95% CI, − 34.259 to − 10.591; p = 0.007), and 24 months (mean difference, 24.6; 95% CI, − 39.494 to − 9.727; p = 0.007) (Table 5). The mean scores differed more than 10 points and were therefore clinically relevant.
HR-QoL After Cervical and Intrathoracic Anastomosis
The HR-QoL scores for the patients who had esophagectomy with a cervical anastomosis (n = 147) were compared over time with the HR-QoL scores of the patients who had esophagectomy with an intrathoracic anastomosis (n = 308). After linear mixed-models analysis and Bonferroni correction, no significant difference was found in any of the domains (data not shown).
Discussion
This study investigated the difference in the short- and long-term HR-QoL for patients with and without postoperative complications after multimodality treatment including an esophagectomy with curative intent for esophageal or GEJ cancer in a nationwide cohort. The results of this study showed that in general, the short- and long-term HR-QoL does not differ between patients with and without postoperative complications after esophagectomy. However, grade 2 or 3 anastomotic leakage was found to affect “chocking when swallowing” compared with grade 1 or no anastomotic leakage.
The absence of differences in HR-QoL between the patients with and without postoperative complications is in contrast to our hypothesis. When investigated separately, in both groups a decline in various short-term HR-QoL domain scores was found that was restored to baseline level with time. The observed impairment in HR-QoL is therefore more likely to be attributable to functional complaints related to the reconstruction after esophagectomy, and remarkably, complications do not seem to influence this. A recent prospective multicenter study showed that the majority of patients have functional complaints that last up to more than 1 year after an esophagectomy.29 The authors found a relation between the absence of 30-day complications and HR-QoL, with an increased physical, social, role functioning, and global health status in the group without complications.
Few other studies have investigated the influence of postoperative complications on HR-QoL after an esophagectomy.12,13,14,15 Overall, an impaired HR-QoL was found at the 6-month follow-up evaluations of patients with postoperative complications versus patients without postoperative complications.13,14,15 Anastomotic leakage, one of the most severe postoperative complications associated with the development of strictures,30 was found to be associated with odynophagia and eating difficulties 6 months after an esophagectomy with an intrathoracic anastomosis.15 Only one study investigated the impact of major postoperative complications on long-term HR-QoL and found that the patients with major postoperative complications reported more dyspnea, fatigue, and eating restrictions 6 months, 3 years, and 5 years after the operation than the patients with no postoperative complications.13 The negative impact of postoperative complications on HR-QoL was found to last up to 10 years postoperatively.12 The majority of these studies reported only major postoperative complications, although no complication grading system was used to define the severity of the complications.12,13,14
In 2016, the national audit for upper GI cancer (DUCA) started with the registration of the Clavien-Dindo classification for postoperative complications. Between 2016 and 2017, the results showed that 1046 (65%) of 1617 patients had a complication after their esophagectomy. Altogether, 529 patients (33%) had pulmonary complications, with pneumonia as the most common complication (341 cases; 21% of all complications and 64% of all pulmonary complications). Of the patients with a complication, 29% had Clavien-Dindo grade 3 or higher complications.1 The majority of the patients in the current study may have had a complication below Clavien-Dindo grade 3, which may explain the absence of differences in HR-QoL found between the patients with and without postoperative complications. In addition, the patients with more severe anastomotic leakage (grade 2 or 3), reported more problems with “choking when swallowing” at the 6-, 9-, and 24-month follow-up evaluation. This accords with a previous study that found significantly more odynophagia and problems with eating among patients with anastomotic leakage than among patients without an anastomotic leakage 6 months after an esophagectomy with an intrathoracic anastomosis.15 In addition, because problems with eating also are known to be dependent on the anastomotic site,31 we performed an analysis comparing HR-QoL between the patients with cervical and intrathoracic anastomoses and found no significant difference in HR-QoL between these two groups. However, because the number of patients in the grades 2 and 3 anastomotic leakage group was limited, this finding may have been due to chance despite the use of a Bonferroni procedure.
This study had a number of limitations. Selection bias could have occurred because it was unknown how many patients were eligible and how many had died during the follow-up period. In addition, the reasons for declining participation were not recorded. The results also could have been influenced by the decline in the response rate in the long-term follow-up evaluation. Moreover, this was a population-based, non-randomized cohort study of patients who differed in the number of postoperative complications. Therefore, the two groups differed with respect to a number of baseline variables including occurrence of (pulmonary) comorbidities, surgical technique (open, minimally invasive, hybrid), surgical approach (transthoracic, transhiatal), and location of anastomosis (cervical, intrathoracic). No correction for confounders was performed because we aimed to investigate the difference in HR-QoL in a naturally occurring population considering age, gender, comorbidities, and surgical technique. Furthermore, recurrent laryngeal nerve palsy also likely is independently related to HR-QoL. However, only a small number of patients in this study (n = 13) had a recurrent laryngeal nerve palsy, so no reliable subgroup analysis could be performed. Also, it was not possible to investigate the influence of severity of complications according to Clavien-Dindo grade, nor to investigate the influence of separate pulmonary complications on HR-QoL because the NCR does not register these data.
A strength of this study was that it investigated a population-based prospective cohort, which counteracted the selection bias seen in randomized clinical trials that use strict inclusion criteria. Also, this study included a large sample of post-esophagectomy patients treated after implementation of improvements in esophageal cancer treatment, including minimally invasive surgery and neoadjuvant/perioperative therapy.
To counteract the bias of multiple testing, a Bonferroni correction was performed. Because the number of patients with grade 2 or 3 anastomotic leakage was relatively small, a more stringent p value (p < 0.001) was chosen for this subgroup analysis. Also, to prevent over-interpretation of the clinical relevance of the results, a mean HR-QoL score change of more than 10 points was considered clinically relevant for all the HR-QoL domains.
Conclusion
Patients with and without complications after esophagectomy generally report comparable short- and long-term HR-QoL up to 24-months after surgery. In this study, both groups of patients showed a decline in short-term HR-QoL in various domains, which was restored to baseline levels with time. The patients with grade 2 or 3 anastomotic leakage reported worse HR-QoL in a single HR-QoL domain (“choking when swallowing”) than the patients with grade 1 or no anastomotic leakage. The temporary decrease in HR-QoL likely was related to the nature of the esophagectomy and reconstruction itself, and future research should focus on how to minimize these functional complaints.
References
van der Werf LR, Busweiler LAD, van Sandick JW, van Berge Henegouwen MI, Wijnhoven BPL; Dutch Upper GI Cancer Audit (DUCA) group. Reporting National Outcomes After Esophagectomy and Gastrectomy According to the Esophageal Complications Consensus Group (ECCG). Ann Surg. 2020;271(6):1095–1101. https://doi.org/10.1097/SLA.0000000000003210.
van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, Richel DJ, Nieuwenhuijzen GA, Hospers GA, Bonenkamp JJ, Cuesta MA, Blaisse RJ, Busch OR, ten Kate FJ, Creemers GJ, Punt CJ, Plukker JT, Verheul HM, Spillenaar Bilgen EJ, van Dekken H, van der Sangen MJ, Rozema T, Biermann K, Beukema JC, Piet AH, van Rij CM, Reinders JG, Tilanus HW, van der Gaast A; CROSS Group. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84. https://doi.org/10.1056/NEJMoa1112088.
Lau CSM, Chamberlain RS. Prehabilitation programs improve exercise capacity before and after surgery in gastrointestinal cancer surgery patients: a meta-analysis. J Gastrointest Surg. 2019;24:2829–37.
Gianotti L, Sandini M, Romagnoli S, Carli F, Ljungqvist O. Enhanced recovery programs in gastrointestinal surgery: Actions to promote optimal perioperative nutritional and metabolic care. Clin Nutr. 2020;39(7):2014–24. https://doi.org/10.1016/j.clnu.2019.10.023
Straatman J, van der Wielen N, Cuesta MA, Daams F, Roig Garcia J, Bonavina L, Rosman C, van Berge Henegouwen MI, Gisbertz SS, van der Peet DL. Minimally Invasive Versus Open Esophageal Resection: Three-year Follow-up of the Previously Reported Randomized Controlled Trial: the TIME Trial. Ann Surg. 2017;266(2):232-36. https://doi.org/10.1097/SLA.0000000000002171
Low DE, Kuppusamy MK, Alderson D, Cecconello I, Chang AC, Darling G, Davies A, D'Journo XB, Gisbertz SS, Griffin SM, Hardwick R, Hoelscher A, Hofstetter W, Jobe B, Kitagawa Y, Law S, Mariette C, Maynard N, Morse CR, Nafteux P, Pera M, Pramesh CS, Puig S, Reynolds JV, Schroeder W, Smithers M, Wijnhoven BPL. Benchmarking Complications Associated with Esophagectomy. Ann Surg. 2019;269(2):291–98. https://doi.org/10.1097/SLA.0000000000002611
Walburn J, Vedhara K, Hankins M, Rixon L, Weinman J. Psychological stress and wound healing in humans: a systematic review and meta-analysis. J Psychosom Res. 2009;67(3):253–71. https://doi.org/10.1016/j.jpsychores.2009.04.002.
Woodfield J, Deo P, Davidson A, Chen TY, van Rij A. Patient reporting of complications after surgery: what impact does documenting postoperative problems from the perspective of the patient using telephone interview and postal questionnaires have on the identification of complications after surgery? BMJ Open. 2019;9(7):e028561. https://doi.org/10.1136/bmjopen-2018-028561.
van der Werf LR, Wijnhoven BPL, Fransen LFC, van Sandick JW, Nieuwenhuijzen GAP, Busweiler LAD, van Hillegersberg R, Wouters MWJM, Luyer MDP, van Berge Henegouwen MI. A National Cohort Study Evaluating the Association Between Short-term Outcomes and Long-term Survival After Esophageal and Gastric Cancer Surgery. Ann Surg. 2019;270(5):868–76. https://doi.org/10.1097/SLA.0000000000003520.
Archer S, Pinto A, Vuik S, Bicknell C, Faiz O, Byrne B, Johnston M, Skapinakis P, Athanasiou T, Vincent C, Darzi A. Surgery, Complications, and Quality of Life: A Longitudinal Cohort Study Exploring the Role of Psychosocial Factors. Ann Surg. 2019;270(1):95–101. https://doi.org/10.1097/SLA.0000000000002745
Pinto A, Faiz O, Davis R, Almoudaris A, Vincent C. Surgical complications and their impact on patients' psychosocial well-being: a systematic review and meta-analysis. BMJ Open. 2016;6(2):e007224. https://doi.org/10.1136/bmjopen-2014-007224
Kauppila JH, Johar A, Lagergren P. Postoperative complications and health-related quality of life 10 years after esophageal cancer surgery. Ann Surg. 2020;271:311–6.
Derogar M, Orsini N, Sadr-Azodi O, Lagergren P. Influence of major postoperative complications on health-related quality of life among long-term survivors of esophageal cancer surgery. J Clin Oncol. 2012;30(14):1615–29. https://doi.org/10.1200/JCO.2011.40.3568.
Scarpa M, Saadeh LM, Fasolo A, Alfieri R, Cagol M, Cavallin F, Pinto E, Zaninotto G, Ancona E, Castoro C. Health-related quality of life in patients with oesophageal cancer: analysis at different steps of the treatment pathway. J Gastrointest Surg. 2013;17(3):421–33. https://doi.org/10.1007/s11605-012-2069-1.
van der Schaaf M, Lagergren J, Lagergren P. Persisting symptoms after intrathoracic anastomotic leak following oesophagectomy for cancer. Br J Surg. 2012;99:95–9.
Coebergh van den Braak RRJ, van Rijssen LB, van Kleef JJ, Vink GR, Berbee M, van Berge Henegouwen MI, Bloemendal HJ, Bruno MJ, Burgmans MC, Busch ORC, Coene PPLO, Coupé VMH, Dekker JWT, van Eijck CHJ, Elferink MAG, Erdkamp FLG, van Grevenstein WMU, de Groot JWB, van Grieken NCT, de Hingh IHJT, Hulshof MCCM, Ijzermans JNM, Kwakkenbos L, Lemmens VEPP, Los M, Meijer GA, Molenaar IQ, Nieuwenhuijzen GAP, de Noo ME, van de Poll-Franse LV, Punt CJA, Rietbroek RC, Roeloffzen WWH, Rozema T, Ruurda JP, van Sandick JW, Schiphorst AHW, Schipper H, Siersema PD, Slingerland M, Sommeijer DW, Spaander MCW, Sprangers MAG, Stockmann HBAC, Strijker M, van Tienhoven G, Timmermans LM, Tjin-A-Ton MLR, van der Velden AMT, Verhaar MJ, Verkooijen HM, Vles WJ, de Vos-Geelen JMPGM, Wilmink JW, Zimmerman DDE, van Oijen MGH, Koopman M, Besselink MGH, van Laarhoven HWM; Dutch Pancreatic Cancer Group, Dutch Upper GI Cancer Group and PLCRC working group. Nationwide comprehensive gastro-intestinal cancer cohorts: the 3P initiative. Acta Oncol. 2018 Feb;57(2):195–202. https://doi.org/10.1080/0284186X.2017.1346381.
EORTC. 2020. http://www.eortc.org. Accessed 1 Jan 2020.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008.
Shapiro J, van Lanschot JJB, Hulshof MCCM, van Hagen P, van Berge Henegouwen MI, Wijnhoven BPL, van Laarhoven HWM, Nieuwenhuijzen GAP, Hospers GAP, Bonenkamp JJ, Cuesta MA, Blaisse RJB, Busch ORC, Ten Kate FJW, Creemers GM, Punt CJA, Plukker JTM, Verheul HMW, Bilgen EJS, van Dekken H, van der Sangen MJC, Rozema T, Biermann K, Beukema JC, Piet AHM, van Rij CM, Reinders JG, Tilanus HW, Steyerberg EW, van der Gaast A; CROSS study group. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16(9):1090–98. https://doi.org/10.1016/S1470-2045(15)00040-6.
Ostwal V, Sahu A, Ramaswamy A, Sirohi B, Bose S, Talreja V, Goel M, Patkar S, Desouza A, Shrikhande SV. Perioperative Epirubicin, Oxaliplatin, and Capecitabine Chemotherapy in Locally Advanced Gastric Cancer: Safety and Feasibility in an Interim Survival Analysis. J Gastric Cancer. 2017;17(1):21–32. https://doi.org/10.5230/jgc.2017.17.e3.
Al-Batran SE, Homann N, Pauligk C, Goetze TO, Meiler J, Kasper S, Kopp HG, Mayer F, Haag GM, Luley K, Lindig U, Schmiegel W, Pohl M, Stoehlmacher J, Folprecht G, Probst S, Prasnikar N, Fischbach W, Mahlberg R, Trojan J, Koenigsmann M, Martens UM, Thuss-Patience P, Egger M, Block A, Heinemann V, Illerhaus G, Moehler M, Schenk M, Kullmann F, Behringer DM, Heike M, Pink D, Teschendorf C, Löhr C, Bernhard H, Schuch G, Rethwisch V, von Weikersthal LF, Hartmann JT, Kneba M, Daum S, Schulmann K, Weniger J, Belle S, Gaiser T, Oduncu FS, Güntner M, Hozaeel W, Reichart A, Jäger E, Kraus T, Mönig S, Bechstein WO, Schuler M, Schmalenberg H, Hofheinz RD; FLOT4-AIO Investigators. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393(10184):1948–57. https://doi.org/10.1016/S0140-6736(18)32557-1.
Guidelines for the management of adults with hospital-acquired. ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416.
Low DE, Alderson D, Cecconello I, Chang AC, Darling GE, DʼJourno XB, Griffin SM, Hölscher AH, Hofstetter WL, Jobe BA, Kitagawa Y, Kucharczuk JC, Law SY, Lerut TE, Maynard N, Pera M, Peters JH, Pramesh CS, Reynolds JV, Smithers BM, van Lanschot JJ. International Consensus on Standardization of Data Collection for Complications Associated With Esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg. 2015;262(2):286–94. https://doi.org/10.1097/SLA.0000000000001098.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Fayers P, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A. EORTC QLQ-C30 Scoring Manual. 3rd ed. European Organisation for Research and Treatment of Cancer, Brussel, 2001.
Lagergren P, Fayers P, Conroy T, Stein HJ, Sezer O, Hardwick R, Hammerlid E, Bottomley A, Van Cutsem E, Blazeby JM; European Organisation for Research Treatment of Cancer Gastrointestinal and Quality of Life Groups. Clinical and psychometric validation of a questionnaire module, the EORTC QLQ-OG25, to assess health-related quality of life in patients with cancer of the oesophagus, the oesophago-gastric junction and the stomach. Eur J Cancer. 2007;43(14):2066–73. https://doi.org/10.1016/j.ejca.2007.07.005
Cocks K, King MT, Velikova G, de Castro G Jr, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Eur J Cancer. 2012;48(11):1713–21. https://doi.org/10.1016/j.ejca.2012.02.059.
Markar SR, Zaninotto G, Castoro C, Johar A, Lagergren P, Elliott JA, Gisbertz SS, Mariette C, Alfieri R, Huddy J, Sounderajah V, Pinto E, Scarpa M, Klevebro F, Sunde B, Murphy CF, Greene C, Ravi N, Piessen G, Brenkman H, Ruurda JP, Van Hillegersberg R, Lagarde S, Wijnhoven B, Pera M, Roig J, Castro S, Matthijsen R, Findlay J, Antonowicz S, Maynard N, McCormack O, Ariyarathenam A, Sanders G, Cheong E, Jaunoo S, Allum W, Van Lanschot J, Nilsson M, Reynolds JV, van Berge Henegouwen MI, Hanna GB. Lasting Symptoms After Esophageal Resection (LASER): European Multicenter Cross-sectional Study. Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000003917.
van Heijl M, Gooszen JA, Fockens P, Busch OR, van Lanschot JJ, van Berge Henegouwen MI. Risk factors for development of benign cervical strictures after esophagectomy. Ann Surg. 2010;251(6):1064–69. https://doi.org/10.1097/SLA.0b013e3181deb4b7.
Jezerskyte E, Saadeh LM, Hagens ERC, Sprangers MAG, Noteboom L, van Laarhoven HWM, Eshuis WJ, Hulshof MCCM, van Berge Henegouwen MI, Gisbertz SS. Long-term health-related quality of life after McKeown and Ivor Lewis esophagectomy for esophageal carcinoma. Dis Esophagus. 2020;33(11):doaa022. https://doi.org/10.1093/dote/doaa022.
Acknowledgment
The authors thank all centers in the Netherlands that participated in the NCR and POCOP data collection.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosure
M. I. van Berge Henegouwen has a consultant role with Mylan, Johnson and Johnson, and Medtronic, as well as research funding from Olympus and Stryker. H. W. M. van Laarhoven has a consultant or advisory role with BMS, Lilly, MSD, Merck, Nordic Pharma, Servier, as well as research funding from Bayer, BMS, Celgene, Janssen, Lilly, Merck, Nordic Pharma, Philips, Roche, and Servier. C. Rosman has research funding from Johnson & Johnson and Medtronic. R. van Hillegersberg is a proctor for Intuitive Surgery. The remaining authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jezerskyte, E., van Berge Henegouwen, M.I., van Laarhoven, H.W.M. et al. Postoperative Complications and Long-Term Quality of Life After Multimodality Treatment for Esophageal Cancer: An Analysis of the Prospective Observational Cohort Study of Esophageal-Gastric Cancer Patients (POCOP). Ann Surg Oncol 28, 7259–7276 (2021). https://doi.org/10.1245/s10434-021-10144-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10144-5