Abstract
Purpose
Current evidence suggests that the neutrophil-to-lymphocyte ratio (NLR) is a prognostic factor in several types of cancer. In this study, we aimed to evaluate the prognostic impact of clinicopathological factors, including postoperative NLR, in patients with locally advanced non-small-cell lung cancer (LA-NSCLC) who underwent surgery after chemoradiotherapy (CRT) with or without postoperative adjuvant chemotherapy.
Methods
The medical records of LA-NSCLC patients treated with trimodality therapy at our institution between June 1999 and May 2019 were reviewed. The association between several clinicopathological factors and overall survival (OS) was analyzed.
Results
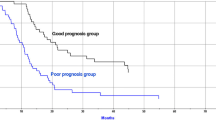
A total of 168 patients were included in this study. Regarding the prognosis, the 5-year OS rate was 68.1%, and the 2-year recurrence-free survival rate was 66.1% in the entire population. In multivariate analysis, we identified that high postoperative NLR, not pretreatment or preoperative NLR, was one of the independent factors for unfavorable OS (NLR high vs NLR low; hazard ratio = 2.45, 95% confidence interval: 1.53–3.94, p < 0.001). In addition, among patients with high postoperative NLR, patients who received postoperative adjuvant chemotherapy showed significantly better 5-year OS compared with those who did not (p = 0.016). On the other hand, postoperative adjuvant chemotherapy had no impact on the prognosis in patients with low NLR (p = 0.19).
Conclusions
Our results suggest that high postoperative NLR was not only an independent unfavorable prognostic factor in patients with LA-NSCLC who were treated with trimodality therapy, but also a promising indicator for postoperative treatment in this population.


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Ferlay J, Colombet M, Soerjomataram I, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356–87.
Stinchcombe TE, Zhang Y, Vokes EE, et al. Pooled analysis of individual patient data on concurrent chemoradiotherapy for stage III non-small-cell lung cancer in elderly patients compared with younger patients who participated in US National Cancer Institute Cooperative Group Studies. J Clin Oncol. 2017;35(25):2885–92.
Paz-Ares L, Luft A, Vicente D, et al. Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med. 2018;379(21):2040–51.
Spira A, Ettinger DS. Multidisciplinary management of lung cancer. N Engl J Med. 2004;350(4):379–92.
Toyooka S, Kiura K, Takemoto M, et al. Long-term outcome of induction chemoradiotherapy with docetaxel and cisplatin followed by surgery for non-small-cell lung cancer with mediastinal lymph node metastasis. Interactive Cardiovasc Thoracic Surg. 2012;14(5):565–9.
Katayama H, Ueoka H, Kiura K, et al. Preoperative concurrent chemoradiotherapy with cisplatin and docetaxel in patients with locally advanced non-small-cell lung cancer. Br J Cancer. 2004;90(5):979–84.
Torigoe H, Soh J, Tomida S, et al. Induction chemoradiotherapy using docetaxel and cisplatin with definitive-dose radiation followed by surgery for locally advanced non-small cell lung cancer. J Thorac Dis. 2017;9(9):3076–86.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Peng F, Hu D, Lin X, et al. The monocyte to red blood cell count ratio is a strong predictor of postoperative survival in colorectal cancer patients: the Fujian prospective investigation of cancer (FIESTA) study. J Cancer. 2017;8(6):967–75.
Zou ZY, Liu HL, Ning N, Li SY, Du XH, Li R. Clinical significance of pre-operative neutrophil lymphocyte ratio and platelet lymphocyte ratio as prognostic factors for patients with colorectal cancer. Oncol Lett. 2016;11(3):2241–8.
Gu XB, Tian T, Tian XJ, Zhang XJ. Prognostic significance of neutrophil-to-lymphocyte ratio in non-small cell lung cancer: a meta-analysis. Sci Rep. 2015;5:12493.
Templeton AJ, McNamara MG, Šeruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):111124.
Luo G, Guo M, Liu Z, et al. Blood neutrophil-lymphocyte ratio predicts survival in patients with advanced pancreatic cancer treated with chemotherapy. Ann Surg Oncol. 2015;22(2):670–6.
Yamamoto H, Namba K, Yamamoto H, et al. The neutrophil-to-lymphocyte ratio as a novel independent prognostic factor for multiple metastatic lung tumors from various sarcomas. Surg Today. 2021;51:127–35.
Guo D, Han A, Jing W, et al. Preoperative to postoperative change in neutrophil-to-lymphocyte ratio predicts survival in colorectal cancer patients. Future Oncol. 2018;14(12):1187–96.
Jin F, Han A, Shi F, Kong L, Yu J. The postoperative neutrophil-to-lymphocyte ratio and changes in this ratio predict survival after the complete resection of stage I non-small cell lung cancer. Onco Targets Ther. 2016;9:6529–37.
Goldstraw P, Chansky K, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol. 2016;11(1):39–51.
Yokomise H, Gotoh M, Okamoto T, et al. Induction chemoradiotherapy (carboplatin-taxane and concurrent 50-Gy radiation) for bulky cN2, N3 non-small cell lung cancer. J Thoracic Cardiovasc Surg. 2007;133(5):1179–85.
Kanda Y, Kanda J, Atsuta Y, et al. Impact of a single human leucocyte antigen (HLA) allele mismatch on the outcome of unrelated bone marrow transplantation over two time periods. A retrospective analysis of 3003 patients from the HLA Working Group of the Japan Society for Blood and Marrow Transplantation. Br J Haematol. 2013;161(4):566–77.
Pataer A, Kalhor N, Correa AM, et al. Histopathologic response criteria predict survival of patients with resected lung cancer after neoadjuvant chemotherapy. J Thorac Oncol. 2012;7(5):825–32.
Zahorec R. Ratio of neutrophil to lymphocyte counts—rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102(1):5–14.
Zhang H, Xia H, Zhang L, Zhang B, Yue D, Wang C. Clinical significance of preoperative neutrophil-lymphocyte vs platelet-lymphocyte ratio in primary operable patients with non-small cell lung cancer. Am J Surg. 2015;210(3):526–35.
Hu P, Shen H, Wang G, Zhang P, Liu Q, Du J. Prognostic significance of systemic inflammation-based lymphocyte-monocyte ratio in patients with lung cancer: based on a large cohort study. PLoS ONE. 2014;9(9):e108062.
Ishikawa D, Nishi M, Takasu C, et al. The role of neutrophil-to-lymphocyte ratio on the effect of CRT for patients with rectal cancer. In Vivo. 2020;34(2):863–8.
Li C, Wen TF, Yan LN, et al. Postoperative neutrophil-to-lymphocyte ratio plus platelet-to-lymphocyte ratio predicts the outcomes of hepatocellular carcinoma. J Surg Res. 2015;198(1):73–9.
Josa V, Krzystanek M, Eklund AC, et al. Relationship of postoperative thrombocytosis and survival of patients with colorectal cancer. Int J Surg. 2015;18:1–6.
Van Berckelaer C, Van Geyt M, Linders S, et al. A high neutrophil-lymphocyte ratio and platelet-lymphocyte ratio are associated with a worse outcome in inflammatory breast cancer. Breast. 2020;53:212–20.
Mouchli M, Reddy S, Gerrard M, Boardman L, Rubio M. Usefulness of Neutrophil-to-Lymphocyte Ratio (NLR) as a prognostic predictor after treatment of hepatocellular carcinoma. Review article. Ann Hepatol. 2020;22:100249.
Shin S, Kim HK, Cho JH, et al. Adjuvant therapy in stage IIIA-N2 non-small cell lung cancer after neoadjuvant concurrent chemoradiotherapy followed by surgery. J Thorac Dis. 2020;12(5):2602–13.
Acknowledgement
This work was supported by a Management Expenses Grant for National University Corporations in Japan. We would like to thank Editage (http://www.editage.com) for English language editing.
Funding
This work was supported by a Management Expenses Grant for National University Corporations in Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Katsuyuki Kiura; Ono Pharmaceutical Co., Ltd.; Boehringer Ingelheim Co., Ltd.; Taiho Pharmaceutical Co., Ltd.; Chugai Pharmaceutical Co., Ltd.; Nippon Kayaku Co., Ltd.; Bristol-Myers Squibb K.K.; MSD K.K.; Pfizer Japan Inc.; TEIJIN Pharma Limited.; KYORIN Pharmaceutical Co., Ltd.; Merck Biopharma Co., Ltd.; Daiichi Sankyo Co., Ltd.; SHIONOGI & Co., Ltd.; Takeda Pharmaceutical Co., Ltd.; AstraZeneca K.K.; Eli Lilly Japan K.K.; Novartis International AG.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10434_2021_9690_MOESM2_ESM.tif
Supplementary Fig. 1. ROC curves to determine the cutoff value for pretreatment, preoperative and postoperative NLR (TIF 512 kb)
10434_2021_9690_MOESM3_ESM.tif
Supplementary Fig. 2. Overall survival (OS) stratified by the completion of postoperative adjuvant chemotherapy in the high postoperative NLR (≥ 4.06) group of patients who underwent postoperative adjuvant chemotherapy (TIF 410 kb)
Rights and permissions
About this article
Cite this article
Tsudaka, S., Yamamoto, H., Sato, H. et al. Prognostic Significance of Neutrophil-to-Lymphocyte Ratio in Locally Advanced Non-small-cell Lung Cancer Treated with Trimodality Therapy. Ann Surg Oncol 28, 4880–4890 (2021). https://doi.org/10.1245/s10434-021-09690-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09690-9