Abstract
Background
The purpose of this study was to evaluate the impact of ipsilateral supraclavicular lymph node dissection (ISLND) on the outcomes of breast cancer patients with ipsilateral supraclavicular lymph node metastasis (ISLNM), and to evaluate the prognostic value of ipsilateral supraclavicular pathological complete response (ispCR). Meanwhile, a nomogram was constructed to predict ispCR.
Methods
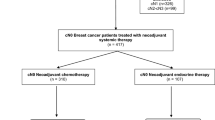
We retrospectively reviewed the medical documents of 353 patients with ISLNM but no distant metastasis at presentation. Based on whether ISLND was performed, patients were divided into radiotherapy (RT) and ISLND + RT groups. The impact of ISLND was evaluated after propensity score matching, and the prognostic value of ispCR was also analyzed. A nomogram to predict the probability of ispCR was constructed based on clinicopathologic variables.
Results
After propensity score matching, we found that the use of ISLND was associated with a higher rate of ipsilateral supraclavicular relapse-free survival (ISRFS; p < 0.0001). Among 307 patients who underwent ISLND, ispCR was associated with a higher rate of ISRFS and disease-free survival (p = 0.018 and p = 0.00033, respectively). Furthermore, the nomogram constructed with number of axillary lymph node metastases, breast pCR, size of the ipsilateral supraclavicular lymph nodes after neoadjuvant chemotherapy (NAC), number of NAC cycles, and Ki67 level showed a good fit for predicting ispCR.
Conclusion
For breast cancer patients with ISLNM but no distant metastasis, ISLND may be beneficial in some certain subtypes, and ispCR indicated a better prognosis. Our nomogram is well-fitted to predict the probability of achieving ispCR.




Similar content being viewed by others
Change history
18 March 2021
A Correction to this paper has been published: https://doi.org/10.1245/s10434-021-09841-y
References
Ai X, Wang M, Li J, et al. Supraclavicular lymph node dissection with radiotherapy versus radiotherapy alone for operable breast cancer with synchronous ipsilateral supraclavicular lymph node metastases: a real-world cohort study. Gland Surg. 2020;9(2):329–41.
Fleming ID, Cooper JS, Henson DE, Hutter RVP, Kennedy BJ, Murphy GP, et al., editors. American Joint Committee on Cancer. Manual for staging of cancer. 5th edition. Philadelphia: JB Lippincott; 1997.
Brito RA, Valero V, Buzdar AU, et al. Long-term results of combined-modality therapy for locally advanced breast cancer with ipsilateral supraclavicular metastases: The University of Texas M.D. Anderson Cancer Center experience. J Clin Oncol. 2001;19(3):628–33.
Greene FL, Page DL, Fleming ID, et al., editors. AJCC cancer staging manual. 6th ed. New York: Springer; 2002.
Singletary SE, Allred C, Ashley P, et al. Revision of the American Joint Committee on Cancer staging system for breast cancer. J Clin Oncol. 2002;20(17):3628–36.
Fisher B, Brown A, Mamounas E, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997;15(7):2483–93.
Buzdar AU, Ibrahim NK, Francis D, et al. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol. 2005;23(16):3676–85.
Hennessy BT, Hortobagyi GN, Rouzier R, et al. Outcome after pathologic complete eradication of cytologically proven breast cancer axillary node metastases following primary chemotherapy. J Clin Oncol. 2005;23(36):9304–11.
Dominici LS, Negron Gonzalez VM, Buzdar AU, et al. Cytologically proven axillary lymph node metastases are eradicated in patients receiving preoperative chemotherapy with concurrent trastuzumab for HER2-positive breast cancer. Cancer 2010;116(12):2884–9.
Jin X, Jiang YZ, Chen S, Shao ZM, Di GH. A nomogram for predicting the pathological response of axillary lymph node metastasis in breast cancer patients. Sci Rep. 2016;6:32585.
Choi HJ, Ryu JM, Kim I, et al. Nomogram for accurate prediction of breast and axillary pathologic response after neoadjuvant chemotherapy in node positive patients with breast cancer. Ann Surg Treat Res. 2019;96(4):169–76.
Vila J, Mittendorf EA, Farante G, et al. Nomograms for predicting axillary response to neoadjuvant chemotherapy in clinically node-positive patients with breast cancer. Ann Surg Oncol. 2016;23(11):3501–9.
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 2002;41(3A):154–61.
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32.
Bisase B, Kerawala C. Survey of UK practice for management of breast cancer metastases to the neck. Ann R Coll Surg Engl. 2012;94(7):484–9.
Jung J, Kim SS, Ahn SD, et al. Treatment outcome of breast cancer with pathologically proven synchronous ipsilateral supraclavicular lymph node metastases. J Breast Cancer. 2015;18(2):167–72.
Olivotto IA, Chua B, Allan SJ, Speers CH, Chia S, Ragaz J. Long-term survival of patients with supraclavicular metastases at diagnosis of breast cancer. J Clin Oncol. 2003;21(5):851–4.
Huang EH, Strom EA, Valero V, et al. Locoregional treatment outcomes for breast cancer patients with ipsilateral supraclavicular metastases at diagnosis. Int J Radiat Oncol Biol Phys. 2007;67(2):490–6.
National Bureau of Statistics of the People’s Republic of China. China Statistical Yearbook. Beijing: China Statistics Press; 2020.
Ellis H, Colborn GL, Skandalakis JE. Surgical embryology and anatomy of the breast and its related anatomic structures. Surg Clin North Am. 1993;73(4):611–32.
Skandalakis LJ, Vohman MD, Skandalakis JE, Gray SW. The axillary lymph nodes in radical and modified radical mastectomy. Am Surg. 1979;45(9):552–5.
Veronesi U, Luini A, Galimberti V, Marchini S, Sacchini V, Rilke F. Extent of metastatic axillary involvement in 1446 cases of breast cancer. Eur J Surg Oncol. 1990;16(2):127–33.
Nathanson SD, Wachna DL, Gilman D, Karvelis K, Havstad S, Ferrara J. Pathways of lymphatic drainage from the breast. Ann Surg Oncol. 2001;8(10):837–43.
Fan Y, Xu B, Liao Y, Yao S, Sun Y. A retrospective study of metachronous and synchronous ipsilateral supraclavicular lymph node metastases in breast cancer patients. Breast 2010;19(5):365–9.
Berruti A, Amoroso V, Gallo F, et al. Pathologic complete response as a potential surrogate for the clinical outcome in patients with breast cancer after neoadjuvant therapy: a meta-regression of 29 randomized prospective studies. J Clin Oncol. 2014;32(34):3883–91.
Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 2014;384(9938):164–72.
Zhu J, Jiao D, Guo X, et al. Predictive factors and prognostic value of pathologic complete response of ipsilateral supraclavicular lymph nodes in breast cancer after neoadjuvant chemotherapy. Ann Transl Med. 2019;7(22):666.
Acknowledgment
This study was supported by the Science and Technology Development Plan of He’nan (Grant No. 202102310428).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Minhao Lv, Juntao Li, Huihui Guo, Chao Wang, Peiqi Tian, Youzhao Ma, Xiuchun Chen, and Suxia Luo declare no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of the article has been revised due to a retrospective open access cancellation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2020_9548_MOESM2_ESM.jpg
SUPPLEMENTARY FIG. S1 Kaplan–Meier curves for (a) ipsilateral supraclavicular relapse-free survival (ISRFS), (b) disease-free survival (DFS), and (c) overall survival (OS) with the ISLND + RT versus RT groups in propensity score-matched patients with luminal A and B subtypes. ISLND ipsilateral supraclavicular lymph node dissection, RT radiotherapy (JPEG 610 kb)
10434_2020_9548_MOESM3_ESM.jpg
SUPPLEMENTARY FIG. S2 Kaplan–Meier curves for (a) ipsilateral supraclavicular relapse-free survival (ISRFS), (b) disease-free survival (DFS), and (c) overall survival (OS) with the ISLND + RT versus RT groups in propensity score-matched patients with luminal-HER2, HER2+, and triple-negative subtypes. ISLND ipsilateral supraclavicular lymph node dissection, RT radiotherapy (JPEG 613 kb)
10434_2020_9548_MOESM4_ESM.jpg
SUPPLEMENTARY FIG. S3 Calibration plot of the nomogram for the probability of ipsilateral supraclavicular pathological complete response (ispCR) (bootstrap 1000 repetitions) (JPEG 252 kb)
Rights and permissions
About this article
Cite this article
Lv, M., Li, J., Guo, H. et al. Impact of Ipsilateral Supraclavicular Lymph Node Dissection (ISLND) for Breast Cancer Patients and a Nomogram for Predicting Ipsilateral Supraclavicular Pathological Complete Response (ispCR). Ann Surg Oncol 28, 5098–5109 (2021). https://doi.org/10.1245/s10434-020-09548-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09548-6