Abstract
Background
Breast core needle biopsy (CNB) can obviate the need for breast surgery in patients with an unknown breast lesion; however, variation in compliance with this guideline may represent a disparity in health care and a surrogate measure of unnecessary surgery. We evaluated variation in breast CNB rates prior to initial breast cancer surgery.
Methods
We performed a retrospective analysis using Medicare claims from 2015 to 2017 to evaluate the proportion of patients who received a CNB within 6 months prior to initial breast cancer surgery. Outlier practice pattern was defined as a preoperative CNB rate ≤ 70%. Logistic regression was used to evaluate surgeon characteristics associated with outlier practice pattern.
Results
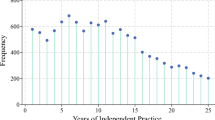
We identified 108,935 female patients who underwent initial breast cancer surgery performed by 3229 surgeons from July 2015 to June 2017. The mean CNB rate was 86.7%. A total of 7.7% of surgeons had a CNB performed prior to initial breast surgery ≤ 70% of the time, and 2.0% had a CNB performed ≤ 50% of the time. Outlier breast surgeons were associated with practicing in a micropolitan area (odds ratio [OR] 1.88, 95% confidence interval [CI] 1.29–2.73), in the South (OR 1.84, 95% CI 1.20–2.84) or West region (OR 1.78, 95% CI 1.11–2.86), > 20 years in practice (OR 1.52, 95% CI 1.09–2.11), and low breast cancer surgery volume (< 30 cases in the study period; OR 4.03, 95% CI 2.75–5.90).
Conclusions
Marked variation exists in whether a breast core biopsy is performed prior to initial breast surgery, which may represent unnecessary surgery on individual patients. Providing surgeon-specific feedback on guideline compliance may reduce unwarranted variation.


Similar content being viewed by others
References
Bevers TB, Anderson BO, Bonaccio E, et al. Breast cancer screening and diagnosis: Clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2009;7(10):1060–96. https://doi.org/10.6004/jnccn.2009.0070.
Silverstein MJ, Lagios MD, Recht A, et al. Image-Detected Breast Cancer: State of the Art Diagnosis and Treatment. J Am Coll Surg. 2005;201(4):586-597. https://doi.org/10.1016/j.jamcollsurg.2005.05.032.
nBx – Breast measure: Image or palpation-guided needle biopsy to the primary site is performed to establish diagnosis of breast cancer. 2019. Available at: https://www.facs.org/~/media/files/quality programs/cancer/ncdb/measure specs breast.ashx. Accessed 9 Jul 2020.
NAPBC Standards Manual 2014 Edition. Available at: https://www.facs.org/~/media/files/quality%20programs/napbc/2014%20napbc%20standards%20manual.ashx. Accessed 12 Jul 2018.
Commission on Cancer: Five Things Physicians and Patients Should Question. Choosing Wisely. Available at: https://www.choosingwisely.org/societies/commission-on-cancer/. Published 2013. Accessed 9 Jul 2020.
Centers for Medicare and Medicaid Services. Physician compare national downloadable file. https://data.medicare.gov/Physician-Compare/Physician-Compare-National-Downloadable-File/mj5m-pzi6. Updated 2018. Accessed 7 Nov 2018.
Centers for Medicare and Medicaid Services. Medicare data on provider practice and specialty (MD-PPAS) user documentation version 2.2. Updated 2017. Available at: https://resdac.umn.edu/sites/resdac.umn.edu/files/MD-PPAS%20User%20Documentation%20-%20Version%202.2.docx.
United States Census Bureau. Geographic Terms and Concepts-Core Based Statistical Areas and Related Statistical Areas. Available at: https://www.census.gov/geo/reference/gtc/gtc_cbsa.html.
Society of Surgical Oncology. SSO-Approved Breast Oncology Fellowship Training Programs. Rosemont, IL: Society of Surgical Oncology.
ACGME. Complex General Surgical Oncology Programs Academic Year 2017–2018 United States. Available at: https://www.surgonc.org/fellows/surgical-oncology-fellowships/program-list/. Accessed 8 Jan 2017.
The New York Times. Breast Biopsies Leave Room for Doubt, Study Finds. Available at: https://www.nytimes.com/2015/03/18/health/breast-biopsies-dcis-atypia-diagnosis-leave-room-for-doubt.html. Accessed 4 Oct 2018.
Healthcare Bluebook. Available at: https://www.healthcarebluebook.com/ui/consumerfront. Accessed 4 Jun 2017.
Dahabreh IJ, Wieland LS, Adam GP, Halladay C, Lau J TT. Core Needle and Open Surgical Biopsy for Diagnosis of Breast Lesions: An Update to the 2009 Report. Comp Eff Rev No. 139. 2014: AHRQ Publication No. 14-EHC040-EF. Available at: https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/breast-biopsy-update_research.pdf.
Holloway CMB, Saskin R, Paszat L. Geographic variation and physician specialization in the use of percutaneous biopsy for breast cancer diagnosis. Can J Surg. 2008;51(6):453–463.
Williams RT, Yao K, Stewart AK, et al. Needle versus excisional biopsy for noninvasive and invasive breast cancer: report from the national cancer data base, 2003–2008. Ann Surg Oncol. 2011;18(13):3802–3810. https://doi.org/10.1245/s10434-011-1808-y.
Medicare.gov Part B costs. Available at: https://www.medicare.gov/your-medicare-costs/part-b-costs/part-b-costs.html.
Breslin TM, Caughran J, Pettinga J, et al. Improving breast cancer care through a regional quality collaborative. Surgery. 2011;150(4):635–642. http://dx.doi.org/10.1016/j.surg.2011.07.071.
Navathe AS, Emanuel EJ. Physician peer comparisons as a nonfinancial strategy to improve the value of care. JAMA. 2016;316(17):1759–1760. https://doi.org/10.1001/jama.2016.13739.
Acknowledgments
None.
Funding
Funding for this work was provided by the Division of Surgical Oncology, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA, and the Robert Wood Johnson Foundation at Johns Hopkins University.
Author information
Authors and Affiliations
Contributions
Study conception and design: RCG, KK, MAM, DME. Acquisition of data: PW, SH, KK. Analysis and interpretation of data: PW, SH, RCG, MAM, DME. Drafting of the manuscript: RCG, PW. Critical revision: MAM, DME, LKJ, MH, JL, MC.
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gilmore, R.C., Wang, P., Kaczmarski, K. et al. Underutilization of Needle Biopsy Before Breast Surgery: A Measure of Low-Value Care. Ann Surg Oncol 28, 2485–2492 (2021). https://doi.org/10.1245/s10434-020-09340-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09340-6