Abstract
Background
Sentinel lymph node (SLN) surgery after neoadjuvant chemotherapy (NAC) has been well studied. However, outcomes data addressing the oncologic safety of this technique are sparse. This study aimed to evaluate use of SLN surgery versus axillary lymph node dissection (ALND) for clinically node-positive patients treated with NAC and to report outcomes.
Methods
The study identified patients at the authors’ institution with biopsy proven clinically node-positive (cN1–cN3) breast cancer undergoing axillary surgery after NAC from 2009 to 2019. Practice patterns and outcomes were evaluated.
Results
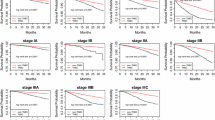
Of 602 patients, 52.3% underwent SLN surgery. Use of SLN surgery increased significantly over time, reaching 75.3% during 2015–2019. For 52.5% of the patients who had an SLN identified, ALND was not used. Use of ALND (± SLN surgery) decreased from 100% in 2009 to 57.2% in 2015–2019. The nodal positivity rate of patients who proceeded directly to ALND was 64.5% (185/287), increasing significantly over time. Factors significantly associated with performing SLN surgery on multivariable analysis were lower presenting clinical T category, lower presenting clinical N category (cN1 vs cN2–3) and HER2-positive status. During the median 34-month follow-up period, 17 regional recurrences were observed (16/443 with ALND; 1/159 with SLN surgery alone), for a 2-year freedom-from-regional-recurrence rate of 99.1% among the SLN surgery patients and 96.4% among the ALND patients (p = 0.10).
Conclusions
For cN1–3 breast cancer treated with NAC, SLN surgery has been incorporated into clinical practice at the authors’ institution. In this study, selection for SLN surgery was based on clinical factors and tumor biology. More than half of the patients who were selected for SLN surgery were spared ALND, with a low nodal failure rate and no recurrence-free survival disadvantage at 2 years.



Similar content being viewed by others
References
Giuliano AE, Kirgan DM, Guenther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994;220:391–8. (discussion 398–401).
Krag DN, Andeson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary lymph node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927–33.
Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569–75.
Pathak M, Deo SVS, Nand Dwivedi S, Sreenivas V, Thakur B, Kumar Julka P, Rath GK. Role of neoadjuvant chemotherapy in breast cancer patients: systematic review and meta-analysis. Indian J Med Paediatr Oncol. 2019;40:48.
Boughey JC, Suman VJ, Mittendorf EA, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310:1455–61.
Kuehn T, Bauerfeind I, Fehm T, et al. Sentinel lymph node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol. 2013;14:609–18.
Boileau JF, Poirier B, Basik M, et al. Sentinel node biopsy after neoadjuvant chemotherapy in biopsy-proven node-positive breast cancer: the SN FNAC study. J Clin Oncol. 2015;33:258–64.
Krag DN, Anderson SJ, Julian TB, et al. Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III TRIAL. Lancet Oncol. 2007;8:881–8.
Nguyen TT, Hoskin TL, Day CN, Degnim AC, Jakub JW, Hieken TJ, Boughey JC. Decreasing use of axillary dissection in node-positive breast cancer patients treated with neoadjuvant chemotherapy. Ann Surg Oncol. 2018;25:2596–602.
Caudle AS, Bedrosian I, Milton DR, DeSnyder SM, Kuerer HM, Hunt KK, Mittendorf EA. Use of sentinel lymph node dissection after neoadjuvant chemotherapy in patients with node-positive breast cancer at diagnosis: practice patterns of American Society of Breast Surgeons members. Ann Surg Oncol. 2017;24:2925–34.
Wilke LG, et al. Consensus Guidelines on the Management of the Axilla in Patients with Invasive In Situ Breast Cancer. American Society of Breast Surgeons. 2019. https://www.breastsurgeons.org/docs/statements/Consensus-Guideline-on-the-Management-of-the-Axilla.pdf?v2. Accessed 24 June 2020.
Schijven MP, Vingerhoets AJJM, Rutten HJT, Nieuwenhuijzen GAP, Roumen RMH, van Bussel ME, Voogd AC. Comparison of morbidity between axillary lymph node dissection and sentinel node biopsy. Eur J Surg Oncol. 2003;29:341–50.
Schrenk P, Rieger R, Shamiyeh A, Wayand W. Morbidity following sentinel lymph node biopsy versus axillary lymph node dissection for patients with breast carcinoma. Cancer. 2000;88:608–14.
Gregorowitsch,ML, Verkooijen HM, Houweling A, et al. Impact of modern-day axillary treatment on patient reported arm morbidity and physical functioning in breast cancer patients. Radiother Oncol. 2019;131:221–8.
Esserman LJ, Berry DA, DeMichele A, et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 trial–CALGB 150007/150012, ACRIN 6657. J Clin Oncol. 2012;30:3242–9.
Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Boughey J, Ballman KV, McCall LM, et al. Tumor biology and response to chemotherapy impact breast cancer-specific survival in node-positive breast cancer patients treated with neoadjuvant chemotherapy: long-term follow-up from ACOSOG Z1071 (Alliance). Ann Surg. 2017;266:667–76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Piltin, M.A., Hoskin, T.L., Day, C.N. et al. Oncologic Outcomes of Sentinel Lymph Node Surgery After Neoadjuvant Chemotherapy for Node-Positive Breast Cancer. Ann Surg Oncol 27, 4795–4801 (2020). https://doi.org/10.1245/s10434-020-08900-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08900-0