Abstract
Background
The authors hypothesized that in resected pancreatic adenocarcinoma (PDAC), pathologic characteristics, oncologic outcomes, prognostic factors, and the accuracy of the American Joint Committee on Cancer (AJCC) staging system might differ based on tumor location.
Methods
Patients undergoing pancreatectomy for PDAC at two academic institutions from 2000 to 2015 were retrieved. A comparative analysis between head (H-PDAC) and body–tail (BT-PDAC) tumors was performed using uni- and multivariable models. The accuracy of the eighth AJCC staging system was analyzed using C-statistics.
Results
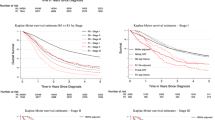
Among 1466 patients, 264 (18%) had BT-PDAC, which displayed greater tumor size but significantly lower rates of perineural invasion and G3/4 grading. Furthermore, BT-PDAC was associated with a lower frequency of nodal involvement and a greater representation of earlier stages. The recurrence-free survival and disease-specific survival times were longer for BT-PDAC (16 vs 14 months [p = 0.020] and 33 vs 26 months [p = 0.026], respectively), but tumor location was not an independent predictor of recurrence or survival in the multivariable analyses. The recurrence patterns did not differ. Certain prognostic factors (i.e., CA 19.9, grading, R-status, and adjuvant treatment) were common, whereas others were site-specific (i.e., preoperative pain, diabetes, and multivisceral resection). The performances of the AJCC staging system were similar (C-statistics of 0.573 for H-PDAC and 0.597 for BT-PDAC, respectively).
Conclusions
Despite differences in pathologic profile found to be in favor of BT-PDAC, tumor location was not an independent predictor of recurrence or survival after pancreatectomy. An array of site-specific prognostic factors was identified, but the AJCC staging system displayed similar prognostic power regardless of primary tumor location.

Similar content being viewed by others
References
Allen PJ, Kuk D, Castillo CF, et al. Multi-institutional validation study of the American Joint Commission on Cancer (8th edition) changes for T and N staging in patients with pancreatic adenocarcinoma. Ann Surg. 2017;265:185–91.
Kamarajah SK, Burns WR, Frankel TL, et al. Validation of the American Joint Commission on Cancer (AJCC) 8th-edition staging system for patients with pancreatic adenocarcinoma: a surveillance, epidemiology and end results (SEER) analysis. Ann Surg Oncol. 2017;24:2023–30.
van Roessel S, Kasumova GG, Verheij J, et al. International validation of the eighth edition of the American Joint Committee on Cancer (AJCC) TNM staging system in patients with resected pancreatic cancer. JAMA Surg. 2018;153:e183617.
Schlitter AM, Jesinghaus M, Jäger C, et al. pT but not pN stage of the 8th TNM classification significantly improves prognostication in pancreatic ductal adenocarcinoma. Eur J Cancer. 2017;84:121–9.
Tempero MA, et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) for Pancreatic Adenocarcinoma V.1.2020. © 2020 National Comprehensive Cancer Network, Inc. Available at https://www.nccn.org/. Accessed 15 Apr 2020.
Kanda M, Fujii T, Nagai S, et al. Pattern of lymph node metastasis spread in pancreatic cancer. Pancreas. 2011;40:951–5.
Kayahara M, Nagakawa T, Futagami F, et al. Lymphatic flow and neural plexus invasion associated with carcinoma of the body and tail of the pancreas. Cancer. 1996;78:2485–91.
Makino I, Kitagawa H, Ohta T, et al. Nerve plexus invasion in pancreatic cancer: spread patterns on histopathologic and embryological analyses. Pancreas. 2008;37:358–65.
Hartwig W, Vollmer CM, Fingerhut A, et al. Extended pancreatectomy in pancreatic ductal adenocarcinoma: definition and consensus of the International Study Group for Pancreatic Surgery (ISGPS). Surgery. 2014;156:1–14.
Sener SF, Fremgen A, Menck HR, Winchester DP. Pancreatic cancer: a report of treatment and survival trends for 100,313 patients diagnosed from 1985–1995, using the National Cancer Database. J Am Coll Surg. 1999;189:1–7.
Lau MK, Davila JA, Shaib YH. Incidence and survival of pancreatic head and body and tail cancers: a population-based study in the United States. Pancreas. 2010;39:458–62.
Mackay TM, van Erning FN, van der Geest LGM, et al. Association between primary origin (head, body, and tail) of metastasised pancreatic ductal adenocarcinoma and oncologic outcome: a population-based analysis. Eur J Cancer. 2019;106:99–105.
van Erning FN, Mackay TM, van der Geest LGM, et al. Association of the location of pancreatic ductal adenocarcinoma (head, body, tail) with tumor stage, treatment, and survival: a population-based analysis. Acta Oncol. 2018;57:1655–62.
Ryan DP, Hong TS, Bardeesy N. Pancreatic adenocarcinoma. N Engl J Med. 2014;371:1039–49.
Sohn TA, Yeo CJ, Cameron JL, et al. Resected adenocarcinoma of the pancreas-616 patients: results, outcomes, and prognostic indicators. J Gastrointest Surg. 2000;4:567–79.
Artinyan A, Soriano PA, Prendergast C, et al. The anatomic location of pancreatic cancer is a prognostic factor for survival. HPB. 2008;10:371–6.
Dreyer SB, Jamieson NB, Upstill-Goddard R, et al. Defining the molecular pathology of pancreatic body and tail adenocarcinoma. Br J Surg. 2018;105:e183–91.
Winer LK, Dhar VK, Wima K, et al. The Impact of tumor location on resection and survival for pancreatic ductal adenocarcinoma. J Surg Res. 2019;239:60–6.
Tomasello G, Ghidini M, Costanzo A, et al. Outcome of head compared to body and tail pancreatic cancer: a systematic review and meta-analysis of 93 studies. J Gastrointest Oncol. 2019;10:259–69.
Toomey P, Hernandez J, Golkar F, et al. Pancreatic adenocarcinoma: complete tumor extirpation improves survival benefit despite larger tumors for patients who undergo distal pancreatectomy and splenectomy. J Gastrointest Surg. 2012;16:376–81.
Ruess DA, Makowiec F, Chikhladze S, et al. The prognostic influence of intrapancreatic tumor location on survival after resection of pancreatic ductal adenocarcinoma. BMC Surg. 2015;15:123.
Amin, MB, Edge S, Greene, F, et al. AJCC cancer staging manual. 8th ed. Berlin: Springer; 2017.
Malleo G, Maggino L, Marchegiani G, et al. Pancreatectomy with venous resection for pT3 head adenocarcinoma: perioperative outcomes, recurrence pattern, and prognostic implications of histologically confirmed vascular infiltration. Pancreatology. 2017;17:847–57.
Tol JAMG, Gouma DJ, Bassi C, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery. 2014;156:591–600.
Malleo G, Maggino L, Capelli P, et al. Reappraisal of nodal staging and study of lymph node station involvement in pancreaticoduodenectomy with the Standard International Study Group of Pancreatic Surgery definition of lymphadenectomy for cancer. J Am Coll Surg. 2015;221:367–79.e4.
Fernández-Cruz L, Johnson C, Dervenis C. Locoregional dissemination and extended lymphadenectomy in pancreatic cancer. Dig Surg. 1999;16:313–9.
Malleo G, Maggino L, Ferrone CR, et al. Number of examined lymph nodes and nodal status assessment in distal pancreatectomy for body/tail ductal adenocarcinoma. Ann Surg. 2019;270:1138–46.
Ling Q, Xu X, Zheng SS, Kalthoff H. The diversity between pancreatic head and body/tail cancers: clinical parameters and in vitro models. Hepatobil Pancreat Dis Int. 2013;12:480–87.
Court CM, Ankeny JS, Sho S, et al. Circulating tumor cells predict occult metastatic disease and prognosis in pancreatic cancer. Ann Surg Oncol. 2018;25:1000–8.
Sohal DPS, Tullio K, Khorana AA. Do patients with pancreatic body or tail cancer benefit from adjuvant therapy? A cohort study. Surg Oncol. 2018;27:245–50.
Shi S, Hua J, Liang C, et al. Proposed modification of the 8th edition of the AJCC staging system for pancreatic ductal adenocarcinoma. Ann Surg. 2019;269:944–950.
Chen YT, Huang ZP, Zhou ZW, et al. Equipping the American Joint Committee on Cancer staging for resectable pancreatic ductal adenocarcinoma with tumor grade: a recursive partitioning analysis. Med Oncol. 2016;33:122.
Jiang Y, Su Y, Chen Y, et al. Refining the American Joint Committee on Cancer staging scheme for resectable pancreatic ductal adenocarcinoma using recursive partitioning analysis. J Cancer. 2017;8:2765–73.
Roland CL, Yang AD, Katz MHG, et al. Neoadjuvant therapy is associated with a reduced lymph node ratio in patients with potentially resectable pancreatic cancer. Ann Surg Oncol. 2015;22:1168–75.
Michelakos T, Pergolini I, Castillo CF, et al. Predictors of resectability and survival in patients with borderline and locally advanced pancreatic cancer who underwent neoadjuvant treatment with FOLFIRINOX. Ann Surg. 2019;269:733–40.
Mokdad AA, Minter RM, Zhu H, et al. Neoadjuvant therapy followed by resection versus upfront resection for resectable pancreatic cancer: a propensity score-matched analysis. J Clin Oncol. 2017;35:515–22.
Hirono S, Kawai M, Okada K, et al. Pancreatic neck cancer has specific and oncologic characteristics regarding portal vein invasion and lymph node metastasis. Surgery. 2016;159:426–40.
Acknowledgements
This study was funded by the Associazione Italiana per la Ricerca sul Cancro (AIRC 5x1000 n. 12182).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Motaz Qadan was paid consulting fee by Olympus. The remaining authors had no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Malleo, G., Maggino, L., Ferrone, C.R. et al. Does Site Matter? Impact of Tumor Location on Pathologic Characteristics, Recurrence, and Survival of Resected Pancreatic Ductal Adenocarcinoma. Ann Surg Oncol 27, 3898–3912 (2020). https://doi.org/10.1245/s10434-020-08354-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08354-4