Abstract
Background
Recently, it was reported that minimally invasive surgery (MIS) has a negative impact on early-stage cervical cancer (ECC) patient survival. At the same time, advantages of MIS regarding quality of life and low rate of intra- and postoperative complications are well known. Therefore, it is essential to select patients who may benefit from MIS without worsening their oncologic outcomes. The aim of this study is to investigate which pathological factors could guide surgeons’ choice about the best approach in ECC.
Patients and Methods
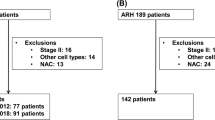
Patients with 2009 FIGO stage from IA1 with lymphovascular space invasion (LVSI) to IB1/IIA1 treated by open or laparoscopic surgery were judged eligible for the study. Disease-free survivals (DFS) of both approaches were tested in subgroups, defined according to histology, tumor size, grading, LVSI, parametrial involvement, and nodal status.
Results
A total of 423 patients were enrolled (217 in the open and 206 in the laparoscopic group). No difference between open surgery and laparoscopy was found among subgroups defined according to histology, grading, LVSI, parametrial involvement, or nodal status. Among patients with tumor > 20 mm, laparoscopy showed a significantly higher relapse risk [hazard ratio (HR): 2.103, p = 0.030]. Among patients with tumor < 20 mm, laparoscopy showed DFS superimposable to open surgery (HR: 0.560, p = 0.128).
Conclusions
Tumor size of 20 mm appeared as the only independent discrimination criterion in patients whose prognosis is affected by surgical approaches.



Similar content being viewed by others
References
Bansal N, Herzog TJ, Shaw RE, et al. Primary therapy for early-stage cervical cancer: radical hysterectomy vs radiation. Am J Obs Gynecol. 2009;201(5):485.e1–9. https://doi.org/10.1016/j.ajog.2009.06.015
National Comprehensive Cancer Network. Cervical Cancer (Version 4.2019). https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed 30 April 2019
Nezhat CR, Burrell MO, Nezhat FR, Benigno BB, Welander CE. Laparoscopic radical hysterectomy with paraaortic and pelvic node dissection. Am J Obstet Gynecol. 1992;166(3):864–5. https://doi.org/10.1016/0002-9378(92)91351-a
Diver E, Hinchcliff E, Gockley A, et al. Minimally invasive radical hysterectomy for cervical cancer is associated with reduced morbidity and similar survival outcomes compared with laparotomy. J Minim Invasive Gynecol. 2017;24(3):402–6. https://doi.org/10.1016/j.jmig.2016.12.005
Nam JH, Park JY, Kim DY, et al. Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: long-term survival outcomes in a matched cohort study. Ann Oncol. 2012;23(4):903–11. https://doi.org/10.1093/annonc/mdr360
Corrado G, Vizza E, Legge F, et al. Comparison of different surgical approaches for stage IB1 cervical cancer patients: a multi-institution study and a review of the literature. Int J Gynecol Cancer. 2018;28(5):1020–8. https://doi.org/10.1097/igc.0000000000001254
Laterza RM, Uccella S, Casarin J, et al. Recurrence of early stage cervical cancer after laparoscopic versus open radical surgery. Int J Gynecol Cancer. 2016;26(3):47–52. https://doi.org/10.1097/igc.0000000000000627
Colombo N, Preti E, Landoni F, et al. Endometrial cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(suppl_6):vi33–8. https://doi.org/10.1093/annonc/mdt353
Ramirez PT, Frumovitz M, Pareja R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Eng J Med. 2018;379(20):1895–904
Kimmig R, Ind T. Minimally invasive surgery for cervical cancer: consequences for treatment after LACC Study. J Gynecol Oncol. 2018;29(4):e75. https://doi.org/10.3802/jgo201829.e75
Naumann RW. Minimally invasive radical hysterectomy has many benefits compared with open radical hysterectomy: will the LACC trial cause the premature demise of this procedure? J Minim Invasive Gynecol. 2019;26(3):379–80. https://doi.org/10.1016/j.jmig.2019.01.002
Leitao MM Jr. The LACC trial: Has minimally invasive surgery for early-stage cervical cancer been dealt a knockout punch? Int J Gynecol Cancer. 2018;28(7):1248–50
Park JY, Nam JH. How should gynecologic oncologists react to the unexpected results of LACC trial? J Gynecol Oncol. 2018;29(4):e74. https://doi.org/10.3802/jgo201829.e74
Margul DJ, Yang J, Seagle BL, et al. Outcomes and costs of open, robotic, and laparoscopic radical hysterectomy for stage IB1 cervical cancer. J Clin Oncol. 2018;36(15_suppl):5502. https://doi.org/10.1200/JCO.2018.36.15_suppl.5502
Melamed A, Margul DJ, Chen L, Keating NL, Del Carmen MG, Yang J, Seagle BL, Alexander A, Barber EL, Rice LW, Wright JD, Kocherginsky M, Shahabi SR-HJ. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med. 2018;379(20):1905–14
Angst E, Hiatt JR, Gloor B, Reber HA, Hines OJ. Laparoscopic surgery for cancer: a systematic review and a way forward. J Am Coll Surg. 2010;211(3):412–23. https://doi.org/10.1016/j.jamcollsurg.2010.05.019.laparoscopic
Kooby DA. Laparoscopic surgery for cancer: historical, theoretical, and technical considerations. Oncol (willist Park). 2006;20(8):917–27
Alletti SG, Petrillo M, Vizzielli G, Bottoni C, Nardelli F, Costantini B, Quagliozzi L, Gallotta V, Scambia G, Fagotti A. Minimally invasive versus standard laparotomic interval debulking surgery in ovarian neoplasm: a single-institution retrospective case-control study. Gynecol Oncol. 2016;143(3):516–520
Gioiella ME, Berkman B, Robinson M. Spirituality and quality of life in gynecologic oncology patients. Cancer Pract. 1998;6(6):333–8. https://doi.org/10.1046/j.1523-5394.1998.006006333.x
Zeng YC, Ching SS, Loke AY. Quality of life measurement in women with cervical cancer: implications for Chinese cervical cancer survivors. Heal Qual Life Outcomes. 2010;19:830
Pecorelli S, Zigliani L, Odicino F. Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obs. 2009;105(2):107–8
Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncol. 2008;9(3):297–303
Kaplan EL, Meier P. Nonparametric estimation from incomplete samples. J Am Stat Assoc. 1958;53(282):457–81
Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep. 1966;50(3):163–70
Cox DR. Models and Life-Tables Regression. J R Stat Soc Ser B (Methodological). 1972;34(2):187–220
Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Laparoscopic compared with open radical hysterectomy in obese women with early-stage cervical cancer. Obs Gynecol. 2012;119(6):1201–9
Shah CA, Veljovich D, Paley P, Beck T, Liao JB, Giannakopoulos N V. Surgical and oncologic outcomes after robotic radical hysterectomy as compared to open radical hysterectomy in the treatment of early cervical cancer. J Gynecol Oncol. 2017;28(6):e82
Wang YZ, Deng L, Xu HC, Zhang Y, Liang, ZQ. Laparoscopy versus laparotomy for the management of early stage cervical cancer. BMC Cancer. 2015. https://doi.org/10.1186/s12885-015-1818-4
Kim SI, Cho JH, Seol A, et al. Gynecologic oncology comparison of survival outcomes between minimally invasive surgery and conventional open surgery for radical hysterectomy as primary treatment in patients with stage IB1–IIA2 cervical cancer. Gynecol Oncol. 2019;153(1):3–12
Wagner AE, Pappas L, Ghia AJ, Gaffney DK. Impact of tumor size on survival in cancer of the cervix and validation of stage IIA1 and IIA2 subdivisions. Gynecol Oncol. 2013;129(3):517–21
Fagotti A, Pedone Anchora L, Conte C, et al. Beyond sentinel node algorithm. Toward a more tailored surgery for cervical cancer patients. Cancer Med. 2016;5(8):1725–30. https://doi.org/10.1002/cam4.722
Ramirez PT, Pareja R, Rendón GJ, Millan C, Frumovitz M, Schmeler KM. Management of low-risk early-stage cervical cancer: Should conization, simple trachelectomy, or simple hysterectomy replace radical surgery as the new standard of care? Gynecol Oncol. 2014;132(1):254–9. https://doi.org/10.1016/j.ygyno.2013.09.004
Kohler C, Hertel H, Herrmann J, et al. Laparoscopic radical hysterectomy with consequent transvaginal closure of vaginal cuff: results of a retrospective analysis of a prospective collected multicenter database. Int J Gynecol Cancer. 2019. https://doi.org/10.1136/ijgc-2019-000388
Mabuchi S, Okazawa M, Matsuo K, et al. Impact of histological subtype on survival of patients with surgically-treated stage IA2-IIB cervical cancer: adenocarcinoma versus squamous cell carcinoma. Gynecol Oncol. 2012;127(1):114–20. https://doi.org/10.1016/j.ygyno.2012.06.021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pedone Anchora, L., Turco, L.C., Bizzarri, N. et al. How to Select Early-Stage Cervical Cancer Patients Still Suitable for Laparoscopic Radical Hysterectomy: a Propensity-Matched Study. Ann Surg Oncol 27, 1947–1955 (2020). https://doi.org/10.1245/s10434-019-08162-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-08162-5