Abstract
Background
The size and importance of socioeconomic status (SES)-based disparities in use of surgery for non-advanced stage gastrointestinal (GI) cancers have not been quantified.
Methods
The exposure in this study of patients age 18–80 with one of nine non-advanced stage GI cancers in the 2007–2015 SEER database was a census tract-level SES composite. Multivariable models assessed associations of SES with use of surgery. Causal mediation analysis was used to estimate the proportion of survival disparities in SES quintiles 1 versus 5 that were mediated by disparities in use of surgery.
Results
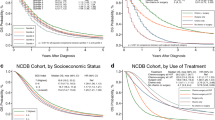
Lowest SES quintile patients underwent surgery at significantly lower rates than highest quintile patients in each cancer. SES-based disparities in use of surgery were large and graded in esophagus adenocarcinoma, intrahepatic and extrahepatic cholangiocarcinoma, and pancreatic adenocarcinoma. Smaller but clinically relevant disparities were present in stomach, ampulla, and small bowel adenocarcinoma, whereas disparities were small in colorectal adenocarcinoma. Five-year all-stage overall survival (OS) was correlated with the size of disparities in use of surgery in SES quintiles 1 versus 5 (r = − 0.87; p = 0.003). Mean OS was significantly longer (range 3.5–8.9 months) in SES quintile 5 versus 1. Approximately one third of SES-based survival disparities in poor prognosis GI cancers were mediated by disparities in use of surgery. The size of disparities in use of surgery in SES quintiles 1 versus 5 was correlated with the proportion mediated (r = 0.98; p < 0.001).
Conclusions
Low SES patients with poor prognosis GI cancers are at substantial risk of undertreatment. Disparities in use of surgery contribute to diminished survival.


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Singh GK, Jemal A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health. 2017;2017:2819372.
McGhan LJ, Etzioni DA, Gray RJ, Pockaj BA, Coan KE, Wasif N. Underuse of curative surgery for early stage upper gastrointestinal cancers in the United States. J Surg Res. 2012;177(1):55–62.
Shapiro M, Chen Q, Huang Q, et al. Associations of socioeconomic variables with resection, stage, and survival in patients with early-stage pancreatic cancer. JAMA Surg. 2016;151(4):338–45.
Michalski CW, Liu B, Heckler M, et al. Underutilization of surgery in periampullary cancer treatment. J Gastrointest Surg. 2019;23(5):959–65.
Boswort B. Increasing disparities in mortality by socioeconomic status. Annu Rev Public Health. 2018;39:237–51.
Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS. National failure to operate on early stage pancreatic cancer. Ann Surg. 2007;246(2):173–80.
Frohman HA, Martin JT, Le AT, Dineen SP, Tzeng CD. Failure to operate on resectable gastric cancer: implications for policy changes and regionalization. J Surg Res. 2017;214:229–39.
Liu N, Molena D, Stem M, Blackford AL, Sewell DB, Lidor AO. Underutilization of treatment for regional gastric cancer among the elderly in the USA. J Gastrointest Surg. 2018;22(6):955–63.
Swords DS, Mulvihill SJ, Skarda DE, et al. Hospital-level variation in utilization of surgery for clinical stage I–II pancreatic adenocarcinoma. Ann Surg. 2019;269(1):133–42.
Swords DS, Mulvihill SJ, Brooke BS, Skarda DE, Firpo MA, Scaife CL. Disparities in utilization of treatment for clinical stage I-II pancreatic adenocarcinoma by area socioeconomic status and race/ethnicity. Surgery. 2019;165(4):751–9.
National Cancer Institute Surveillance, Epidemiology, and End Results Program. Census tract-level SES database. 2019. https://seer.cancer.gov/seerstat/databases/census-tract/index.html. Accessed 13 Apr 2019.
National Comprehensive Cancer Network. NCCN guidelines versioono 1.2019: esophageal and esophagogastric junction cancers. 2019. https://www.nccn.org/professionals/physician_gls/pdf/esophageal.pdf. Accessed 21 Apr 2019.
Lordick F, Mariette C, Haustermans K, Obermannova R, Arnold D. Oesophageal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v51–5.
Taylor LJ, Greenberg CC, Lidor AO, Leverson GE, Maloney JD, Macke RA. Utilization of surgical treatment for local and locoregional esophageal cancer: analysis of the National Cancer Data Base. Cancer. 2017;123(3):410–9.
Yu M, Tatalovich Z, Gibson JT, Cronin KA. Using a composite index of socioeconomic status to investigate health disparities while protecting the confidentiality of cancer registry data. Cancer Causes Control. 2014;25(1):81–92.
Liu L, Deapen D, Bernstein L. Socioeconomic status and cancers of the female breast and reproductive organs: a comparison across racial/ethnic populations in Los Angeles County, California (United States). Cancer Causes Control. 1998;9(4):369–80.
Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for di. Cancer Causes Control. 2001;12(8):703–11.
United States Census Bureau. Census tracts. 2019. https://www2.census.gov/geo/pdfs/education/CensusTracts.pdf. Accessed 13 Apr 2019.
Schisterman EF, Cole SR, Platt RW. Over adjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20(4):488–95.
Sauer BC, Brookhart A, Roy J, Vanderweele T. A review of covariate selection for non-experimental comparative effectiveness research. Pharmacoepidemiol Drug Saf. 2013;22(11):1139–45.
Norton EC, Dowd BE, Maciejewski ML. Odds ratios—current best practice and use. JAMA. 2018;320(1):84–5.
Norton EC, Miller MM, Kleinman LC. Computing adjusted risk ratios and risk differences in Stata. Stata J. 2013;13(3):492–509.
Uno H, Claggett B, Tian L, et al. Moving beyond the hazard ratio in quantifying the between-group difference in survival analysis. J Clin Oncol. 2014;32(22):2380–5.
Baugh KA, Tran Cao HS, van Buren G 2nd, et al. Understaging of clinical stage I pancreatic cancer and the impact of multimodality therapy. Surgery. 2019;165(2):307–14.
Swords DS, Firpo MA, Johnson KM, Boucher KM, Scaife CL, Mulvihill SJ. Implications of inaccurate clinical nodal staging in pancreatic adenocarcinoma. Surgery. 2017;162(1):104–11.
VanderWeele TJ. Policy-relevant proportions for direct effects. Epidemiology. 2013;24(1):175–6.
VanderWeele TJ. A unification of mediation and interaction: a 4-way decomposition. Epidemiology. 2014;25(5):749–61.
Discacciati A, Bellavia A, Lee JJ, Mazumdar M, Valeri L. Med4way: a Stata command to investigate mediating and interactive mechanisms using the four-way effect decomposition. Int J Epidemiol. 2018. https://doi.org/10.1093/ije/dyy236.
Lufti W, Zenati M, Zureikat A, Zeh H, Hogg M. Health disparities impact expected treatment of pancreatic ductal adenocarcinoma nationally. Ann Surg Oncol. 2018;25(7)1860–7.
McDowell BD, Chapman CG, Smith B.J., Button A.M., Chrischilles EA, Mezhir JJ. Pancreatectomy predicts improved survival for pancreatic adenocarcinoma: results of an instrumental variable analysis. Ann Surg. 2015;261(4):740–5.
Swords DS, Mulvihill SJ, Brooke BS, Stoddard GJ, Firpo MA, Scaife CL. County-level Variation in use of surgery and cancer-specific survival for stage I-II pancreatic adenocarcinoma. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003236.
Sridhar P, Misir P, Kwak H, et al. Impact of race, insurance status, and primary language on the presentation, treatment, and outcomes of patients with pancreatic adenocarcinoma at a safety-net hospital. J Am Coll Surg. 2019;229(4):389–96.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Swords, D.S., Mulvihill, S.J., Brooke, B.S. et al. Size and Importance of Socioeconomic Status-Based Disparities in Use of Surgery in Nonadvanced Stage Gastrointestinal Cancers. Ann Surg Oncol 27, 333–341 (2020). https://doi.org/10.1245/s10434-019-07922-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07922-7