Abstract
Background
American College of Surgeons Oncology Group Z0011 confirms the safety of omitting axillary lymph node dissection (ALND) and regional nodal irradiation (RNI) in breast cancer patients with one to two positive sentinel lymph nodes (SLNs), without compromising disease-free survival (DFS) and overall survival (OS). In contrast, the NCIC MA20 trial showed improved DFS in node-positive patients undergoing ALND and RNI. We sought to examine how these data have influenced the management of patients with limited nodal burden.
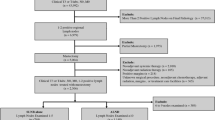
Methods
Using the National Cancer Database, patients diagnosed between 2010 and 2015 and who met the criteria for Z0011 were identified. Logistic regression was used to analyze factors associated with practice patterns. The Cox proportional hazards model was used to assess the association of ALND and RNI with OS.
Results
Omission of ALND in Z0011-eligible patients reached 89.2% in 2015. This Z0011-compliant group was more likely to undergo RNI compared with the non-compliant group (36.4% vs. 31.3%; p < 0.05), with RNI increasing to 43.8% by 2015. Factors associated with the use of RNI included later year of diagnosis [odds ratio (OR) 1.8, 95% confidence interval (CI) 1.6–2.1], hormone receptor-negative tumor (OR 1.2, 95% CI 1.1–1.4), grade 3 tumor (OR 1.2, 95% CI 1.1–1.3), treatment at a non-academic site (OR 1.2, 95% CI 1.1–1.3) and two versus one positive SLN (OR 2.0, 95% CI 1.8–2.2). With 43 months median follow-up, RNI was not associated with improved OS.
Conclusion
Since the publication of Z0011, the omission of ALND has become widespread; however nearly half of these women now receive RNI. The optimal radiation therapy approach for this low nodal burden population warrants further study.




Similar content being viewed by others
References
Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11(10):927–33.
Giuliano A, McCall L, Beitsch P, et al. ACOSOG Z0011: a randomized trial of axillary node dissection in women with clinical T1–2 N0 M0 breast cancer who have a positive sentinel node. J Clin Oncol. 2010;28(18):CRA506.
Giuliano AE, Ballman K, McCall L, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: long-term follow-up from the American College of Surgeons Oncology Group (Alliance) ACOSOG Z0011 Randomized Trial. Ann Surg. 2016;264(3):413–20.
Whelan TJ, Olivotto IA, Parulekar WR, et al. Regional nodal irradiation in early-stage breast cancer. N Engl J Med. 2015;373(4):307–16.
Poortmans PM, Collette S, Kirkove C, et al. Internal mammary and medial supraclavicular irradiation in breast cancer. N Engl J Med. 2015;373(4):317–27.
Ong CT, Thomas SM, Blitzblau RC, et al. Patient age and tumor subtype predict the extent of axillary surgery among breast cancer patients eligible for the American College of Surgeons Oncology Group Trial Z0011. Ann Surg Oncol. 2017;24(12):3559–66.
American College of Surgeons Commission on Cancer. Scope of Regional Lymph Node Surgery: A review of data validity, revised coding directives, and agency transition plans. American College of Surgeons Commission on Cancer; 2012.
Black DM, Jiang J, Kuerer HM, Buchholz TA, Smith BD. Racial disparities in adoption of axillary sentinel lymph node biopsy and lymphedema risk in women with breast cancer racial disparities in sentinel lymph node biopsy racial disparities in sentinel lymph node biopsy. JAMA Surgery. 2014;149(8):788–96.
Woolson RF, Clarke WR. Statistical methods for the analysis of biomedical data, vol. 371. Wiley, New York; 2011.
Hosmer D, Lemeshow S. Applied logistic regression. 2nd ed. New York: Wiley; 2000.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–81.
Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep. 1966;50:163–70.
Cox DR. Regression models and life‐tables. J R Stat Soc Ser B Methodol. 1972;34(2):187–202.
McLaughlin SA, Wright MJ, Morris KT, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol. 2008;26(32):5213.
Petrek JA, Senie RT, Peters M, Rosen PP Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer. 2001;92(6):1368–77.
Giuliano AE, Ballman KV, McCall L, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) Randomized Clinical Trial. JAMA. 2017;318(10):918–26.
Morrow M, Jagsi R, McLeod MC, Shumway D, Katz SJ. Surgeon attitudes toward the omission of axillary dissection in early breast cancer. JAMA Oncol. 2018;4(11):1511–16.
Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med 2011;104(12):510–20.
Mitchell KB, Lin H, Shen Y, et al. DCIS and axillary nodal evaluation: compliance with national guidelines. BMC Surg. 2017;17(1):12.
Jagsi R, Chadha M, Moni J, et al. Radiation field design in the ACOSOG Z0011 (Alliance) Trial. J Clin Oncol. 2014;32(32):3600.
Schlembach PJ, Buchholz TA, Ross MI, et al. Relationship of sentinel and axillary level I–II lymph nodes to tangential fields used in breast irradiation. Int J Radiat Oncol Biol Phys. 2001;51(3):671–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raber, B.M., Lin, H., Shen, Y. et al. Trends in Regional Nodal Management of Breast Cancer Patients with Low Nodal Burden. Ann Surg Oncol 26, 4346–4354 (2019). https://doi.org/10.1245/s10434-019-07901-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07901-y