Abstract
Background
The tumor microenvironment, including cancer-associated fibroblasts (CAFs), plays various clinical roles in cancer growth. CAFs are a heterogeneous population and express a variety of mesenchymal markers. However, the clinical roles for CAFs expressing different markers in pancreatic ductal adenocarcinoma (PDAC) remain unknown.
Methods
We reviewed 67 resected PDAC patients who had not received preoperative therapy. Each primary tumor was analyzed for vimentin and α-smooth muscle actin (α-SMA) expression by immunohistochemical and dual immunofluorescence staining.
Results
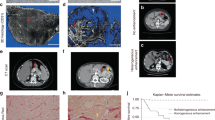
There was no correlation between the percentage of cells expressing vimentin and α-SMA in the tumor stroma (Pearson’s correlation coefficient: r = 0.171). Higher vimentin expression (p = 0.018) was associated with significantly shorter overall survival in PDAC patients. Using dual immunofluorescence staining, vimentin-positive CAFs were divided into two subpopulations: co-expression of α-SMA, and no co-expression of α-SMA. In PDAC, the level of co-expression had no effect on survival using univariate analysis (median survival time, 33.3 months for low co-expression vs. 18.2 months for high co-expression; log-rank, p = 0.143). However, multivariate analysis clarified that CAFs expressing vimentin alone was an independent predictor of poor survival (p = 0.014; hazard ratio, 2.305; 95% confidence interval, 1.181–4.497).
Conclusions
Vimentin-positive CAFs without co-expression of α-SMA were associated with poor survival in PDAC, and CAFs possessed molecular and functional heterogeneity in this disease.



Similar content being viewed by others
References
Kraman M, Bambrough PJ, Arnold JN, et al. Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-alpha. Science. 2010. https://doi.org/10.1126/science.1195300.
Liao D, Luo Y, Markowitz D, Xiang R, Reisfeld RA. Cancer associated fibroblasts promote tumor growth and metastasis by modulating the tumor immune microenvironment in a 4T1 murine breast cancer model. PLoS One. 2009. https://doi.org/10.1371/journal.pone.0007965.
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014. https://doi.org/10.3322/caac.21208.
Neesse A, Michl P, Frese KK, et al. Stromal biology and therapy in pancreatic cancer. Gut. 2011. https://doi.org/10.1136/gut.2010.226092.
Kalluri R, Zeisberg M. Fibroblasts in cancer. Nat Rev Cancer. 2006;6:392–401.
Neesse A, Bauer CA, Öhlund D, et al. Stromal biology and therapy in pancreatic cancer: ready for clinical translation? Gut. 2019. https://doi.org/10.1136/gutjnl-2018-316451.
Sugimoto H, Mundel TM, Kieran MW, Kalluri R. Identification of fibroblast heterogeneity in the tumor microenvironment. Cancer Biol Ther. 2006;5:1640–6.
Neuzillet C, Tijeras-Raballand A, Ragulan C, et al. Inter- and intra-tumoural heterogeneity in cancer-associated fibroblasts of human pancreatic ductal adenocarcinoma. J Pathol. 2019. https://doi.org/10.1002/path.5224.
Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016. https://doi.org/10.1038/nrc.2016.73.
Bu L, Baba H, Yoshida N, et al. Biological heterogeneity and versatility of cancer-associated fibroblasts in the tumor microenvironment. Oncogene. 2019. https://doi.org/10.1038/s41388-019-0765-y.
Nielsen MF, Mortensen MB, Detlefsen S. Key players in pancreatic cancer-stroma interaction: Cancer-associated fibroblasts, endothelial and inflammatory cells. World J Gastroenterol. 2016. https://doi.org/10.3748/wjg.v22.i9.2678.
Öhlund D, Handly-Santana A, Biffi G, et al. Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. J Exp Med. 2017. https://doi.org/10.1084/jem.20162024.
Ikuta D, Miyake T, Shimizu T, et al. Fibrosis in metastatic lymph nodes is clinically correlated to poor prognosis in colorectal cancer. Oncotarget. 2018; 9: 29574–29586.
Erez N, Truitt M, Plson P, Arron ST, Hanahan D. Cancer-associated fibroblasts are activated in incipient neoplasia to orchestrate tumor-promoting inflammation in an NF-kappaB-dependent manner. Cancer Cell. 2010. https://doi.org/10.1016/j.ccr.2009.12.041.
Sobin LH, Gospodarowicz MK, Wittekind C, eds. International Union Against Cancer. TNM classification of malignant tumors, 7th edn. New Jersey: Wiley-Blackwell, 2009.
Nitta T, Mitsuhashi T, Hatanaka Y, et al. Prognostic significance of epithelial-mesenchymal transition-related markers in extrahepatic cholangiocarcinoma: comprehensive immunohistochemical study using a tissue microarray. Br J Cancer. 2014. https://doi.org/10.1038/bjc.2014.415.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013. https://doi.org/10.1038/bmt.2012.244.
Maehira H, Iida H, Mori H, et al. Computed tomography enhancement pattern of the pancreatic parenchyma predicts postoperative pancreatic fistula after pancreaticoduodenectomy. Pancreas. 2019. https://doi.org/10.1097/MPA.0000000000001229.
Iida H, Maehira H, Mori H, et al. Serum procalcitonin as a predictor of infectious complication after pancreaticoduodenectomy: review of the literature and our experience. Surg Today. 2019. https://doi.org/10.1007/s00595-019-01811-y.
Iida H, Tani M, Maehira H, et al. Postoperative pancreatic swelling predicts pancreatic fistula after pancreaticoduodenectomy. Am Surg. 2019;85:321–6.
Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011. https://doi.org/10.1056/NEJMoa1011923.
Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013. https://doi.org/10.1056/NEJMoa1304369.
Fujita H, Ohuchida K, Mizumoto K, et al. Alpha-smooth muscle actin expressing stroma promotes an aggressive tumor biology in pancreatic ductal adenocarcinoma. Pancreas. 2010. https://doi.org/10.1097/MPA.0b013e3181dbf647.
Sinn M, Denkert C, Striefler JK, et al. α-Smooth muscle actin expression and desmoplastic stromal reaction in pancreatic cancer: results from the CONKO-001 study. Br J Cancer. 2014. https://doi.org/10.1038/bjc.2014.495.
Özdemir BC, Pentcheva-Hoang T, Carstens JL, et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014. https://doi.org/10.1016/j.ccr.2014.04.005.
Rhim AD, Oberstein PE, Thomas DH, et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014. https://doi.org/10.1016/j.ccr.2014.04.021
Kawase T, Yasui Y, Nishina S, et al. Fibroblast activation protein-α-expressing fibroblasts promote the progression of pancreatic ductal adenocarcinoma. BMC Gastroenterol. 2015. https://doi.org/10.1186/s12876-015-0340-0.
Shi M, Yu DH, Chen Y, et al. Expression of fibroblast activation protein in human pancreatic adenocarcinoma and its clinicopathological significance. World J Gastroenterol. 2012. https://doi.org/10.3748/wjg.v18.i8.840.
Whittle MC, Hingorani SR. Fibroblasts in pancreatic ductal adenocarcinoma: biological mechanisms and therapeutic targets. Gastroenterology. 2019. https://doi.org/10.1053/j.gastro.2018.12.044.
Acknowledgment
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
H. Maehira and T.M. described and designed the article. M.T. revised the article. H. Maehira and K.M performed microscopic evaluation. H.I., A.T., H. Mori, D.Y., and T.S. performed the surgery and postoperative management. All authors read and approved the final article.
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplementary Fig.
1 Receiver operating characteristic (ROC) curve of Vimentin expression rate (a), co-expression rate of α-SMA and Vimentin (b), single α-SMA expression (c), and single Vimentin expression (d) for alive or dead analysis at the median follow-up time. The areas under the ROC are 0.604 (95% CI, 0.448–0.760), 0.538 (95% CI, 0.396–0.681), 0.655 (95% CI, 0.524–0.786), and 0.598 (95% CI, 0.452–0.743), respectively (TIFF 191 kb)
Supplementary Fig.
2 Kaplan–Meier analyses of RFS (a) and OS (b), according to the CAF number in the tumor, and of RFS (c) and OS (d), according to the CAF number per tumor area, as determined by dual IF staining. CAF cancer-associated fibroblasts; RFS recurrent-free survival; OS overall survival; IF immunofluorescence (TIFF 106 kb)
Supplementary Fig.
3 Kaplan–Meier analyses of RFS (a) and OS (b) according to the degree of α-SMA single expression in the central part of the tumor stroma, as determined by dual IF staining. RFS recurrent-free survival; OS overall survival; α-SMA alpha-smooth muscle actin; IF immunofluorescence (TIFF 74 kb)
Rights and permissions
About this article
Cite this article
Maehira, H., Miyake, T., Iida, H. et al. Vimentin Expression in Tumor Microenvironment Predicts Survival in Pancreatic Ductal Adenocarcinoma: Heterogeneity in Fibroblast Population. Ann Surg Oncol 26, 4791–4804 (2019). https://doi.org/10.1245/s10434-019-07891-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07891-x