Abstract
Background
Adherence to quality measures has become an important indicator of cancer center performance for high-quality cancer care. We examined regional variation in performance for Commission on Cancer breast quality measures and its impact on overall survival (OS) for those measures that have been shown to impact OS.
Methods
Six breast quality measures were analyzed using the National Cancer Data Base from 2014 to 2015, and a multivariable model was used to assess performance for each measure by region. Kaplan–Meier and Cox proportional hazard models were used to examine OS between high- and low-performing centers from 2007 to 2012.
Results
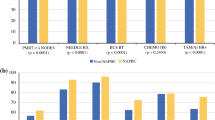
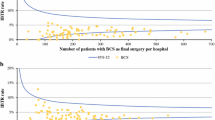
Overall, 305,391 women had surgery at 1322 institutions in nine US regions; 90.8% underwent needle biopsy (range 86.0–92.6% between regions, p < 0.01), 69.8% had breast-conserving surgery (BCS) for stage 0–II cancer (60.9–79.3%, p < 0.01), 85.2% aged < 70 years had radiation therapy (RT) after BCS (79.6–90.8%, p < 0.01), 78.3% of women with four or more positive nodes had post-mastectomy RT (70.9–84.5%, p < 0.01), 90.9% with hormone receptor (HR)-positive stage IB–III cancer had hormone therapy (83.7–95.1%, p < 0.01), and 89.4% aged < 70 years with HR-negative stage IB–III cancer had chemotherapy (87.6–91.4%, p < 0.01). Multivariate analyses adjusted for patient and facility factors found that region was the only consistent predictor of non-compliance across measures. With median 65-month follow-up, there was no difference in OS between high- and low-performing centers for the three measures that have been shown to impact OS.
Conclusions
There is significant regional variation in performance on the breast quality measures but this variation did not impact OS. Targeted efforts in certain areas of the country may help improve performance on these measures.


Similar content being viewed by others
References
Bensenhaver J, Winchester DP. Surgical leadership and standardization of multidisciplinary breast cancer care: the evolution of the National Accreditation Program for Breast Centers. Surg Oncol Clin N Am 2014;23(3):609–16.
American College of Surgeons. CoC Quality of Care Measures: Standard 4.4 and 4.5 Expected Performance Rates, 2018 Surveys. 2018. Available at: https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasures. Accessed 3 Apr 2018.
Knutson AC, McNamara EJ, McKeller DP, Kaufman CS, Winchester DP. The role of the American College of Surgeons’ cancer program accredidation in influencing oncologic outcomes. J Surg Oncol 2014;110(5):611–5.
Schroeck FR, Kaufman SR, Jacobs BL, Skolarus TA, Hollingsworth JM, Shahinian VB, et al. Regional variation in quality of prostate cancer care. J Urol 2014;191(4):957–62.
Kasumova GG, Eskander MF, de Geus SWL, et al. Regional variation in the treatment of pancreatic adenocarcinoma: Decreasing disparities with multimodality therapy. Surgery 2017;162(2):275–84.
Monson JR, Probst CP, Wexner SD, et al. Failure of evidence-based cancer care in the United States: the association between rectal cancer treatment, cancer center volume, and geography. Ann Surg 2014;260(4):625–31.
Rahal R, Cadder J, DeCaria K, Lockwood G, Bryan H; System Performance Steering Committee and the Technical Working Group. How difference is cancer control across Canada? Comparing performance indicators for prevention, screening, diagnosis, and treatment. Curr Oncol 2017; 24(2);124–8.
Chiu AS, Thomas P, Killelea BK, Horowitz N, Chagpar AB, Lannin DR. Regional variation in breast cancer surgery: results from the National Cancer Database (NCDB). Am J Surg 2017;214(5):907–13.
Punglia RS, Cronin AM, Uno H, et al. Association of Regional Intensity of Ductal Carcinoma In Situ Treatment With Likelihood of Breast Preservation. JAMA Oncol 2017;3(1):101–4.
Berger ER, Wang CE, Kaufmann CS, et al. National Accreditation Program for Breast Centers Demonstrates Improved Compliance with Post-Mastectomy Radiation Therapy Quality Measure. J Am Coll Surg 2017;224(3):236–44.
Feinstein AJ, Soulos PR, Long JB, Herrin J, Roberts KB, Yu JB, et al. Variation in receipt of radiation therapy after breast-conserving surgery: assessing the impact of physicians and geographic regions. Med Care 2013;51(4):330–8.
Daly B, Olopade OI, Hou N, Yao K, Winchester DJ, Huo D. Evaluation of the Quality of Adjuvant Endocrine Therapy Delivery for Breast Cancer Care in the United States. JAMA Oncol 2017;3(7):928–35.
Parise CA, Caggiano V. Regional variation in disparities in breast cancer specific mortality due to race/ethnicity, socioeconomic status, and urbanization. J Racial Ethn Health Disparities 2017;4(4):706–17.
De Angelis R, Sant M, Coleman MP, et al. Cancer survival in Europe 1999-2007 by country and age: results of EUROCARE-5: a population-based study. Lancet Oncol 2014;15(1):23–34.
Bilimoria KY, Bentrem DJ, Steward AK, Wincehster DP, Ko CY. Comparison of Commission On Cancer-approved and -nonapproved hospitals in the United States: implications for studies that use the National Cancer Data Base. J Clin Oncol 2009;27(25):4177–81.
American Joint Committee on Cancer. AJCC Cancer Staging Manual. 7th ed. Chicago, IL: Springer; 2010.
US Census. Statistical Groupings of States and Counties. 2010. Available at: http://www.census.gov/geo/reference/pdfs/GARM/Ch6GARM.pdf. Accessed 3 Apr 2018.
Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25(33):5203–9.
Yao K, Stewart AK, Winchester DJ, Winchester DP. Trends in contralateral prophylactic mastectomy for unilateral cancer: a report from the National Cancer Data Base, 1998–2007. Ann Surg Oncol 2010;17(10):2554–62.
Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg 2015;150(1):9–16.
Yanez B, Stanton AL, Maly RC. Breast cancer treatment decision making among Latinas and non-Latina Whites: a communication model predicting decisional outcomes and quality of life. Health Psychol 2012;31(5):552–61.
Ess S, Savidan A, Frick H, Rageth CH, Vlastos G, Lutolf U, et al. Geographic variation in breast cancer care in Switzerland. Cancer Epidemiol 2010;34(2):116–21.
Breslin TM, Caughran J, Pettingra J, et al. Improving breast cancer care through a regional quality collaborative. Surgery 2011;150(4):635–42.
Reames BN, Shubeck SP, Birkmeyer JD. Strategies for reducing regional variation in the use of surgery: a systemic review. Ann Surg 2014;259(4):616–27.
Stacey D, Legare F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017;(1):CD001431.
Spain P, Teixeira-Poit S, Halpern MT, et al. The National Cancer Institute Community Cancer Centers Program (NCCCP): Sustaining Quality and Reducing Disparities in Guideline-Concordant Breast and Colon Cancer Care. Oncologist 2017; 22(8):910–7.
Birkmeyer NJ, Goodney PP, Stukel TA, Hillner BE, Birkmeyer JD. Do cancer centers designated by the National Cancer Institute have better surgical outcomes? Cancer 2005;103(3):435–41.
Bristow RE, Chang J, Ziogas A, Campos B, Chavez LR, Anton-Culver H. Impact of National Cancer Institute Comprehensive Cancer Centers on ovarian cancer treatment and survival. J Am Coll Surg 2015;220(5):940–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Olga Kantor, Chi-Hsiung Wang, and Katharine Yao have no disclosures to declare.
Rights and permissions
About this article
Cite this article
Kantor, O., Wang, CH. & Yao, K. Regional Variation in Performance for Commission on Cancer Breast Quality Measures and Impact on Overall Survival. Ann Surg Oncol 25, 3069–3075 (2018). https://doi.org/10.1245/s10434-018-6592-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6592-5