Abstract
Purpose
To develop a nomogram that estimates 1-year recurrence-free survival (RFS) after trimodality therapy for esophageal adenocarcinoma and to assess the overall survival (OS) benefit of esophagectomy after chemoradiotherapy (CRT) on the basis of 1-year recurrence risk.
Methods
In total, 568 consecutive patients with potentially resectable esophageal adenocarcinoma who underwent CRT were included for analysis, including 373 patients who underwent esophagectomy after CRT (trimodality therapy), and 195 who did not undergo surgery (bimodality therapy). A nomogram for 1-year RFS was created using a Cox regression model. The upper tertile of the nomogram score was used to stratify patients in low-risk and high-risk groups for 1-year recurrence. The 5-year OS was compared between trimodality and bimodality therapy in low-risk and high-risk patients after propensity score matching, respectively.
Results
Median follow-up for the entire cohort was 62 months. The 5-year OS in the trimodality and bimodality treatment groups was 56.3% (95% confidence interval [CI] 47.9–64.7) and 36.9% (95% CI 31.4–42.4), respectively. The final nomogram for the prediction of 1-year RFS included male gender, poor histologic grade, signet ring cell adenocarcinoma, cN1, cN2-3, and baseline SUVmax, with accurate calibration and reasonable discrimination (C-statistic: 0.66). Trimodality therapy was associated with improved 5-year OS in low-risk patients (p = 0.003), whereas it showed no significant survival benefit in high-risk patients (p = 0.302).
Conclusions
The proposed nomogram estimates early recurrence risk. The addition of surgery to CRT provides a clear OS benefit in low-risk patients. The OS benefit of surgery in high-risk patients is less pronounced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Neoadjuvant chemoradiotherapy (CRT) combined with surgical resection of the esophagus (trimodality therapy) is a generally recommended treatment strategy with curative intent for patients with locally advanced esophageal cancer.1,2 Definitive CRT (bimodality therapy) is an alternative approach for patients with a poor performance status or inoperable locally advanced esophageal cancer.3,4 Despite recent improvement in multimodality treatment and perioperative care, esophageal cancer remains a devastating condition for the patient with an estimated 5-year overall survival (OS) rate of 36–47% after trimodality therapy.5,6,7
The relatively poor OS even after trimodality therapy is partially attributable to the high incidence (49–85%) of disease recurrence after surgery.8 The remaining OS of patients in this setting is generally poor.9 To advocate an extensive surgical resection, such as esophagectomy, there should be a fair chance of improving OS combined with an acceptable health-related quality of life.10 Despite improvements in (minimally invasive) surgical techniques, esophageal resection can still induce significant treatment-related morbidity and mortality.11,12 Furthermore, esophagectomy has been associated with a reduction in health-related quality of life up to 3–12 months following surgery.13,14,15 As such, in the group of patients who experience early disease recurrence within 1 year of completing their treatment, the benefit of surgery would probably not outweigh its potential side-effects.13,14,15 Some suggest that consideration should be given to less invasive treatment strategies in patients who are likely to have early disease recurrence after surgery.10 Preoperative identification of these patients may help to guide subsequent treatment decision-making.
Currently, most available studies that assessed prognosis after trimodality therapy rely on the postoperative available pathology results of the resection specimen, limiting their practical use at the time of surgical decision-making.10,16,17 Additionally, no single clinicopathological characteristic in esophageal cancer can yet optimally predict prognosis preoperatively. Therefore, the purpose of the current study was to develop a preoperative risk prediction model for 1-year recurrence-free survival (RFS) after trimodality therapy for esophageal adenocarcinoma—incorporating multiple clinicopathological characteristics and 18F-FDG PET/CT features—and assess the OS benefit of subsequent surgery after CRT in patients at low and high risk of early disease recurrence.
Methods
Study Population
From a prospectively acquired database, all patients with locally advanced potentially resectable adenocarcinoma of the esophagus (cT1N+ or cT2-4aNany) considered eligible for curative resection after initial staging who underwent trimodality therapy or bimodality therapy between January 2006 and February 2016, at the MD Anderson Cancer Center were identified. Patients were excluded if 18FDG-PET/CT scanning before and after CRT was not performed or if restaging after CRT discovered distant metastases. Staging was performed in accordance with the 7th edition of the International Union Against Cancer cTNM-classification.18 Initial diagnostic work-up included endoscopy with biopsy, endoscopic ultrasound (including fine-needle aspiration if indicated), and 18F-FDG PET/CT. The cT-status and cN-status reported in this study were determined before the start of CRT. This study was approved by the institutional review board at MD Anderson Cancer Center and the requirement to obtain informed consent was waived. The data were analysed in May 2017.
Treatment Protocol
CRT consisted of fluoropyrimidine (intravenous or oral) with either a platinum or a taxane compound with concurrent radiotherapy (45 or 50.4 Gy in fractions of 1.8 Gy) (Table 1). Patients were considered to have received trimodality therapy if esophagectomy was performed within 4 months after completion of CRT. Reasons to refrain from surgery (bimodality therapy) included patient and physician choice (e.g., physician preference for observation) or a decline in performance status secondary to CRT. Surgical treatment consisted of either transhiatal esophagectomy with abdominal lymphadenectomy or Ivor Lewis esophagectomy with abdominal and thoracic lymphadenectomy. The choice of technique was at the discretion of the treating surgeon.
Follow-Up
After treatment patients were routinely monitored at intervals of 3 months in the first year, 6 months during the second and third year, and 12 months until 5 years after treatment or until death. The follow-up assessment consisted of routine blood tests, chest/abdominal CT, endoscopy with biopsies, and/or 18F-FDG PET/CT. The main endpoint of this study was 1-year RFS after trimodality therapy and was calculated from the day of surgery to either the date of recurrence or end of follow-up (censored at 12 months in case of > 12 months follow-up). OS was calculated from the end of CRT to either date of death or last follow-up (censored at 5 years in case of > 5-year follow-up).
Preoperative Predictors
Clinical characteristics were derived from the prospective collected departmental registry. Initial selection of predictors for for 1-year RFS were prespecified based on previous literature to prevent overfitting of the model. Categories were based on previously published cut-off points (Table 1).10,19,20,21
Statistical Analysis
Missing data were considered at random and handled using imputation with the iterative Markov chain Monte Carlo method.22 Kaplan–Meier curves were used to assess RFS and OS, and differences were evaluated by using the log-rank test. Statistical analysis was performed using SPSS version 24.0 (IBM Corp., Armonk, NY) and R 3.1.2 open-source software (http://www.R-project.org; MatchIt, optmatch, rms, Hmisc, mice, packages). A p value < 0.05 was considered statistically significant.
Model Development
For the development of the model for 1-year RFS only trimodality patients were used. In case of high correlated variables (i.e., Spearman rank correlation coefficient r ≥ 0.6) the easiest measurable factor was included. The initial multivariable Cox regression model was reduced by using backward stepwise elimination and the Akaike Information Criteria (AIC) was used to compare different models. The discriminative ability of the final model for 1-year RFS was evaluated using Harrell’s C-statistic.23 For internal validation, the model was subjected to 200 bootstrap resamples to calculate the optimism of the model, after which the C-statistic was adjusted and a shrinkage factor was calculated to correct the β-coefficients. Calibration of the final model, which reflects the agreement between predicted versus actual (observed) outcomes, was visualized with calibration plots after bias correction. The final model was used to construct a nomogram.
Propensity Score Matching
The upper tertile of the nomogram score was used to stratify patients in low-risk and high-risk groups for recurrence within 1 year. Propensity score matching was used to balance patient characteristics between the trimodality and bimodality group within the different risk strata. A propensity score was generated using logistic regression, based on all covariates presented in Table 2. Subsequently, the nearest-neighbour matching technique was used to generate matched pairs of cases (1:1) using a caliper width of 0.45.24 Kaplan–Meier curves were used to compare OS between trimodality and bimodality for low-risk and high-risk groups, respectively.
Results
Patient and Treatment-Related Characteristics
From 568 patients with esophageal adenocarcinoma that met our inclusion and exclusion criteria, 373 underwent trimodality therapy and 195 underwent bimodality therapy (Fig. 1). The distribution of patient and treatment-related characteristics are summarized in Table 1. Of the trimodality patients, 345 (93%) underwent Ivor-Lewis esophagectomy, in 352 (94%) a R0 resection was achieved, and the median number of harvested lymph nodes was 21 (Interquartile range: 15–26). Most common postoperative complications were pulmonary complications (26%), atrial fibrillation (15%), and anastomotic leakage (9%). The median follow-up was 62 months (range 1–130) for the entire cohort. The 5-year OS rate in the trimodality and bimodality treatment groups were 56.3% (95% confidence interval [CI] 47.9–64.7) and 36.9% (95% CI 31.4–42.4), respectively.
Preoperative Prediction Model for Early Disease Recurrence
Among the 373 trimodality patients, 102 (Kaplan–Meier estimate: 28%) had recurrence within 1 year following esophagectomy, with 91 (89%) having distant metastases. Median OS after documentation of disease recurrence within 1 year after surgery was 9.1 months (95% CI 6.6–11.6). A detailed description of the location and treatment of 1-year disease recurrence is summarized in Supplemental Table 1.
The association of clinical characteristics with 1-year RFS in univariable analysis are presented in supplemental Table 2. After multivariable analysis, male gender (optimism adjusted hazard ratio [aHR] 2.13, 95% CI 0.95–4.77), poor tumor differentiation grade (aHR 1.59, 95% CI 1.07–2.35), signet ring cell adenocarcinoma (cHR 1.72, 95% CI 1.07–2.75), baseline cN1 (aHR 1.72, 95% CI 1.09–2.75), baseline cN2-3 (aHR 2.07, 95% CI 1.27–3.38), and baseline SUVmax ≥ 7 (aHR 1.71, 95% CI 1.09–2.69), were independently predictive for 1-year RFS, respectively (Supplemental Table 3). A nomogram based on these variables was constructed (Fig. 2). The discriminative ability of the nomogram was reasonable with an apparent C-statistic of 0.67 and 0.66 after adjustment for optimism. Calibration was accurate, with predictions corresponding closely with the actual observed 1-year RFS probability (Supplemental Fig. 1).
Risk Stratification of Early Disease Recurrence
Based on the nomogram score patients receiving trimodality treatment were grouped into a low-risk (< 276 nomogram points; number of patients in group = 256) and a high-risk group (≥ 276 nomogram points; number of patients in group = 117) for early disease recurrence, respectively. The corresponding 1-year RFS estimate of the low-risk group (80%) was significantly better than the high-risk group (54%) (log-rank test: p < 0.001). After applying the same nomogram score cutoff values to patients in the bimodality group, stratification into low-risk (number of patients in group = 135) and high-risk (number of patients in group = 60) groups allowed significant distinction between 1-year RFS (60 vs. 46%, log-rank test: p = 0.049, respectively).
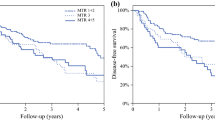
Survival Comparison Between Trimodality and Bimodality Therapy in Low- and High-Risk Patients
After propensity score matching, balance in patient and tumor characteristics between the stratified trimodality and bimodality groups was achieved (Table 2). In the low-risk group, 5-year OS was significantly better after trimodality therapy compared with bimodality therapy (66 vs. 46%, respectively; log-rank test: p = 0.003). In the high-risk patients, 5-year OS difference of trimodality versus bimodality therapy was not statistically significant (32 vs. 21%, respectively; log-rank test: p = 0.302, respectively; Fig. 3).
Discussion
In this study, a preoperative prediction model for early disease recurrence for esophageal cancer patients treated with trimodality therapy was developed. In summary, the proposed nomogram showed accurate calibration and reasonable discrimination (C-statistic: 0.66). Stratification into different risk groups based on the nomogram score allowed significant distinction between 1-year RFS and OS. Treatment with esophagectomy after CRT for patients with a low-risk of early disease recurrence resulted in a substantially higher 5-year OS compared with patients who underwent definitive CRT. Interestingly, the OS benefit of surgery was less apparent (and nonsignificant) in patients with a high-risk of early disease recurrence. Before surgery, by using this easy-to-use scoring system treating physicians could generate individualized predictions on early disease recurrence after surgery. As such, identifying subgroups of patients with different risks of early recurrence may impact shared treatment decision-making and choices of care.
Currently, the NCCN guideline recommends preoperative chemoradiation with subsequent esophagectomy for medically fit patients with locally advanced esophageal cancer.2 However, despite multimodality treatment strategies, studies have reported that as many as 29% of the patients experience disease recurrence within 1-year after esophagectomy.7 The location of disease recurrence is typically systemic (86–88%) and results in a poor median OS of only 3–9 months.8,25,26 These findings were verified by the current study in which 28% of the patients experienced disease recurrence within 1 year after trimodality therapy (89% systemic), with a median post-recurrence survival of 9 months.
The relatively high incidence of early disease recurrence after trimodality therapy suggests that small distant metastases, which are not detected by currently available staging techniques, may already have occurred at the time of esophagectomy.20 Until clinical staging improves significantly, the key point of handling early disease recurrence is to identify high-risk patients and consider alternative treatment strategies. If high-risk patients could be identified accurately, alternative less invasive strategies would be to delay esophagectomy after extensive CRT (with 50.4 Gy) and closely monitor patients for systemic disease. Salvage surgery could then still be an option in high-risk patients who did not develop early systemic recurrence within 1 year.27,28 Another option would be to avoid chemoradiation due to its considerable morbidity and directly move to esophagectomy.29 However, risk stratified treatment pathways in this setting that are most beneficial for patients have yet to be investigated.
The current study identified gender, poor tumor differentiation grade, signet ring cell adenocarcinoma, baseline cN1, cN2-3, and baseline SUVmax ≥ 7 as independent prognostic factors for 1-year RFS. These findings are in concordance with previous reports on risk factors for oncologic outcomes (i.e., RFS and OS) after esophagectomy.10,19,20,21,29 By stratifying patients using cutoff values from the proposed nomogram, it was possible to separate patients in low-risk and high-risk groups for 1-year disease recurrence with distinct OS outcomes. For patients with a low-risk profile, the prognosis after trimodality therapy was substantially better compared with patients treated with bimodality therapy.
In the high-risk group, however, patients had a 46% chance of disease recurrence within 1-year after surgery, with no significant OS difference compared to patients treated with bimodality therapy. Because the OS benefit of trimodality therapy in these high-risk patients was considerably less pronounced, an argument could therefore be made to refrain from surgery in these patients. Despite this, most physicians will find it difficult to withhold surgery from a patient with an otherwise resectable tumor based on the predicted outcomes of a nomogram. This is especially true when considering that even some of these high-risk patients are cured after trimodality therapy. Our nomogram should be considered as a first step in the challenging process of patient selection. However, our study at least indicates that a subgroup of patients is likely not served by a multimodality treatment strategy. At best for now, these high-risk patients should be informed about their individual potential for disease recurrence for them to balance the possible risks and benefits of the various treatment strategies.
The discriminative ability of the proposed nomogram may benefit from further refinement with additional predictors in the future. The incorporation of validated risk prediction models for the occurrence and severity of postoperative complications, for example, may further facilitate preoperative decision making.30 Furthermore, potential advances that could improve patient selection in the future include blood biomarkers (e.g., circulating tumor DNA) and functional magnetic resonance imaging.31,32,33 The latter has shown to have a role in the prediction of pathologic complete response to neoadjuvant CRT.32,33
Important limitations of this study are that it represents a single-institution analysis, where findings may not be generalizable to other centres. Therefore, external validation of the developed nomogram is warranted to determine generalizability.34 Second, although propensity score matching was performed to improve the comparability between the two treatment groups, unknown confounding factors may have influenced our findings. Third, the absence of a statistical significant benefit of esophagectomy in the high-risk patient may be due to a lack of power. As such, the risk-stratified analysis should be validated in a large population. Despite these limitations, the major strengths of this study include that it is the first demonstration of a clinically applicable nomogram for preoperative prediction of 1-year RFS after esophagectomy, providing detailed analyses of handling variables, model building, validation, and calibration according to a standardized template for conducting and reporting of prognostic studies.35 This will facilitate validation in other populations and incorporation of other factors to improve this model. Also, the ability of the nomogram to make significant distinction between 1-year RFS in another patient group (i.e., the bimodality group) suggests generalizability of the model.
This study demonstrates a novel nomogram that predicts the preoperative probability of early disease recurrence after trimodality therapy for patients with esophageal cancer. The addition of surgery to CRT provided a clear OS benefit in patients at low risk of early disease recurrence. The OS benefit of surgery in high-risk patients was less pronounced. External validation and improvement of the model with new imaging or biomarkers is desired.
References
Lordick F, Mariette C, Haustermans K, Obermannová R, Arnold D. Oesophageal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Onconl. 2016. https://doi.org/10.1093/annonc/mdw329.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)—Esophageal and Esophagogastric Junction Cancers Version 3. 2017. http://www.nccn.org/professionals/physician_gls/pdf/esophageal.pdf. Accessed 1 Jan 2017.
Gwynne S, Hurt C, Evans M, Holden C, Vout L, Crosby T. Definitive chemoradiation for oesophageal cancer—a standard of care in patients with non-metastatic oesophageal cancer. Clin Oncol. 2011;23(3):182–8. https://doi.org/10.1016/j.clon.2010.12.001.
Teoh AYB, Chiu PWY, Yeung WK, Liu SYW, Wong SKH, Ng EKW. Long-term survival outcomes after definitive chemoradiation versus surgery in patients with resectable squamous carcinoma of the esophagus: results from a randomized controlled trial. Ann Oncol. 2013;24(1):165–71. https://doi.org/10.1093/annonc/mds206.
van Hagen P, Hulshof MC, van Lanschot JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84. https://doi.org/10.1056/nejmoa1112088.
Sjoquist KM, Burmeister BH, Smithers BM, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12(7):681–92. https://doi.org/10.1016/s1470-2045(11)70142-5.
Shapiro J, van Lanschot JJB, Hulshof MCCM, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16(9):1090–8. https://doi.org/10.1016/s1470-2045(15)00040-6.
Goense L, van Rossum PS, Reitsma JB, et al. Diagnostic performance of (1)(8)F-FDG PET and PET/CT for the detection of recurrent esophageal cancer after treatment with curative intent: a systematic review and meta-analysis. J Nucl Med. 2015;56(7):995–1002. https://doi.org/10.2967/jnumed.115.155580.
Parry K, Visser E, van Rossum PSN, Mohammad NH, Ruurda JP, van Hillegersberg R. Prognosis and treatment after diagnosis of recurrent esophageal carcinoma following esophagectomy with curative intent. Ann Surg Oncol. 2015;22(Suppl 3):1292–300. https://doi.org/10.1245/s10434-015-4840-5.
Davies AR, Pillai A, Sinha P, et al. Factors associated with early recurrence and death after esophagectomy for cancer. J Surg Oncol. 2014;109(5):459–64. https://doi.org/10.1002/jso.23511.
Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet. 2012;379(9829):1887–92. https://doi.org/10.1016/s0140-6736(12)60516-9.
Briez N, Piessen G, Torres F, Lebuffe G, Triboulet J-P, Mariette C. Effects of hybrid minimally invasive oesophagectomy on major postoperative pulmonary complications. Br J Surg. 2012;99(11):1547–53. https://doi.org/10.1002/bjs.8931.
Safieddine N, Xu W, Quadri SM, et al. Health-related quality of life in esophageal cancer: effect of neoadjuvant chemoradiotherapy followed by surgical intervention. J Thorac Cardiovasc Surg. 2009;137(1):36–42. https://doi.org/10.1016/j.jtcvs.2008.09.049.
Lagergren P, Avery KNL, Hughes R, et al. Health-related quality of life among patients cured by surgery for esophageal cancer. Cancer. 2007;110(3):686–93. https://doi.org/10.1002/cncr.22833.
de Boer AGEM, van Lanschot JJB, van Sandick JW, et al. Quality of life after transhiatal compared with extended transthoracic resection for adenocarcinoma of the esophagus. J Clin Oncol. 2004;22(20):4202–8. https://doi.org/10.1200/jco.2004.11.102.
Francis AM, Sepesi B, Correa AM, et al. The influence of histopathologic tumor viability on long-term survival and recurrence rates following neoadjuvant therapy for esophageal adenocarcinoma. Ann Surg. 2013;258(3):500–7. https://doi.org/10.1097/sla.0b013e3182a196f4.
Shapiro J, Biermann K, van Klaveren D, et al. Prognostic value of pretreatment pathological tumor extent in patients treated with neoadjuvant chemoradiotherapy plus surgery for esophageal or junctional cancer. Ann Surg. 2017;265(2):356–62. https://doi.org/10.1097/sla.0000000000001630.
Rice TW, Blackstone EH, Rusch VW. 7th edition of the AJCC cancer staging manual: esophagus and esophagogastric junction. Ann Surg Oncol. 2010;17(7):1721–4. https://doi.org/10.1245/s10434-010-1024-1.
Stiles BM, Salzler GG, Nasar A, et al. Clinical predictors of early cancer-related mortality following neoadjuvant therapy and oesophagectomy. Eur J Cardio-Thoracic Surg. 2015;48(3):455–60. https://doi.org/10.1093/ejcts/ezu479.
Zhu Z-J, Hu Y, Zhao Y-F, Chen X-Z, Chen L-Q, Chen Y-T. Early recurrence and death after esophagectomy in patients with esophageal squamous cell carcinoma. Ann Thorac Surg. 2011;91(5):1502–8. https://doi.org/10.1016/j.athoracsur.2011.01.007.
Xi M, Liao Z, Deng W, et al. A prognostic scoring model for the utility of induction chemotherapy prior to neoadjuvant chemoradiotherapy in esophageal cancer. J Thorac Oncol. 2017;12(6):1001–10. https://doi.org/10.1016/j.jtho.2017.03.017.
Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. https://doi.org/10.1136/bmj.b2393.
Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87. https://doi.org/10.1002/(sici)1097-0258(19960229)15:4<361::aid-sim168>3.0.co;2-4.
Austin PC. A comparison of 12 algorithms for matching on the propensity score. Stat Med. 2014;33(6):1057–69. https://doi.org/10.1002/sim.6004.
Blom RL, Lagarde SM, van Oudenaarde K, et al. Survival after recurrent esophageal carcinoma has not improved over the past 18 years. Ann Surg Oncol. 2013;20(8):2693–8. https://doi.org/10.1245/s10434-013-2936-3.
Parry K, Visser E, van Rossum PSN, Mohammad NH, Ruurda JP, van Hillegersberg R. Prognosis and treatment after diagnosis of recurrent esophageal carcinoma following esophagectomy with curative intent. Ann Surg Oncol. 2015;22(S3):1292–300. https://doi.org/10.1245/s10434-015-4840-5.
Sudo K, Xiao L, Wadhwa R, et al. Importance of surveillance and success of salvage strategies after definitive chemoradiation in patients with esophageal cancer. J Clin Oncol. 2014;32(30):3400–5. https://doi.org/10.1200/jco.2014.56.7156.
Markar S, Gronnier C, Duhamel A, et al. Salvage surgery after chemoradiotherapy in the management of esophageal cancer: is it a viable therapeutic option? J Clin Oncol. 2015;33(33):3866–73. https://doi.org/10.1200/jco.2014.59.9092.
Sudo K, Wang X, Xiao L, et al. A nomogram to predict distant metastases after multimodality therapy for patients with localized esophageal cancer. J Natl Compr Canc Netw. 2016;14(2):173–9.
Grotenhuis BA, van Hagen P, Reitsma JB, et al. Validation of a nomogram predicting complications after esophagectomy for cancer. Ann Thorac Surg. 2010;90(3):920–5. https://doi.org/10.1016/j.athoracsur.2010.06.024.
Hsieh C-C, Hsu H-S, Chang S-C, Chen Y-J. Circulating cell-dree DNA levels could predict oncological outcomes of patients undergoing esophagectomy for esophageal squamous cell carcinoma. Int J Mol Sci. 2016;17(12):2131. https://doi.org/10.3390/ijms17122131.
Van Rossum PSN, Van Lier ALHMW, Van Vulpen M, et al. Diffusion-weighted magnetic resonance imaging for the prediction of pathologic response to neoadjuvant chemoradiotherapy in esophageal cancer. Radiother Oncol. 2015;115(2):163–70. https://doi.org/10.1016/j.radonc.2015.04.027.
Heethuis SE, van Rossum PSN, Lips IM, et al. Dynamic contrast-enhanced MRI for treatment response assessment in patients with oesophageal cancer receiving neoadjuvant chemoradiotherapy. Radiother Oncol. 2016. https://doi.org/10.1016/j.radonc.2016.05.009.
Iasonos A, Schrag D, Raj G V, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–70. https://doi.org/10.1200/jco.2007.12.9791.
Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD Statement. Ann Intern Med. 2015;162(1):55. https://doi.org/10.7326/m14-0697.
Acknowledgements
Lucas Goense was supported by the René Vogels Foundation, Oirschot, The Netherlands.
Disclosure
SHL received research funding from STCube Pharmaceuticals, Genetech, Peregrine Pharmaceuticals, Hitachi Chemical, and honorarium from AstraZeneca. All other authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Goense, L., van Rossum, P.S.N., Xi, M. et al. Preoperative Nomogram to Risk Stratify Patients for the Benefit of Trimodality Therapy in Esophageal Adenocarcinoma. Ann Surg Oncol 25, 1598–1607 (2018). https://doi.org/10.1245/s10434-018-6435-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6435-4