ABSTRACT
Background
Timely administration of adjuvant chemotherapy for breast cancer is associated with a survival benefit. Specific elements of surgical management may lead to delays initiating chemotherapy, resulting in unfavorable outcomes. The purpose of this study was to determine the correlation between surgical factors and delayed chemotherapy in breast cancer patients.
Methods
A retrospective analysis of the National Cancer Database was performed. The study cohort consisted of female patients with stage 1–3 breast cancer diagnosed between 2010 and 2014. Initiation of chemotherapy beyond 90 days after surgery was defined as delayed. Multivariable logistic regression modeling was performed to establish associations between delayed chemotherapy and clinical and demographic factors of interest. Survival analysis was performed using the Kaplan-Meier estimation and Cox proportional hazards regression to evaluate potential 5-year overall survival disadvantage of delayed initiation of chemotherapy.
Results
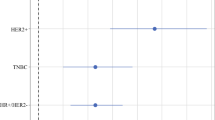
Of 166,681 women assessed, 4.3% had a delay in the initiation of chemotherapy. Surgery-specific risk factors included unplanned readmission in the postoperative period, lower surgical volume, mastectomy with immediate autologous reconstruction, and positive surgical margins. Adjusted survival analysis showed a survival disadvantage of delayed initiation of chemotherapy (hazard ratio [HR] 1.46; p < 0.01).
Conclusions
Risk factors for delayed initiation of chemotherapy specific to the surgical process were identified. Delayed initiation of adjuvant chemotherapy was associated with a survival detriment. Efforts should be made to address these surgical management issues and optimize the perioperative process to ensure timely patient treatment.

Similar content being viewed by others
References
Fisher B, Gunduz N, Saffer EA. Influence of the interval between primary tumor removal and chemotherapy on kinetics and growth of metastases. Cancer Res. 1983;43:1488–92.
Fisher B, Saffer E, Rudock C, Coyie J, Gunduz N. Effect of local or systemic treatment prior to primary tumor removal on the production and response to a serum growth-stimulating factor in mice. Cancer Res. 1989;49:2002–4.
Chavez-MacGregor M, Clarke CA, Lichtensztajn DY, Giordano SH. Delayed initiation of adjuvant chemotherapy among patients with breast cancer. JAMA Oncol. 2016;2(3):322–9. https://doi.org/10.1001/jamaoncol.2015.3856.
Hershman DL, Wang X, McBride R, Jacobson JS, Grann VR, Neugut AI. Delay of adjuvant chemotherapy initiation following breast cancer surgery among elderly women. Breast Cancer Res Treat. 2006;99:313–21. https://doi.org/10.1007/s10549-006-9206-z.
Nurgalieva ZZ, Franzini L, Morgan RO, Vernon SW, Liu CC, Du XL. Impact of timing of adjuvant chemotherapy initiation and completion after surgery on racial disparities in survival among women with breast cancer. Med Oncol. 2013;30(419):1–9. https://doi.org/10.1007/s12032-012-0419-1.
Lohrisch C, Paltiel C, Gelmon K, Speers C, Taylor S, Barnett J. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol. 2017;24(30):4888–94. https://doi.org/10.1200/jco.2005.01.6089.
Yu K-D, Huang S, Zhang J-X, Liu G-Y, Shao Z-M. Association between delayed initiation of adjuvant cmf or anthracycline-based chemotherapy and survival in breast cancer: a systematic review and meta-analysis. BMC Cancer. 2013;13(240):1–10.
Seneviratne S, Campbell I, Scott N, Kuper-hommel M, Round G, Lawrenson R. Ethnic differences in timely adjuvant chemotherapy and radiation therapy for breast cancer in New Zealand: a cohort study. BMC Cancer. 2014;14:839.
Losk K, Vaz-Luis I, Camuso K, Batista R, Lloyd M. Factors associated with delays in chemotherapy initiation among patients with breast cancer at a comprehensive cancer center. J Natl Compr Cancer Netw. 2016;14(12):1519–26.
De Melo Gagliato D, Gonzalez-Angulo AM, Lei X, et al. Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer. J Clin Oncol. 2014;32(8):735–44. https://doi.org/10.1200/jco.2013.49.7693.
Al-Hilli Z, Thomsen KM, Habermann EB, Jakub JW, Boughey JC. Reoperation for complications after lumpectomy and mastectomy for breast cancer from the 2012 National Surgical Quality Improvement Program (ACS-NSQIP). Ann Surg Oncol. 2015;22:459–69. https://doi.org/10.1245/s10434-015-4741-7.
Rubio IT, Ahmed M, Kovacs T, Marco V. Margins in breast conserving surgery: a practice-changing process. Eur J Surg Oncol. 2016;42:631–40. https://doi.org/10.1016/j.ejso.2016.01.019.
Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–37.
Finks JF, Osborne NH, Birkmeyer J. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128–37.
Chen C-S, Liu T-C, Lin H-C, Lien Y-C. Does high surgeon and hospital surgical volume raise the five-year survival rate for breast cancer? A population-based study. Breast Cancer Res Treat. 2008;110:349–56. https://doi.org/10.1007/s10549-007-9715-4.
Greenup RA, Obeng-Gyasi S, Thomas S, et al. The effect of hospital volume on breast cancer mortality. Ann Surg. 2016;267(2):375–81. https://doi.org/10.1097/sla.0000000000002095.
Peltoniemi P, Peltola M, Hakulinen T, Hakkinen U, Pylkkanen L, Holli K. The effect of hospital volume on the outcome of breast cancer surgery. Ann Surg Oncol. 2011;18:1684–90. https://doi.org/10.1245/s10434-010-1514-1.
Vrijens F, Stordeur S, Beirens K, Devriese S, Van Eycken E, Vlayen J. Effect of hospital volume on processes of care and 5-year survival after breast cancer: a population-based study on 25,000 women. The Breast. 2012;21:261–6. https://doi.org/10.1016/j.breast.2011.12.002.
Kong AL, Pezzin LE, Nattinger AB. Identifying patterns of breast cancer care provided at high-volume hospitals: a classification and regression tree analysis. Breast Cancer Res Treat. 2015;153:689–98. https://doi.org/10.1007/s10549-015-3561-6.
Ennis SR, Rios-Vargas M, Albert NG. The Hispanic population: 2010. 2011. https://doi.org/10.1016/j.mhpa.2012.10.005.
Dubard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. Am J Public Health. 2008;98(11):2021–8. https://doi.org/10.2105/ajph.2007.119008.
Gazmararian JA, Baker DW, Williams M V., et al. Health literacy and preventive health care use among medicare enrollees in a managed care organization. JAMA. 1999;281(6):545–51. https://doi.org/10.1097/00005650-200205000-00005.
Sentell T, Braun K. Low health literacy, limited english proficiency, and health status in Asian, Latinos and other racial/ethnic groups in California. J Health Commun. 2012;17(3):82–99. https://doi.org/10.1080/10810730.2012.712621.low.
Weiss BD, Blanchard JS, McGee DL, et al. Illiteracy among Medicaid recipients and its relationship to health care costs. J Health Care Poor Underserv. 1994;5(2):99–111. https://doi.org/10.1353/hpu.2010.0272.
Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–6. https://doi.org/10.1111/j.1525-1497.2005.0174.x.
Acknowledgement
The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed or the conclusions drawn from these data by the investigator.
Disclosure
There is no conflict of interests or financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Riba, L.A., Gruner, R.A., Fleishman, A. et al. Surgical Risk Factors for the Delayed Initiation of Adjuvant Chemotherapy in Breast Cancer. Ann Surg Oncol 25, 1904–1911 (2018). https://doi.org/10.1245/s10434-018-6351-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6351-7