Abstract
Background
Efficacy of preoperative portal vein embolization (PVE) has been established; however, differences of outcomes among diseases, including hepatocellular carcinoma (HCC), biliary tract cancer (BTC), and colorectal liver metastases (CLM), are unclear.
Methods
Subjects included patients in a prospectively collected database undergoing PVE (from 1995 to 2013). A future liver remnant (FLR) volume ≥40% is the minimal requirement for patients with an indocyanine green retention rate at 15 min (ICGR15) <10%, and stricter criteria (FLR volume ≥50%) have been applied for patients with 20% > ICGR15 ≥ 10%. Patient characteristics and survivals were compared among those three diseases, and predictors of dropout and better FLR hypertrophy were determined.
Results
In 319 consecutive patients undergoing PVE for HCC (n = 70), BTC (n = 172), and CLM (n = 77), the degree of hypertrophy did not significantly differ by cancer types (median 10, 9.6, and 10%, respectively). Eighty percent (256 of 319) of patients completed subsequent hepatectomy after a median waiting interval of 24 days (range 5–90), while dropout after PVE was more common in BTC or CLM (odds ratio 2.75, p = 0.018), mainly because of disease progression. Ninety-day liver-related mortality after hepatectomy was 0% in the entire cohort, and 5-year overall survival of patients with HCC, BTC, and CLM was 56, 50, and 51%, respectively (p = 0.948). No patients who dropped out survived more than 2.5 years after PVE.
Conclusion
PVE produced equivalent FLR hypertrophy among the three diseases as long as liver function was fulfilling the preset criteria; however, the completion rate of subsequent hepatectomy was highest in HCC. PVE followed by hepatectomy was a safe and feasible strategy for otherwise unresectable disease irrespective of cancer types.

Similar content being viewed by others
References
Utsunomiya T, Shimada M, Kudo M, et al. Nationwide study of 4741 patients with non-B non-C hepatocellular carcinoma with special reference to the therapeutic impact. Ann Surg. 2014;259:336–45.
Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27:3677–83.
Kishi Y, Abdalla EK, Chun YS, et al. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg. 2009;250:540–8.
Kubota K, Makuuchi M, Kusaka K, et al. Measurement of liver volume and hepatic functional reserve as a guide to decision-making in resectional surgery for hepatic tumors. Hepatology. 1997;26:1176–81.
Ebata T, Yokoyama Y, Igami T, et al. Portal vein embolization before extended hepatectomy for biliary cancer: current technique and review of 494 consecutive embolizations. Dig Surg. 2012;29:23–9.
Makuuchi M, Thai BL, Takayasu K, et al. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 1990;107:521–7.
Kokudo N, Tada K, Seki M, et al. Proliferative activity of intrahepatic colorectal metastases after preoperative hemihepatic portal vein embolization. Hepatology. 2001;34:267–72.
Schadde E, Raptis DA, Schnitzbauer AA, et al. Prediction of mortality after ALPPS stage-1: an analysis of 320 patients from the International ALPPS Registry. Ann Surg. 2015;262:780–6.
Schadde E, Ardiles V, Robles-Campos R, et al. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg. 2014;260:829–38.
Li J, Girotti P, Königsrainer I, et al. ALPPS in right trisectionectomy: a safe procedure to avoid postoperative liver failure? J Gastrointest Surg. 2013;17:956–61.
D’Haese JG, Neumann J, Weniger M, et al. Should ALPPS be used for liver resection in intermediate-stage HCC? Ann Surg Oncol. 2016;23:1335-1343.
Madoff DC, Abdalla EK, Gupta S, et al. Transhepatic ipsilateral right portal vein embolization extended to segment IV: improving hypertrophy and resection outcomes with spherical particles and coils. J Vasc Interv Radiol. 2005;16:215–25.
Nagino M, Kamiya J, Kanai M, et al. Right trisegment portal vein embolization for biliary tract carcinoma: technique and clinical utility. Surgery. 2000;127:155–60.
Yoo H, Kim JH, Ko GY, et al. Sequential transcatheter arterial chemoembolization and portal vein embolization versus portal vein embolization only before major hepatectomy for patients with hepatocellular carcinoma. Ann Surg Oncol. 2011;18:1251–7.
Yokoyama Y, Ebata T, Igami T, et al. The adverse effects of preoperative cholangitis on the outcome of portal vein embolization and subsequent major hepatectomies. Surgery. 2014;156:1190–6.
Shindoh J, Tzeng CW, Aloia TA, et al. Safety and efficacy of portal vein embolization before planned major or extended hepatectomy: an institutional experience of 358 patients. J Gastrointest Surg. 2014;18:45–51.
Yamashita S, Hasegawa K, Takahashi M, et al. One-stage hepatectomy following portal vein embolization for colorectal liver metastasis. World J Surg. 2013;37:622–8.
Aoki T, Imamura H, Hasegawa K, et al. Sequential preoperative arterial and portal venous embolizations in patients with hepatocellular carcinoma. Arch Surg. 2004;139:766–4.
Seyama Y, Kubota K, Sano K, et al. Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg. 2003;238:73–83.
Oba M, Hasegawa K, Shindoh J, et al. Survival benefit of repeat resection of successive recurrences after the initial hepatic resection for colorectal liver metastases. Surgery. 2016;159:632–40.
Imamura H, Shimada R, Kubota M, et al. Preoperative portal vein embolization: an audit of 84 patients. Hepatology. 1999;29:1099–105.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Ishak K, Baptista A, Bianchi L, et al. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22:696–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS) Surgery. 2011;149:713–24.
Miyakawa S, Ishihara S, Horiguchi A, et al. Biliary tract cancer treatment: 5,584 results from the Biliary Tract Cancer Statistics Registry from 1998 to 2004 in Japan. J Hepatobiliary Pancreat Surg. 2009;16:1–7.
Mavros MN, Economopoulos KP, Alexiou VG, et al. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: systematic review and meta-analysis. JAMA Surg. 2014;149:565–574.
Torzilli G, Belghiti J, Kokudo N, et al. A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: is it adherent to the EASL/AASLD recommendations? An observational study of the HCC East-West study group. Ann Surg. 2013;257:929–37.
Oba M, Hasegawa K, Matsuyama Y, et al. Discrepancy between recurrence-free survival and overall survival in patients with resectable colorectal liver metastases: a potential surrogate endpoint for time to surgical failure. Ann Surg Oncol. 2014;21:1817–24.
Shindoh J, Vauthey JN, Zimmitti G, et al. Analysis of the efficacy of portal vein embolization for patients with extensive liver malignancy and very low future liver remnant volume, including a comparison with the associating liver partition with portal vein ligation for staged hepatectomy approach. J Am Coll Surg. 2013; 217:126–34.
Mise Y, Passot G, Wang X, et al. A nomogram to predict hypertrophy of liver segments 2 and 3 after right portal vein embolization. J Gastrointest Surg. 2016;20:1317–23.
Iakova P, Awad SS, Timchenko NA. Aging reduces proliferative capacities of liver by switching pathways of C/EBPalpha growth arrest. Cell. 2003;113:495–506.
Oldhafer KJ, Stavrou GA, van Gulik TM, et al. ALPPS-where do we stand, where do we go? Eight Recommendations from the First International Expert Meeting. Ann Surg. 2016;263:839–41.
Igami T, Ebata T, Yokoyama Y, et al. Portal vein embolization using absolute ethanol: evaluation of its safety and efficacy. J Hepatobiliary Pancreat Sci. 2014;21:676–81.
Farges O, Belghiti J, Kianmanesh R, et al. Portal vein embolization before right hepatectomy: prospective clinical trial. Ann Surg. 2003;237:208–17.
Funding
No grant support or other funding was received in respect of this study.
Disclosure
Suguru Yamashita, Yoshihiro Sakamoto, Satoshi Yamamoto, Nobuyuki Takemura, Kiyohiko Omichi, Hiroji Shinkawa, Kazuhiro Mori, Junichi Kaneko, Nobuhisa Akamatsu, Junichi Arita, Kiyoshi Hasegawa, and Norihiro Kokudo have no conflicts of interest associated with this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
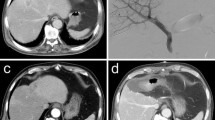
10434_2017_5800_MOESM2_ESM.tif
Supplementary Figure 1. Proposed strategy of portal vein embolization followed by major hepatectomy. A. In patients with hepatocellular carcinoma, selective transcatheter arterial chemoembolization was conducted first to enhance future liver remnant hypertrophy and suppress tumor growth if macroscopic vascular invasion was present. B. In patients with biliary tract cancer, biliary drainage was conducted first if the patient’s condition was compromised by obstructive jaundice. Portal vein embolization was postponed until serum total bilirubin level declined to ≤5.0 mg/dL. C. Upfront surgical resection for initially resectable patients with colorectal liver metastases (CLM) is routinely applied. Patients with technically unresectable CLM at the initial presentation were administered preoperative chemotherapy to convert to technical resectability. (TIFF 3285 kb)
10434_2017_5800_MOESM3_ESM.tif
Supplementary Figure 2. Comparison of total liver volume and indocyanine green retention rate at 15 min before and after portal vein embolization. A. Total liver volume did not significantly differ between pre- and post-portal vein embolization on analysis of the entire cohort or according to disease diagnosis. Median values (horizontal line within each box), interquartile ranges (boxes), and ranges (error bars) are shown. B. Indocyanine green retention rate at 15 min did not significantly differ between pre- and post-portal vein embolization on analysis of the entire cohort or according to disease diagnosis. Median values (horizontal line within each box), interquartile ranges (boxes), and ranges (error bars) are shown. (TIFF 123 kb)
Rights and permissions
About this article
Cite this article
Yamashita, S., Sakamoto, Y., Yamamoto, S. et al. Efficacy of Preoperative Portal Vein Embolization Among Patients with Hepatocellular Carcinoma, Biliary Tract Cancer, and Colorectal Liver Metastases: A Comparative Study Based on Single-Center Experience of 319 Cases. Ann Surg Oncol 24, 1557–1568 (2017). https://doi.org/10.1245/s10434-017-5800-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5800-z