Abstract
Background and Objective
There is variability in physician practice regarding delivery method and timeliness of test results to cancer patients. Our aim was to survey patients to determine if there was a difference between actual and preferred care for disclosure of test results.
Methods
A de-identified survey was distributed to online cancer support groups to query patients about their experience regarding communication of cancer testing and timeliness. Analyses of the differences between actual and preferred communication and wait times were performed.
Results
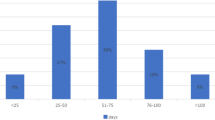
Overall, 1000 patients completed the survey. The analysis herein was restricted to 784 breast cancer survivors. Survey responders were predominately White (non-Hispanic; 89 %), college educated (78 %), and media ‘savvy’ (online medical media usage; 97 %). Differences between actual and preferred care were identified for the domains of mode of communication and wait times for initial breast cancer diagnostic biopsies and other tests. A total of 309 (39 %) of 784 patients received face-to-face communication for a new cancer diagnosis, with 394 (50 %) patients preferring this option (p < 0.0001). In addition, 315 (40 %) of 784 patients received their cancer biopsy result within 2 days, with 646 (82 %) patients preferring this option (p < 0.0001). Differences were also identified between actual and preferred care for multiple other test types.
Conclusions
Actual care for timeliness and modes of communication did not reflect patient-desired care. National and local initiatives to improve performance are needed. As a first step, we recommend that each patient be queried about their preference for mode of communication and timeliness, and efforts made to comply.
Similar content being viewed by others
References
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES—a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–11.
Rose C, Stovall E, Ganz PA, Desch C, Hewitt M. Cancer Quality Alliance: blueprint for a better cancer care system. CA Cancer J Clin. 2008;58(5):266–92.
Purnell CA, Arnold RM. Retrospective analysis of communication with patients undergoing radiological breast biopsy. J Support Oncol. 2010;8(6):259–63.
Butow PN, Kazemi JN, Beeney LJ, Griffin A, Dunn SM, Tattersall MHN. When the diagnosis is cancer: patient communication experiences and preferences. Cancer. 1996;77(12):2630–7.
Choudhry A, Hong J, Chong K, et al. Patients’ preferences for biopsy result notification in an era of electronic messaging methods. JAMA Dermatol. 2015;151(5):513–20.
Figg WD, Smith EK, Price DK, English BC, Thurman PW, Steinberg SM, et al. Disclosing a diagnosis of cancer: where and how does it occur? J Clin Oncol. 2010;28(22):3630–5.
Salber P. How docs give us the bad news. The doctor weighs in (blog). 2010. http://thedoctorweighsin.com/how-docs-give-us-the-bad-news/. Accessed 6 Mar 2016.
The American Society of Breast Surgeons Mastery of Breast Surgery (2015). Quality Measurement Program and Breast Surgeons Forum. https://www.breastsurgeons.org/new_layout/programs/mastery/. Accessed 19 Apr 2016.
Institute of Medicine (2001). Crossing the quality chasm: a new health system for the 21st century. National Academy Press; 2001. http://www.nap.edu/read/10027/chapter/1. Accessed 6 Mar 2016.
Institute for Healthcare Improvement (2016). The IHI triple aim: improving the patient experience. http://www.ihi.org/engage/initiatives/TripleAim/Pages/default.aspx. Accessed 6 Mar 2016.
Agency for Healthcare Research and Quality. Person and family partnerships and effective communication as part of the six priorities of the National Quality Strategy (NQS). 2016. http://www.ahrq.gov/workingforquality/. Accessed 6 Mar 2016.
National Quality Forum. Importance criteria and identifying a performance gap by variation of care. http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwjBtKbDgtLLAhXGNT4KHYBFAYQQFggcMAA&url=http%3A%2F%2Fwww.qualityforum.org%2Fdocs%2FMeasure_Evaluation_Criteria_Guidance.aspx&usg=AFQjCNF2d2f3UIhxRdFXkGFqNeP0EGgNHg. Accessed 6 Mar 2016.
Gundersen Health System. Patient portal for communication test results ‘My Care’. 2016. http://www.gundersenhealth.org/mycare/information. Accessed 6 Mar 2016.
Landercasper J, Linebarger JH, Ellis RL, et al. A quality review of the timeliness of breast cancer diagnosis and treatment in an integrated breast center. J Am Coll Surg. 2010;210(4):449–55.
Berman A, Teig B, Duracinsky M, et al. One day diagnosis for breast lesions: medical and psychological assessment—EVADIASEIN study [in French]. J Gynecol Obstet Biol Reprod (Paris). 2016;45(1):21–8.
Barentsz MW, Wessels H, van Diest PJ, et al. Same-day diagnosis based on histology for women suspected of breast cancer: high diagnostic accuracy and favorable impact on the patient. PLoS One. 2014;9(7):e103–5.
Krishnan N, Fagerlin A, Skolarus TA. Rethinking patient-physician communication of biopsy results: the waiting game. JAMA Oncol. 2015;1(8):1025–6.
Fayanju OM, Mayo TL, Spinks TE, et al. Value-based breast cancer care: a multidisciplinary approach for defining patient-centered outcomes. Ann Surg Oncol. 2016;94(4):719–28.
Bleicher RJ, Ruth K, Sigurdson ER, et al. Time to surgery and breast cancer survival in the United States. JAMA Oncol. 2016;2(3):330–9.
Atisha DM, Rushing CN, Samsa GP, et al. A national snapshot of satisfaction with breast cancer procedures. Ann Surg Oncol. 2015;22:361–9.
Acknowledgment
The authors would like to acknowledge the Norma J. Vinger Center for Breast Care, the Gundersen Medical Foundation, and Ms. Choua Vang for financial support, statistical support, and manuscript assistance, respectively. In addition, we would like to acknowledge the Dr. Susan Love Research Foundation, the Seattle Cancer Care Alliance, and Living Beyond Breast Cancer for assistance with distributing the survey using their social media channels.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Attai, D.J., Hampton, R., Staley, A.C. et al. What Do Patients Prefer? Understanding Patient Perspectives on Receiving a New Breast Cancer Diagnosis. Ann Surg Oncol 23, 3182–3189 (2016). https://doi.org/10.1245/s10434-016-5312-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5312-2