Abstract
Background
Many attempts to prevent lymphatic complications following therapeutic lymph node dissection (TLND) have included modifications in surgical techniques through the use of ultrasonic scalpels (USS) or lymphostatic agents. Previous randomized studies that enrolled heterogeneous groups of patients attempted to confirm the efficacy of such techniques. The aim of the present study was to evaluate the efficacy of the USS following TLND.
Methods
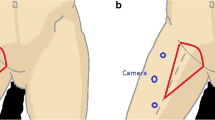
Between 2009 and 2013, patients undergoing inguinal or axillary TLND or completion lymph node dissection after positive sentinel lymph node biopsy for melanoma, squamous cell carcinoma or sarcoma were randomized into two surgical dissection technique groups. In the USS dissection arm, surgery was conducted using a USS. These were compared with a control group whereby ligation and monopolar electrocautery was utilized. For axillary dissection, a standardized level III lymphadenectomy was performed. A complete inguinal lymphadenectomy including Cloquet’s node was performed, and at the end of the procedure a Redon suction drain was routinely placed in the axilla and groin. The primary endpoint was to compare the time to drain removal in both groups, while the secondary endpoint was to evaluate the rate of complications (infection, fistula, lymphocele formation, wound dehiscence, lymphedema) between the two groups.
Results
A total of 80 patients were enrolled in this trial; 40 patients were randomly assigned to both the USS group and the control (C) group. No significant differences were observed in terms of duration of drainage (USS: 31 ± 20 vs. C: 32 ± 18; p = 0.83); however, a significantly increased rate of lymphedema (defined as an increased circumference of the operated limb of more than 10 %) was identified in the USS group (USS: 50 % vs. C: 27.5 %; p = 0.04). No other significant differences were recorded for postoperative complications, including surgical site infection (USS: 5 % vs. C: 7.5 %; p = 0.68), lymphatic fistula (USS: 5 % vs. C: 2.5 %; p = 0.62), lymphocele (USS: 32.5 % vs. C: 22.5 %; p = 0.33), and hematoma (USS: 5 % vs. C: 2.5 %; p = 0.62).
Conclusion
The use of USS failed to offer any significant reduction in length of drain usage and operative complication, but it seems to increase the rate of lymphedema formation.
Similar content being viewed by others
References
Veronesi U, et al. Delayed regional lymph node dissection in stage I melanoma of the skin of the lower extremities. Cancer. 1982;49(11):2420–30.
Balch CM, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27(36):6199–206.
Balch CM, et al. Multivariate analysis of prognostic factors among 2,313 patients with stage III melanoma: comparison of nodal micrometastases versus macrometastases. J Clin Oncol. 2010;28(14):2452–9.
Litrowski N, et al. Complication of radical lymph node dissection following sentinel lymph node biopsy in patients with melanoma [in French]. Ann Dermatol Venereol. 2013;140(6-7):425–30.
Porter KA, et al. Electrocautery as a factor in seroma formation following mastectomy. Am J Surg. 1998;176(1):8–11.
Gauthier T, et al. Lanreotide autogel 90 mg and lymphorrhea prevention after axillary node dissection in breast cancer: a phase III double blind, randomized, placebo-controlled trial. Eur J Surg Oncol. 2012;38(10):902–9.
Judson PL, et al. A prospective, randomized study analyzing sartorius transposition following inguinal-femoral lymphadenectomy. Gynecol Oncol. 2004;95(1):226–30.
Lumachi F, et al. Ultrasonic dissection system technology in breast cancer: a case-control study in a large cohort of patients requiring axillary dissection. Breast Cancer Res Treat. 2013;142(2):399–404.
Iovino F, et al. Preventing seroma formation after axillary dissection for breast cancer: a randomized clinical trial. Am J Surg. 2012;203(6):708–14.
Adwani A, Ebbs SR. Ultracision reduces acute blood loss but not seroma formation after mastectomy and axillary dissection: a pilot study. Int J Clin Pract. 2006;60(5):562–4.
Pellegrino A, et al. Harmonic scalpel versus conventional electrosurgery in the treatment of vulvar cancer. Int J Gynaecol Obstet. 2008;103(2):185–8.
Petrek JA, Pressman PI, Smith RA. Lymphedema: current issues in research and management. CA Cancer J Clin. 2000;50(5):292–307. quiz 308-11.
Clark B, Sitzia J, Harlow W. Incidence and risk of arm oedema following treatment for breast cancer: a three-year follow-up study. QJM. 2005;98(5):343–8.
Mangram AJ, et al. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20(4):250–78; quiz 279-80.
He Q, et al. Harmonic focus versus electrocautery in axillary lymph node dissection for breast cancer: a randomized clinical study. Clin Breast Cancer. 2012;12(6):454–8.
Sanguinetti A, et al. Ultrasound scissors versus electrocautery in axillary dissection: our experience. G Chir. 2010;31(4):151–3.
Manjunath S, et al. Ultrasonic shears versus electrocautery in axillary dissection for breast cancer: a randomized controlled trial. Indian J Surg Oncol. 2014;5(2):95–8.
Ko E, et al. Fibrin glue reduces the duration of lymphatic drainage after lumpectomy and level II or III axillary lymph node dissection for breast cancer: a prospective randomized trial. J Korean Med Sci. 2009;24(1):92–6.
Abe K, et al. Experimental evaluation of bursting pressure in lymphatic vessels with ultrasonically activated shears. World J Surg. 2005;29(1):106–9.
Kajiyama Y, et al. Sealing the thoracic duct with ultrasonic coagulating shears. Hepatogastroenterology. 2005;52(64):1053–6.
Nakayama H, et al. Ultrasonic scalpel for sealing of the thoracic duct: evaluation of effectiveness in an animal model. Interact Cardiovasc Thorac Surg. 2009;9(3):399–401.
Tsimoyiannis EC, et al. Ultrasonically activated shears in extended lymphadenectomy for gastric cancer. World J Surg. 2002;26(2):158–61.
Disclosures
No industry sponsorship was received for this study. Marie-Laure Matthey-Gié, Olivier Gié, Sona Deretti, Nicolas Demartines, and Maurice Matter disclose no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matthey-Gié, ML., Gié, O., Deretti, S. et al. Prospective Randomized Study to Compare Lymphocele and Lymphorrhea Control Following Inguinal and Axillary Therapeutic Lymph Node Dissection With or Without the Use of an Ultrasonic Scalpel. Ann Surg Oncol 23, 1716–1720 (2016). https://doi.org/10.1245/s10434-015-5025-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-5025-y