Abstract
Background
Data on the importance of margin status after total thyroidectomy for papillary thyroid cancer (PTC) remain limited. This study sought to identify factors associated with positive margins and to determine the impact of positive margins on survival for patients with PTC.
Methods
The National Cancer Data Base (1998–2006) was queried for patients with PTC who had undergone total thyroidectomy. The patients were divided into three groups based on margin status (negative, microscopically positive, and macroscopically positive). Patient demographic, clinical, and pathologic features were evaluated. A binary logistic regression model was developed to identify factors associated with positive margins. A Cox proportional hazards model was developed to identify factors associated with survival.
Results
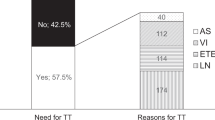
Of the 31,129 patients enrolled in the study, 91.3 % had negative margins, 8.1 % had microscopically positive margins, and 0.6 % had macroscopically positive margins. The patients with negative margins were younger and more likely to be female, white, covered by private insurance, and treated at an academic or high-volume center (p < 0.05). They had smaller tumors and were less likely to have advanced-stage disease. After multivariable adjustment, increasing patient age [odds ratio (OR) = 1.02; p < 0.01], government insurance (OR = 1.20; p < 0.01), and no insurance (OR = 1.34; p = 0.01) were associated with positive margins. Reception of surgery at a high-volume facility (OR = 0.72; p < 0.01) was protective. After multivariable adjustment, both microscopically [hazard ratio (HR), 1.49; p < 0.01] and macroscopically positive margins (HR = 2.38; p < 0.01) were associated with compromised survival.
Conclusions
Several vulnerable patient populations have a higher risk of incomplete resection after thyroidectomy for PTC. High-risk thyroid cancer patients should be referred to high-volume centers to optimize outcomes.

Similar content being viewed by others
References
American Cancer Society. Cancer Facts & Figures. 2013. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf. Retrieved 2 Mar 2015.
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64:252–71.
Davies L, Welch HG. Thyroid cancer survival in the United States: observational data from 1973 to 2005. Arch Otolaryngol Head Neck Surg. 2010;136:440–4.
Konstantinidis IT, Warshaw AL, Allen JN, Blaszkowsky LS, Castillo CF, Deshpande V, et al. Pancreatic ductal adenocarcinoma: is there a survival difference for R1 resections versus locally advanced unresectable tumors? What is a “true” R0 resection? Ann Surg. 2013;257:731–6.
Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, et al. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst. 2001;93:583–96.
Harness JK, Giuliano AE, Pockaj BA, Downs-Kelly E. Margins: a status report from the Annual Meeting of the American Society of Breast Surgeons. Ann Surg Oncol. 2014;21:3192–7.
Chiappa C, Rovera F, Corben AD, Fachinetti A, De Berardinis V, Marchionini V, et al. Surgical margins in breast conservation. Int J Surg. 2013;11(Suppl 1):S69–72.
Behm EC, Beckmann KR, Dahlstrom JE, Zhang Y, Cho C, Stuart-Harris R, et al. Surgical margins and risk of locoregional recurrence in invasive breast cancer: an analysis of 10-year data from the Breast Cancer Treatment Quality Assurance Project. Breast Edinburgh, Scotland. 2013;22:839–44.
Nishida T, Nakao K, Hashimoto T. Local control in differentiated thyroid carcinoma with extrathyroidal invasion. Am J Surg. 2000;179:86–91.
Radowsky JS, Howard RS, Burch HB, Stojadinovic A. Impact of degree of extrathyroidal extension of disease on papillary thyroid cancer outcome. Thyroid. 2014;24:241–4.
Raval MV, Bilimoria KY, Stewart AK, Bentrem DJ, Ko CY. Using the NCDB for cancer care improvement: an introduction to available quality assessment tools. J Surg Oncol. 2009;99:488–90.
Phillips JK, Stewart AK, editors. Facility oncology data standards. Commission on Cancer, Chicago, IL, 2006.
Bilimoria KY, Bentrem DJ, Ko CY, Ritchey J, Stewart AK, Winchester DP, et al. Validation of the 6th edition AJCC pancreatic cancer staging system: report from the National Cancer Database. Cancer. 2007;110:738–44.
Chu DI, Moreira DM, Gerber L, Presti JC Jr, Aronson WJ, Terris MK, et al. Effect of race and socioeconomic status on surgical margins and biochemical outcomes in an equal-access health care setting: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. Cancer. 2012;118:4999–5007.
Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228:320–30.
Hauch A, Al-Qurayshi Z, Randolph G, Kandil E. Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol. 2014;21:3844–52.
Reames BN, Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and operative mortality in the modern era. Ann Surg. 2014;260:244–51.
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214.
Phlips P, Hanzen C, Andry G, Van Houtte P, Fruuling J. Postoperative irradiation for thyroid cancer. Eur J Surg Oncol. 1993;19:399–404.
O’Connell ME, A’Hern RP, Harmer CL. Results of external beam radiotherapy in differentiated thyroid carcinoma: a retrospective study from the Royal Marsden Hospital. Eur J Cancer. 1994;30a:733–9.
Farahati J, Reiners C, Stuschke M, Muller SP, Stuben G, Sauerwein W, et al. Differentiated thyroid cancer: impact of adjuvant external radiotherapy in patients with perithyroidal tumor infiltration (stage pT4). Cancer. 1996;77:172–80.
Keum KC, Suh YG, Koom WS, Cho JH, Shim SJ, Lee CG, et al. The role of postoperative external-beam radiotherapy in the management of patients with papillary thyroid cancer invading the trachea. Int J Radiat Oncol Biol Phys. 2006;65:474–80.
Meadows KM, Amdur RJ, Morris CG, Villaret DB, Mazzaferri EL, Mendenhall WM. External beam radiotherapy for differentiated thyroid cancer. Am J Otolaryngol. 2006;27:24–8.
Disclosure
There are no conflicts of interest. The data used in the study were derived from a de-identified National Cancer Data Base (NCDB) file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology used or the conclusions drawn from these data by the investigators.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Youngwirth, L.M., Adam, M.A., Scheri, R.P. et al. Patients Treated at Low-Volume Centers have Higher Rates of Incomplete Resection and Compromised Outcomes: Analysis of 31,129 Patients with Papillary Thyroid Cancer. Ann Surg Oncol 23, 403–409 (2016). https://doi.org/10.1245/s10434-015-4867-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4867-7