Abstract
Background
Management and outcomes of patients with recurrent intrahepatic cholangiocarcinoma (ICC) following curative-intent surgery are not well documented. We sought to characterize the treatment of patients with recurrent ICC and define therapy-specific outcomes.
Methods
Patients who underwent surgery for ICC from 1990 to 2013 were identified from an international database. Data on clinicopathological characteristics, operative details, recurrence, and recurrence-related management were recorded and analyzed.
Results
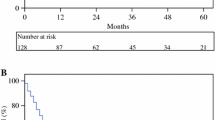
A total of 563 patients undergoing curative-intent hepatic resection for ICC who met the inclusion criteria were identified. With a median follow-up of 19 months, 400 (71.0 %) patients developed a recurrence. At initial surgery, treatment was resection only (98.8 %) or resection + ablation (1.2 %). Overall 5-year survival was 23.6 %; 400 (71.0 %) patients recurred with a median disease-free survival of 11.2 months. First recurrence site was intrahepatic only (59.8 %), extrahepatic only (14.5 %), or intra- and extrahepatic (25.7 %). Overall, 210 (52.5 %) patients received best supportive care (BSC), whereas 190 (47.5 %) patients received treatment, such as systemic chemotherapy-only (24.2 %) or repeat liver-directed therapy ± systemic chemotherapy (75.8 %). Repeat liver-directed therapy consisted of repeat hepatic resection ± ablation (28.5 %), ablation alone (18.7 %), and intra-arterial therapy (IAT) (52.8 %). Among patients who recurred, median survival from the time of the recurrence was 11.1 months (BSC 8.0 months, systemic chemotherapy-only 16.8 months, liver-directed therapy 18.0 months). The median survival of patients undergoing resection of recurrent ICC was 26.7 months versus 9.6 months for patients who had IAT (p < 0.001).
Conclusions
Recurrence following resection of ICC was common, occurring in up to two-thirds of patients. When there is recurrence, prognosis is poor. Only 9 % of patients underwent repeat liver resection after recurrence, which offered a modest survival benefit.


Similar content being viewed by others
References
Aljiffry M, Abdulelah A, Walsh M, Peltekian K, Alwayn I, Molinari M. Evidence-based approach to cholangiocarcinoma: a systematic review of the current literature. J Am Coll Surg. 2009;208(1):134–47.
Khan SA, Toledano MB, Taylor-Robinson SD. Epidemiology, risk factors, and pathogenesis of cholangiocarcinoma. HPB. 2008;10(2):77–82.
Shaib YH, Davila JA, McGlynn K, El-Serag HB. Rising incidence of intrahepatic cholangiocarcinoma in the United States: a true increase? J Hepatol. 2004;40(3):472–7.
Patel T. Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States. Hepatology. 2001;33(6):1353–7.
Mavros MN, Economopoulos KP, Alexiou VG, Pawlik TM. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: systematic review and meta-analysis. JAMA Surg. 2014. doi:10.1001/jamasurg.2013.5137.
Weber SM, Jarnagin WR, Klimstra D, DeMatteo RP, Fong Y, Blumgart LH. Intrahepatic cholangiocarcinoma: resectability, recurrence pattern, and outcomes. J Am Coll Surg. 2001;193(4):384–91.
Amini N, Ejaz A, Spolverato G, Kim Y, Herman JM, Pawlik TM. Temporal trends in liver-directed therapy of patients with intrahepatic cholangiocarcinoma in the United States: a population-based analysis. J Surg Oncol. 2014;110(2):163–70. doi:10.1002/jso.23605.
Farges O, Fuks D, Boleslawski E, et al. Influence of surgical margins on outcome in patients with intrahepatic cholangiocarcinoma: a multicenter study by the AFC-IHCC-2009 study group. Ann Surg. 2011;254(5):824–9; discussion 830.
de Jong MC, Nathan H, Sotiropoulos GC, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol. 2011;29(23):3140–5.
Nuzzo G, Giuliante F, Ardito F, et al. Intrahepatic cholangiocarcinoma: prognostic factors after liver resection. Updates Surg. 2010;62(1):11–9.
Chen LP, Li C, Wang C, Wen TF, Yan LN, Li B. Predictive factors of recurrence for patients with intrahepatic cholangiocarcinoma after hepatectomy. Hepato-gastroenterol. 2012;59(118):1765–8.
Hanazaki K, Kajikawa S, Shimozawa N, et al. Prognostic factors of intrahepatic cholangiocarcinoma after hepatic resection: univariate and multivariate analysis. Hepato-gastroenterol. 2002;49(44):311–6.
Endo I, Gonen M, Yopp AC, et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg. 2008;248(1):84–96.
Miwa S, Miyagawa S, Kobayashi A, et al. Predictive factors for intrahepatic cholangiocarcinoma recurrence in the liver following surgery. J Gastroenterol. 2006;41(9):893–900.
Hyder O, Hatzaras I, Sotiropoulos GC, et al. Recurrence after operative management of intrahepatic cholangiocarcinoma. Surgery. 2013;153(6):811–8.
Kneuertz PJ, Cosgrove DP, Cameron AM, et al. Multidisciplinary management of recurrent hepatocellular carcinoma following liver transplantation. J Gastrointest Surg. 2012;16(4):874–81.
de Jong MC, Mayo SC, Pulitano C, et al. Repeat curative intent liver surgery is safe and effective for recurrent colorectal liver metastasis: results from an international multi-institutional analysis. J Gastrointest Surg. 2009;13(12):2141–51.
Maeda T, Hashimoto K, Ishida T, et al. Repeat hepatectomy for intrahepatic recurrence of cholangiolocellular carcinoma. Fukuoka igaku zasshi = Hukuoka acta medica. 2013;104(12):564–8.
Edge SB BD, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual (7th edn). 2010.
Mayo SC, Shore AD, Nathan H, et al. Refining the definition of perioperative mortality following hepatectomy using death within 90 days as the standard criterion. HPB. 2011;13(7):473–82.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Arnaoutakis DJ, Mavros MN, Shen F, et al. Recurrence patterns and prognostic factors in patients with hepatocellular carcinoma in noncirrhotic liver: a multi-institutional analysis. Ann Surg Oncol. 2014;21(1):147–54.
Spolverato G, Ejaz A, Kim Y, et al. Rates and patterns of recurrence after curative intent resection for gastric cancer: a United States multi-institutional analysis. J Am Coll Surg. 2014;219(4):664–75. doi:10.1016/j.jamcollsurg.2014.03.062.
de Jong MC, Pulitano C, Ribero D, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009;250(3):440–8.
Amini N, Ejaz A, Spolverato G, Maithel SK, Kim Y, Pawlik TM. Management of lymph nodes during resection of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: a systematic review. J Gastrointest Surg. 2014;18(12):2136–48.
Adachi T, Eguchi S, Beppu T, et al. Prognostic impact of preoperative lymph node enlargement in intrahepatic cholangiocarcinoma: a multi-institutional study by the Kyushu Study Group of Liver Surgery. Ann Surg Oncol. 2015;22:2269–78. doi:10.1245/s10434-014-4239-8.
Guglielmi A, Ruzzenente A, Campagnaro T, et al. Patterns and prognostic significance of lymph node dissection for surgical treatment of perihilar and intrahepatic cholangiocarcinoma. J Gastrointest Surg. 2013;17(11):1917–28.
Hyder O, Marsh JW, Salem R, et al. Intra-arterial therapy for advanced intrahepatic cholangiocarcinoma: a multi-institutional analysis. Ann Surg Oncol. 2013;20(12):3779–86.
Acknowledgments
The authors thank Donielle Neal, Susana Rodrigues, John Miura, Francesca Ratti, Timothy Newhook, Malcolm H. Squires, and Stéphanie Meyer.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Spolverato, G., Kim, Y., Alexandrescu, S. et al. Management and Outcomes of Patients with Recurrent Intrahepatic Cholangiocarcinoma Following Previous Curative-Intent Surgical Resection. Ann Surg Oncol 23, 235–243 (2016). https://doi.org/10.1245/s10434-015-4642-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4642-9