Abstract
Background
Hypocalcemia occurs after total thyroidectomy (TT) for Graves disease via parathyroid injury and/or from increased bone turnover. Current management is to supplement calcium after surgery. This study evaluates the impact of preoperative calcium supplementation on hypocalcemia after Graves TT.
Methods
A prospective study of patients with Graves disease undergoing TT was performed. Patients with Graves disease managed over a 9-month period took 1 g of calcium carbonate (CC) three times a day for 2 weeks before TT. Those managed the previous year without supplementation served as historic controls. Age-, gender-, and thyroid weight-matched, non-Graves TT patients were procedure controls. Patient demographics, postoperative laboratory values, complaints, and medications were reviewed. Parathyroid hormone (PTH)-based postoperative protocols dictated postoperative CC and calcitriol use.
Results
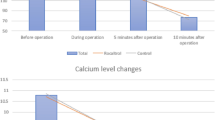
Forty-five patients with Graves disease were treated with CC before TT, and 38 patients with Graves disease were not. Forty control subjects without Graves disease were identified. Age, gender, and thyroid weight were comparable. Preoperative calcium and PTH levels were equivalent. PTH values immediately after surgery, at postoperative day 1, and at 2-week follow-up were equivalent. Postoperative use of scheduled CC (p = 0.10) and calcitriol (p = 0.60) was similar. Postoperatively, patients with untreated Graves disease had lower serum calcium levels than pretreated patients with Graves disease or control subjects without Graves disease (8.3 mg/dL vs. 8.6 vs. 8.6, p = 0.05). Complaints of numbness and tingling were more common in nontreated Graves disease (26 %) than in pretreated Graves disease (9 %) or in control subjects without Graves disease (10 %, p < 0.05).
Conclusions
Calcium supplementation before TT for Graves disease significantly reduced biochemical and symptomatic postoperative hypocalcemia. Preoperative calcium supplementation is a simple treatment that can reduce symptoms of hypocalcemia after Graves TT.

Similar content being viewed by others
References
Hallgrimsson P, Nordenstrom E, Bergenfelz A, Almquist M. Hypocalcaemia after total thyroidectomy for Graves’ disease and for benign atoxic multinodular goitre. Langenbecks Arch Surg. 2012;397:1133–7.
Grodski S, Lundgren CI, Sidhu S, Sywak M, Delbridge L. Postoperative PTH measurement facilitates day 1 discharge after total thyroidectomy. Clin Endocrinol. 2009;70:322–5.
Sywak MS, Palazzo FF, Yeh M, et al. Parathyroid hormone assay predicts hypocalcaemia after total thyroidectomy. ANZ J Surg. 2007;77:667–70.
McCullough M, Weber C, Leong C, Sharma J. Safety, efficacy, and cost savings of single parathyroid hormone measurement for risk stratification after total thyroidectomy. Am Surg. 2013;79:768–74.
Thomusch O, Machens A, Sekulla C, Ukkat J, Brauckhoff M, Dralle H. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: a multivariate analysis of 5846 consecutive patients. Surgery. 2003;133:180–5.
Wang TS, Cheung K, Roman SA, Sosa JA. To supplement or not to supplement: a cost-utility analysis of calcium and vitamin D repletion in patients after thyroidectomy. Ann Surg Oncol. 2011;18:1293–9.
Mazeh H, Khan Q, Schneider DF, Schaefer S, Sippel RS, Chen H. Same-day thyroidectomy program: eligibility and safety evaluation. Surgery. 2012;152:1133–41.
Carter Y, Chen H, Sippel RS. An intact parathyroid hormone-based protocol for the prevention and treatment of symptomatic hypocalcemia after thyroidectomy. J Surg Res. 2014;186:23–8.
Burch HB, Burman KD, Cooper DS. A 2011 survey of clinical practice patterns in the management of Graves’ disease. J Clin Endocrinol Metab. 2012;97:4549–58.
BahnChair RS, Burch HB, Cooper DS, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011;21:593–646.
Yamashita H, Noguchi S, Murakami T, et al. Predictive risk factors for postoperative tetany in female patients with Graves’ disease. J Am Coll Surg. 2001;192:465–8.
Pesce CE, Shiue Z, Tsai HL, et al. Postoperative hypocalcemia after thyroidectomy for Graves’ disease. Thyroid. 2010;20:1279–83.
Welch KC, McHenry CR. Total thyroidectomy: is morbidity higher for Graves’ disease than nontoxic goiter? J Surg Res. 2011;170:96–9.
Snyder S, Govednik C, Lairmore T, Jiang DS, Song J. Total thyroidectomy as primary definitive treatment for Graves’ hyperthyroidism. Am Surg. 2013;79:1283–8.
Kisakol G, Kaya A, Gonen S, Tunc R. Bone and calcium metabolism in subclinical autoimmune hyperthyroidism and hypothyroidism. Endocr J. 2003;50:657–61.
Lal G, Ituarte P, Kebebew E, Siperstein A, Duh QY, Clark OH. Should total thyroidectomy become the preferred procedure for surgical management of Graves’ disease? Thyroid. 2005;15:569–74.
Wilhelm SM, McHenry CR. Total thyroidectomy is superior to subtotal thyroidectomy for management of Graves’ disease in the United States. World J Surg. 2010;34:1261–4.
Murray SE, Sippel RS, Chen H. Incidence of concomitant hyperparathyroidism in patients with thyroid disease requiring surgery. J Surg Res. 2012;178:264–7.
Langley RW, Burch HB. Perioperative management of the thyrotoxic patient. Endocrinol Metab Clin North Am. 2003;32:519–34.
Yamashita H, Noguchi S, Murakami T, et al. Calcium and its regulating hormones in patients with Graves’ disease: sex differences and relation to postoperative tetany. Eur J Surg. 2000;166:924–8.
Thomusch O, Machens A, Sekulla C, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg. 2000;24:1335–41.
Rafferty MA, Goldstein DP, Rotstein L, et al. Completion thyroidectomy versus total thyroidectomy: is there a difference in complication rates? An analysis of 350 patients. J Am Coll Surg. 2007;205:602–7.
Erbil Y, Ozluk Y, Giris M, et al. Effect of lugol solution on thyroid gland blood flow and microvessel density in the patients with Graves’ disease. J Clin Endocrinol Metab. 2007;92:2182–9.
Shinall MC, Jr., Broome JT, Baker A, Solorzano CC. Is potassium iodide solution necessary before total thyroidectomy for Graves’ disease? Ann Surg Oncol. 2013;20:2964–7.
In H, Pearce EN, Wong AK, Burgess JF, McAneny DB, Rosen JE. Treatment options for Graves’ disease: a cost-effectiveness analysis. J Am Coll Surg. 2009;209:170–9.e171–2.
Liu J, Bargren A, Schaefer S, Chen H, Sippel RS. Total thyroidectomy: a safe and effective treatment for Graves’ disease. J Surg Res. 2011;168:1–4.
Yip J, Lang BH, Lo CY. Changing trend in surgical indication and management for Graves’ disease. Am J Surg. 2012;203:162–7.
Genovese BM, Noureldine SI, Gleeson EM, Tufano RP, Kandil E. What is the best definitive treatment for Graves’ disease? A systematic review of the existing literature. Ann Surg Oncol. 2013;20:660–7.
Alexander EK, Larsen PR. High dose of (131)I therapy for the treatment of hyperthyroidism caused by Graves’ disease. J Clin Endocrinol Metab. 2002;87:1073–7.
Torring O, Tallstedt L, Wallin G, et al. Graves’ hyperthyroidism: treatment with antithyroid drugs, surgery, or radioiodine—a prospective, randomized study. Thyroid Study Group. J Clin Endocrinol Metab. 1996;81:2986–93.
Takata K, Kubota S, Fukata S, et al. Methimazole-induced agranulocytosis in patients with Graves’ disease is more frequent with an initial dose of 30 mg daily than with 15 mg daily. Thyroid. 2009;19:559–63.
Ljunggren JG, Torring O, Wallin G, et al. Quality of life aspects and costs in treatment of Graves’ hyperthyroidism with antithyroid drugs, surgery, or radioiodine: results from a prospective, randomized study. Thyroid. 1998;8:653–9.
Stavrakis AI, Ituarte PH, Ko CY, Yeh MW. Surgeon volume as a predictor of outcomes in inpatient and outpatient endocrine surgery. Surgery. 2007;142:887–99.
Oltmann SC, Schneider DF, Leverson G, Sivashanmugam T, Chen H, Sippel RS. Radioactive iodine remnant uptake after completion thyroidectomy: not such a complete cancer operation. Ann Surg Oncol. 2014;21:1379–83.
Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228:320–30.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oltmann, S.C., Brekke, A.V., Schneider, D.F. et al. Preventing Postoperative Hypocalcemia in Patients with Graves Disease: A Prospective Study. Ann Surg Oncol 22, 952–958 (2015). https://doi.org/10.1245/s10434-014-4077-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4077-8