Abstract
Keratin has the potential to function as the gel matrix in an ophthalmic formulation for the encapsulation of the macrolide antibiotic azithromycin. The quality of this formulation was thoroughly evaluated through various analyses, such as in vitro release assessment, rheological examination, intraocular retention studies in rabbits, assessment of bacteriostatic efficacy, and safety evaluations. It is worth mentioning that the gel demonstrated shear thinning properties and exhibited characteristics of an elastic solid, thereby confirming its structural stability. The gel demonstrated a notable affinity for mucosal surfaces in comparison to traditional azithromycin aqueous solutions. In vitro release testing revealed that drug release transpired via diffusion mechanisms, following a first-order kinetic release pattern. Additionally, the formulated gel exhibited remarkable antibacterial efficacy against Staphylococcus aureus and Pseudomonas aeruginosa in bacteriostatic evaluations. Lastly, safety assessments confirmed that the gel eye drops induced minimal irritation and displayed no apparent cytotoxicity, indicating their good safety and biocompatibility for ocular application. Thus, these findings indicated that the prepared azithromycin gel eye drops complied with the requisite standards for ophthalmic preparations.
Graphical Abstract








Similar content being viewed by others
References
Liu YC, Lin MT, Ng AHC, Wong TT, Mehta JS. Nanotechnology for the treatment of allergic conjunctival diseases. Pharmaceuticals (Basel). 2020;13(11). https://doi.org/10.3390/ph13110351.
Liu YC, Ng AHC, Ng XW, Yan P, Venkatraman SS, Mehta JS, et al. Evaluation of a sustained-release prednisolone acetate biodegradable subconjunctival implant in a non-human primate model. Translation Vision Sci Technol. 2017;6(5):9. https://doi.org/10.1167/tvst.6.5.9.
Wu KY, Ashkar S, Jain S, Marchand M, Tran SD. Breaking barriers in eye treatment: polymeric nano-based drug-delivery system for anterior segment diseases and glaucoma. Polymers. 2023;15(6). https://doi.org/10.3390/polym15061373.
Tang X, Liu J, Yan R, Peng Q. Carbohydrate polymer-based bioadhesive formulations and their potentials for the treatment of ocular diseases: a review. Int J Biol Macromol. 2023;242(Pt 3):124902. https://doi.org/10.1016/j.ijbiomac.2023.124902.
Mofidfar M, Abdi B, Ahadian S, Mostafavi E, Desai TA, Abbasi F, et al. Drug delivery to the anterior segment of the eye: a review of current and future treatment strategies. Int J Pharm. 2021;607:120924. https://doi.org/10.1016/j.ijpharm.2021.120924.
Han Y, Jiang L, Shi H, Xu C, Liu M, Li Q, et al. Effectiveness of an ocular adhesive polyhedral oligomeric silsesquioxane hybrid thermo-responsive FK506 hydrogel in a murine model of dry eye. Bioact Mater. 2022;9:77–91. https://doi.org/10.1016/j.bioactmat.2021.07.027.
Wen Y, Song Z, Xu H, Feng S, Zhu L, Teng F, et al. Azithromycin-loaded linolenic acid-modified methoxy poly(ethylene glycol) micelles for bacterial infection treatment. Drug Deliv Transl Res. 2022;12(3):550–61. https://doi.org/10.1007/s13346-021-00953-2.
Wei W, Li S, Xu H, Zhou F, Wen Y, Song Z, et al. MPEG-PCL copolymeric micelles for encapsulation of azithromycin. AAPS PharmSciTech. 2018;19(5):2041–7. https://doi.org/10.1208/s12249-018-1009-0.
Khalil IA, Ali IH, El-Sherbiny IM. Noninvasive biodegradable nanoparticles-in-nanofibers single-dose ocular insert: in vitro, ex vivo and in vivo evaluation. Nanomedicine (Lond). 2019;14(1):33–55. https://doi.org/10.2217/nnm-2018-0297.
Eid HM, Naguib IA, Alsantali RI, Alsalahat I, Hegazy AM. Novel Chitosan-coated niosomal formulation for improved management of bacterial conjunctivitis: a highly permeable and efficient ocular nanocarrier for azithromycin. J Pharm Sci. 2021;110(8):3027–36. https://doi.org/10.1016/j.xphs.2021.04.020.
Mahaling B, Baruah N, Ahamad N, Maisha N, Lavik E, Katti DS. A non-invasive nanoparticle-based sustained dual-drug delivery system as an eyedrop for endophthalmitis. Int J Pharm. 2021;606:120900. https://doi.org/10.1016/j.ijpharm.2021.120900.
Wu F, Zhao X, Guo S, Ni S, Dai Y, Han Y, et al. A bioequivalence study with pharmacokinetic endpoints for azithromycin eye drops. Clin Pharmacol Drug Dev. 2023;12(7):761–6. https://doi.org/10.1002/cpdd.1226.
Bella AL, Einterz E, Huguet P, Bensaid P, Amza A, Renault D. Effectiveness and safety of azithromycin 1.5% eye drops for mass treatment of active trachoma in a highly endemic district in Cameroon. BMJ Open Ophthalmol. 2020;5(1):e000531. https://doi.org/10.1136/bmjophth-2020-000531.
Wu R, Huang Q, Zhou Z, Chen Y, Hu H, Wang F, et al. Nanoparticulate ophthalmic drug delivery of norfloxacin to prevent ocular infection after cataract surgery: evaluation in animal model. Mater Exp. 2021;11(8):1402–11. https://doi.org/10.1166/mex.2021.2040.
Hegde RR, Verma A, Ghosh A. Microemulsion: new insights into the ocular drug delivery. ISRN Pharm. 2013;2013:826798. https://doi.org/10.1155/2013/826798.
Marcano DC, Shin CS, Lee B, Isenhart LC, Liu X, Li F, et al. Synergistic cysteamine delivery nanowafer as an efficacious treatment modality for corneal cystinosis. Mol Pharm. 2016;13(10):3468–77. https://doi.org/10.1021/acs.molpharmaceut.6b00488.
Mfoafo K, Omidi Y, Omidian H. Thermoresponsive mucoadhesive hybrid gels in advanced drug delivery systems. Int J Pharm. 2023;636:122799. https://doi.org/10.1016/j.ijpharm.2023.122799.
White JM, Garza A, Griebler JJ, Bates FS, Calabrese MA. Engineering the structure and rheological properties of P407 hydrogels via reverse poloxamer addition. Langmuir. 2023;39(14):5084–94. https://doi.org/10.1021/acs.langmuir.3c00088.
Lai WF, Reddy OS, Zhang D, Wu H, Wong WT. Cross-linked chitosan/lysozyme hydrogels with inherent antibacterial activity and tuneable drug release properties for cutaneous drug administration. Sci Technol Adv Mater. 2023;24(1):2167466. https://doi.org/10.1080/14686996.2023.2167466.
Kurniawansyah IS, Gozali D, Sopyan I, Iqbal M, Subarnas A. Physical study of chloramphenicol in situ gel with base hydroxypropyl methylcellulose and poloxamer 188. J Pharm Bioallied Sci. 2019;11(Suppl 4):S547-s50. https://doi.org/10.4103/jpbs.JPBS_201_19.
Pace LA, Plate JF, Mannava S, Barnwell JC, Koman LA, Li Z, et al. A human hair keratin hydrogel scaffold enhances median nerve regeneration in nonhuman primates: an electrophysiological and histological study. Tissue Eng Part A. 2014;20(3–4):507–17. https://doi.org/10.1089/ten.TEA.2013.0084.
Catoira MC, Fusaro L, Di Francesco D, Ramella M, Boccafoschi F. Overview of natural hydrogels for regenerative medicine applications. J Mater Sci Mater Med. 2019;30(10):115. https://doi.org/10.1007/s10856-019-6318-7.
Costa AF, Luís S, Noro J, Silva S, Silva C, Ribeiro A. Therapeutic textiles functionalized with keratin-based particles encapsulating terbinafine for the treatment of onychomycosis. Int J Mol Sci. 2022;23(22). https://doi.org/10.3390/ijms232213999.
Yu B, Kong D, Cheng C, Xiang D, Cao L, Liu Y, et al. Assembly and recognition of keratins: a structural perspective. Semin Cell Dev Biol. 2022;128:80–9. https://doi.org/10.1016/j.semcdb.2021.09.018.
Senthilkumar N, Chowdhury S, Sanpui P. Extraction of keratin from keratinous wastes: current status and future directions. J Mater Cycle Waste Manage. 2022;25(1):1–16. https://doi.org/10.1007/s10163-022-01492-9.
Nuutinen EM, Valle-Delgado JJ, Kellock M, Farooq M, Osterberg M. Affinity of keratin peptides for cellulose and lignin: a fundamental study toward advanced bio-based materials. Langmuir. 2022;38(32):9917–27. https://doi.org/10.1021/acs.langmuir.2c01140.
Mattiello S, Guzzini A, Del Giudice A, Santulli C, Antonini M, Lupidi G, et al. Physico-chemical characterization of keratin from wool and chicken feathers extracted using refined chemical methods. Polymers. 2022;15(1). https://doi.org/10.3390/polym15010181.
Tang A, Li Y, Yao Y, Yang X, Cao Z, Nie H, et al. Injectable keratin hydrogels as hemostatic and wound dressing materials. Biomater Sci. 2021;9(11):4169–77. https://doi.org/10.1039/d1bm00135c.
Chen M, Ren X, Dong L, Li X, Cheng H. Preparation of dynamic covalently crosslinking keratin hydrogels based on thiol/disulfide bonds exchange strategy. Int J Biol Macromol. 2021;182:1259–67. https://doi.org/10.1016/j.ijbiomac.2021.05.057.
Wang Y, Xu Y, Zhang Z, He Y, Hou Z, Zhao Z, et al. Rational design of high-performance keratin-based hemostatic agents. Adv Healthc Mater. 2022;11(15):e2200290. https://doi.org/10.1002/adhm.202200290.
Feng CC, Lu WF, Liu YC, Liu TH, Chen YC, Chien HW, et al. A hemostatic keratin/alginate hydrogel scaffold with methylene blue mediated antimicrobial photodynamic therapy. J Mater Chem B. 2022;10(25):4878–88. https://doi.org/10.1039/d2tb00898j.
Demir GC, Erdemli O, Keskin D, Tezcaner A. Xanthan-gelatin and xanthan-gelatin-keratin wound dressings for local delivery of Vitamin C. Int J Pharm. 2022;614:121436. https://doi.org/10.1016/j.ijpharm.2021.121436.
Lu W-F, Lu T-Y, Liu Y-C, Liu T-H, Feng C-C, Lin C-W, et al. Keratin-associated protein nanoparticles as hemostatic agents. ACS Appl Nano Mater. 2021;4(11):12798–806. https://doi.org/10.1021/acsanm.1c03558.
Singaravelu S, Ramanathan G, Raja MD, Nagiah N, Padmapriya P, Kaveri K, et al. Biomimetic interconnected porous keratin-fibrin-gelatin 3D sponge for tissue engineering application. Int J Biol Macromol. 2016;86:810–9. https://doi.org/10.1016/j.ijbiomac.2016.02.021.
Navarro J, Swayambunathan J, Lerman M, Santoro M, Fisher JP. Development of keratin-based membranes for potential use in skin repair. Acta Biomater. 2019;83:177–88. https://doi.org/10.1016/j.actbio.2018.10.025.
Min SJ, Lee JS, Nah H, Moon H-J, Lee SJ, Kang HJ, et al. Degradable and tunable keratin-fibrinogen hydrogel as controlled release system for skin tissue regeneration. J Bionic Eng. 2023;20(3):1049–59. https://doi.org/10.1007/s42235-022-00317-7.
Sharma S, Rostamabadi H, Gupta S, Kumar Nadda A, Kharazmi MS, Jafari SM. Nano/micro-formulations of keratin in biocomposites, wound healing and drug delivery systems; recent advances in biomedical applications. Eur Polymer J. 2022;180. https://doi.org/10.1016/j.eurpolymj.2022.111614.
Zhang H, Su F, Ma X, Zhao G. Brief introduction of keratin and its biological application, especially in drug delivery. Emergent Mater. 2021;4(5):1225–42. https://doi.org/10.1007/s42247-021-00216-3.
Du J, Wang L, Han X, Dou J, Jiang X, Yuan J. Polydopamine/keratin complexes as gatekeepers of mesoporous silica nanoparticles for pH and GSH dual responsive drug delivery. Materials Letters. 2021;293. https://doi.org/10.1016/j.matlet.2021.129676.
Srinivasan B, Kumar R, Shanmugam K, Sivagnam UT, Reddy NP, Sehgal PK. Porous keratin scaffold-promising biomaterial for tissue engineering and drug delivery. J Biomed Mater Res B Appl Biomater. 2010;92(1):5–12. https://doi.org/10.1002/jbm.b.31483.
Yang J, Yu H, Wang L, Liu J, Liu X, Hong Y, et al. Advances in adhesive hydrogels for tissue engineering. European Polymer Journal. 2022;172. https://doi.org/10.1016/j.eurpolymj.2022.111241.
Sarma A. Biological importance and pharmaceutical significance of keratin: a review. Int J Biol Macromol. 2022;219:395–413. https://doi.org/10.1016/j.ijbiomac.2022.08.002.
de Guzman RC, Saul JM, Ellenburg MD, Merrill MR, Coan HB, Smith TL, et al. Bone regeneration with BMP-2 delivered from keratose scaffolds. Biomaterials. 2013;34(6):1644–56. https://doi.org/10.1016/j.biomaterials.2012.11.002.
Yuan J, Geng J, Xing Z, Shim KJ, Han I, Kim JC, et al. Novel wound dressing based on nanofibrous PHBV-keratin mats. J Tissue Eng Regen Med. 2015;9(9):1027–35. https://doi.org/10.1002/term.1653.
Zhai M, Xu Y, Zhou B, Jing W. Keratin-chitosan/n-ZnO nanocomposite hydrogel for antimicrobial treatment of burn wound healing: characterization and biomedical application. J Photochem Photobiol B. 2018;180:253–8. https://doi.org/10.1016/j.jphotobiol.2018.02.018.
Sadeghi S, Nourmohammadi J, Ghaee A, Soleimani N. Carboxymethyl cellulose-human hair keratin hydrogel with controlled clindamycin release as antibacterial wound dressing. Int J Biol Macromol. 2020;147:1239–47. https://doi.org/10.1016/j.ijbiomac.2019.09.251.
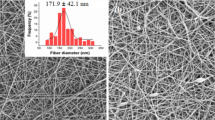
Cruz-Maya I, Guarino V, Almaguer-Flores A, Alvarez-Perez MA, Varesano A, Vineis C. Highly polydisperse keratin rich nanofibers: scaffold design and in vitro characterization. J Biomed Mater Res A. 2019;107(8):1803–13. https://doi.org/10.1002/jbm.a.36699.
Li Y, Lin J, Zhi X, Li P, Jiang X, Yuan J. Triple stimuli-responsive keratin nanoparticles as carriers for drug and potential nitric oxide release. Mater Sci Eng C Mater Biol Appl. 2018;91:606–14. https://doi.org/10.1016/j.msec.2018.05.073.
Wan X, Liu P, Jin X, Xin X, Li P, Yuan J, et al. Electrospun PCL/keratin/AuNPs mats with the catalytic generation of nitric oxide for potential of vascular tissue engineering. J Biomed Mater Res A. 2018;106(12):3239–47. https://doi.org/10.1002/jbm.a.36521.
Hosny KM, Rizg WY, Alkhalidi HM, Abualsunun WA, Bakhaidar RB, Almehmady AM, et al. Nanocubosomal based in situ gel loaded with natamycin for ocular fungal diseases: development, optimization, in-vitro, and in-vivo assessment. Drug Deliv. 2021;28(1):1836–48. https://doi.org/10.1080/10717544.2021.1965675.
Acknowledgements
The authors would like to thank NMPA Key Laboratory for Research and Evaluation of Pharmaceutical Preparations and Excipients, China Pharmaceutical University for providing the instruments and equipment related to the paper.
Funding
This work was supported by the Taizhou Science and Technology Supporting Agriculture Project (TN202006) and the Medical Science Research of Hebei Province (20230403).
Author information
Authors and Affiliations
Contributions
M.S.: formal analysis, date curation, writing-original draft. J.N.: formal analysis, methodology, investigation. Y.Z.: formal analysis, methodology, date curation, validation. M.W. and Y.S.: characterization, software. Y.M., X.C., and Q.L.: conceptualization, methodology, resources, supervision, formal analysis, writing review and editing.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, M., Niu, J., Zhang, Y. et al. Keratin Formed Bioadhesive Ophthalmic Gel for the Bacterial Conjunctivitis Treatment. AAPS PharmSciTech 25, 77 (2024). https://doi.org/10.1208/s12249-024-02772-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-024-02772-3