Abstract
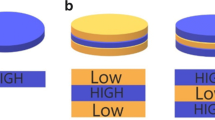
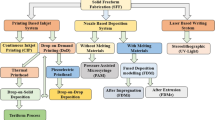
Implants are drug delivery platforms that consist of a drug-polymer matrix with the ability of providing a localized and efficient controlled release of the drug with minimal side effects and achievement of the desired therapeutic outcomes with low drug loadings. Direct powder extrusion (DPE) 3D printing technology involves the extrusion of material through a nozzle of the printer in the form of pellets or powder. The present study aimed at investigating the use of the CELLINK BIO X™ bioprinter using DPE 3D printing technique to fabricate and evaluate the impact of different shapes (cuboid, cylinder, and tube) of raloxifene hydrochloride (RFH)-loaded subdermal implants on the release of RFH from the implants. This study further evaluated the impact of different processing techniques, viz., hot-melt extrusion (HME) technology vs. DPE 3D printing technique, on the release of RFH from the implants fabricated by each processing technique. All the fabricated implants were characterized by XRD, DSC, SEM, and FTIR, and evaluated for their water uptake, mass loss, and in vitro RFH release. The current study successfully demonstrated a great opportunity of controlling and/or tuning the release of RFH from the subdermal implants by altering the implant shape, and hence surface area, and could be a great contribution and/or addition to the personalization of medicines and improvement of patient compliance.












Similar content being viewed by others
Data Availability
Data will be available up on request.
References
Stewart SA, Domínguez-Robles J, Donnelly RF, Larrañeta E. Implantable polymeric drug delivery devices: classification, manufacture, materials, and clinical applications. Polymers. 2018;10(12):1379.
Dharmayanti C, Gillam TA, Williams DB, Blencowe A. Drug-eluting biodegradable implants for the sustained release of bisphosphonates. Polymers. 2020;12(12):1–14.
Zheng Y, Pokorski JK. Hot melt extrusion: an emerging manufacturing method for slow and sustained protein delivery. Nanomed Nanobiotechnol. 2021;13(5):1–23.
Takahashi M, Onishi H, MacHida Y. Development of implant tablet for a week-long sustained release. J Control Release. 2004;100(1):63–74.
Solano AGR, et al. Development and evaluation of sustained-release etoposide-loaded poly(ε-caprolactone) implants. AAPS PharmSciTech. 2013;14(2):890–900.
Koutsamanis I, Spoerk M, Arbeiter F, Eder S, Roblegg E. Development of porous polyurethane implants manufactured via hot-melt extrusion. Polymers. 2020;12(12):1–22.
Muhindo D, Ashour EA, Almutairi M, Repka MA. Development and evaluation of raloxifene hydrochloride-loaded subdermal implants using hot-melt extrusion technology. Int J Pharm. 2022;622(5):121834.
Manoukian OS, et al. Biodegradable polymeric injectable implants for long-term delivery of contraceptive drugs. J Appl Polym Sci. 2018;135(14):1–23.
Cheng L, Lei L, Guo S. In vitro and in vivo evaluation of praziquantel loaded implants based on PEG/PCL blends. Int J Pharm. 2010;387(1–2):129–38.
Khaled SA, Burley JC, Alexander MR, Yang J, Roberts CJ. 3D printing of tablets containing multiple drugs with defined release profiles. Int J Pharm. 2015;494(2):643–50.
Abaci A, Gedeon C, Kuna A, Guvendiren M. Additive manufacturing of oral tablets: Technologies, materials and printed tablets. Pharmaceutics. 2021;13(2):1–27.
Al-Dulimi Z, Wallis M, Tan DK, Maniruzzaman M, Nokhodchi A. 3D printing technology as innovative solutions for biomedical applications. Drug Discov Today. 2021;26(2):360–83.
Vithani K, Goyanes A, Jannin V, Basit AW, Gaisford S, Boyd BJ. An overview of 3D printing technologies for soft materials and potential opportunities for lipid-based drug delivery systems. Pharm Res. 2019;36(1):4.
Wang J, et al. Emerging 3D printing technologies for drug delivery devices: Current status and future perspective. Adv Drug Deliv Rev. 2021;174:294–316.
Tan DK, Maniruzzaman M, Nokhodchi A. Development and optimisation of novel polymeric compositions for sustained release theophylline. Polymers. 2020;12(1):1–18.
Norman J, Madurawe RD, Moore CMV, Khan MA, Khairuzzaman A. A new chapter in pharmaceutical manufacturing: 3D-printed drug products. Adv Drug Deliv Rev. 2017;108:39–50.
Khaled SA, Burley JC, Alexander MR, Yang J, Roberts CJ. 3D printing of five-in-one dose combination polypill with defined immediate and sustained release profiles. J Control Release. 2015;217:308–14.
Edinger M, Jacobsen J, Bar-Shalom D, Rantanen J, Genina N. Analytical aspects of printed oral dosage forms. Int J Pharm. 2018;553(1–2):97–108.
Wallis M, Al-Dulimi Z, Tan DK, Maniruzzaman M, Nokhodchi A. 3D printing for enhanced drug delivery: current state-of-the-art and challenges. Drug Dev Ind Pharm. 2020;46(9):1385–401.
Chen G, Xu Y, Kwok PCL, Kang L. Pharmaceutical applications of 3D printing. Addit Manuf. 2020;34(4):101209.
Tool R, et al. Novel on-demand 3-dimensional (3D) printed tablets using fill density as an effective release-controlling tool. Polymers. 2020;12(1872):1–21.
Rahim TNAT, Abdullah AM, Md Akil H. Recent developments in fused deposition modeling-based 3D printing of polymers and their composites. Polym Rev. 2019;59(4):589–624.
Cui M, et al. Exploration and preparation of patient-specific ciprofloxacin implants drug delivery system via 3D printing technologies. J Pharm Sci. 2021;110(11):3678–89.
Bandari S, Nyavanandi D, Dumpa N, Repka MA. Coupling hot melt extrusion and fused deposition modeling: critical properties for successful performance. Adv Drug Deliv Rev. 2021;172:52–63.
Long J, Gholizadeh H, Lu J, Bunt C, Seyfoddin A. Application of fused deposition modelling (FDM) method of 3D printing in drug delivery. Curr Pharm Des. 2017;23(3):433–9.
Keikhosravi N, Mirdamadian SZ, Varshosaz J, Taheri A. Preparation and characterization of polypills containing aspirin and simvastatin using 3D printing technology for the prevention of cardiovascular diseases. Drug Dev Ind Pharm. 2020;46(10):1665–75.
Oladeji SA, Dadou SM, Zhao M, Li S, Jones DS, Andrews GP. The development and optimisation of gastro-retentive floating tablets using fused deposition modelling 3D printing. J Pharm Pharmacol. 2022;176(3):1–17.
Manini G, Benali S, Mathew A, Napolitano S, Raquez JM, Goole J. Paliperidone palmitate as model of heat-sensitive drug for long-acting 3D printing application. Int J Pharm. 2022;618(3):121662.
Gültekin HE, Tort S, Tuğcu-Demiröz F, Acartürk F. 3D printed extended release tablets for once daily use: an in vitro and in vivo evaluation study for a personalized solid dosage form. Int J Pharm. 2021;596(1):120222.
Lamichhane S, Park J, Sohn DH, Lee S. Customized novel design of 3D printed pregabalin tablets for intra-gastric floating and controlled release using FDM. Pharmaceutics. 2019;11(11):564.
Shi K, Slavage JP, Maniruzzaman M, Nokhodchi A. Role of release modifiers to modulate drug release from fused deposition modelling (FDM) 3D printed tablets. Int J Pharm. 2021;597(3):120315.
Vaz VM, Kumar L. 3D printing as a promising tool in personalized medicine. AAPS PharmSciTech. 2021;22:1–20.
Farmer ZL, et al. 3D printed estradiol-eluting urogynecological mesh implants: Influence of material and mesh geometry on their mechanical properties. Int J Pharm. 2021;593(11):120145.
Zhao X, Wei W, Niu R, Li Q, Hu C, Jiang S. 3D printed intragastric floating and sustained-release tablets with air chambers. J Pharm Sci. 2022;111(1):116–23.
Mirdamadian SZ, Varshosaz J, Minaiyan M, Taheri A. 3D printed tablets containing oxaliplatin loaded alginate nanoparticles for colon cancer targeted delivery. An in vitro/in vivo study. Int J Biol Macromol. 2022;205(2):90–109.
Krause J, Müller L, Sarwinska D, Seidlitz A, Sznitowska M, Weitschies W. 3D printing of mini tablets for pediatric use. Pharmaceuticals. 2021;14(2):1–16.
Yang Y, et al. 3D-printed polycaprolactone-chitosan based drug delivery implants for personalized administration. Mater Des. 2022;214(2):110394.
Li R, Pan Y, Chen D, Xu X, Yan G, Fan T. Design, preparation and in vitro evaluation of core–shell fused deposition modelling 3D-printed verapamil hydrochloride pulsatile tablets. Pharmaceutics. 2022;14(2):437.
Fanous M, et al. Development of immediate release 3D-printed dosage forms for a poorly water-soluble drug by fused deposition modeling: Study of morphology, solid state and dissolution. Int J Pharm. 2021;599:120417.
Cailleaux S, Sanchez-Ballester NM, Gueche YA, Bataille B, Soulairol I. Fused deposition modeling (FDM), the new asset for the production of tailored medicines. J Control Release. 2021;330(7):821–41.
Okwuosa TC, Soares C, Gollwitzer V, Habashy R, Timmins P, Alhnan MA. On demand manufacturing of patient-specific liquid capsules via co-ordinated 3D printing and liquid dispensing. Eur J Pharm Sci. 2018;118(3):134–43.
Isreb A, Baj K, Wojsz M, Isreb M, Peak M, Alhnan MA. 3D printed oral theophylline doses with innovative ‘radiator-like’ design: impact of polyethylene oxide (PEO) molecular weight. Int J Pharm. 2019;564(4):98–105.
Verstraete G, et al. 3D printing of high drug loaded dosage forms using thermoplastic polyurethanes. Int J Pharm. 2018;536(1):318–25.
Gorkem Buyukgoz G, Soffer D, Defendre J, Pizzano GM, Davé RN. Exploring tablet design options for tailoring drug release and dose via fused deposition modeling (FDM) 3D printing. Int J Pharm. 2020;591(7):119987.
Đuranović M, Obeid S, Madžarević M, Cvijić S, Ibrić S. Paracetamol extended release FDM 3D printlets: evaluation of formulation variables on printability and drug release. Int J Pharm. 2021;592(7):120053.
Ong JJ, et al. 3D printed opioid medicines with alcohol-resistant and abuse-deterrent properties. Int J Pharm. 2020;579(1):119169.
Pistone M, et al. Direct cyclodextrin-based powder extrusion 3D printing for one-step production of the BCS class II model drug niclosamide. Drug Deliv Transl Res. 2022;12(8):1895–910.
Goyanes A, Allahham N, Trenfield SJ, Stoyanov E, Gaisford S, Basit AW. Direct powder extrusion 3D printing: fabrication of drug products using a novel single-step process. Int J Pharm. 2019;567(6):118471.
Boniatti J, et al. Direct powder extrusion 3d printing of praziquantel to overcome neglected disease formulation challenges in paediatric populations. Pharmaceutics. 2021;13(8):1114.
Mendibil X, Tena G, Duque A, Uranga N, Campanero MÁ, Alonso J. Direct powder extrusion of paracetamol loaded mixtures for 3d printed pharmaceutics for personalized medicine via low temperature thermal processing. Pharmaceutics. 2021;13(6):907.
Fanous M, Gold S, Muller S, Hirsch S, Ogorka J, Imanidis G. Simplification of fused deposition modeling 3D-printing paradigm: Feasibility of 1-step direct powder printing for immediate release dosage form production. Int J Pharm. 2020;578(2):119124.
Kuźmińska M, et al. Solvent-free temperature-facilitated direct extrusion 3D printing for pharmaceuticals. Int J Pharm. 2021;598(10):1–9.
Annaji M, et al. Application of extrusion-based 3D printed dosage forms in the treatment of chronic diseases. J Pharm Sci. 2020;109(12):3551–68.
Sánchez-Guirales SA, Jurado N, Kara A, Lalatsa A, Serrano DR. Understanding direct powder extrusion for fabrication of 3d printed personalised medicines: a case study for nifedipine minitablets. Pharmaceutics. 2021;13(10):1583.
Stewart SA, et al. Development of a biodegradable subcutaneous implant for prolonged drug delivery using 3D printing. Pharmaceutics. 2020;12(2):105.
Tappa K, et al. Medication eluting devices for the field of OBGYN (MEDOBGYN): 3D printed biodegradable hormone eluting constructs, a proof of concept study. PLoS ONE. 2017;12(8):1–17.
Kempin W, et al. Assessment of different polymers and drug loads for fused deposition modeling of drug loaded implants. Eur J Pharm Biopharm. 2017;115(6):84–93.
Wang Y, et al. 3D printed biodegradable implants as an individualized drug delivery system for local chemotherapy of osteosarcoma. Mater Des. 2020;186(1):108336.
Liaskoni A, Wildman RD, Roberts CJ. 3D printed polymeric drug-eluting implants. Int J Pharm. 2021;597(12):120330.
Vo AQ, Zhang J, Nyavanandi D, Bandari S, Repka MA. Hot-melt extrusion paired fused deposition modeling 3D printing to develop hydroxypropyl cellulose based floating tablets of cinnarizine. Carbohyd Polym. 2020;246(15):139–48.
Narala S, Nyavanandi D, Alzahrani A, Bandari S, Zhang F, Repka MA. Creation of hydrochlorothiazide pharmaceutical cocrystals via hot-melt extrusion for enhanced solubility and permeability. AAPS PharmSciTech. 2022;23(1):1–11.
Li D, et al. PLA/F68/Dexamethasone implants prepared by hot-melt extrusion for controlled release of anti-inflammatory drug to implantable medical devices: I. Preparation, characterization and hydrolytic degradation study. Int J Pharm. 2013;441(1–2):365–72.
Balik BA, Argin S, Lagaron JM, Torres-Giner S. Preparation and characterization of electrospun pectin-based films and their application in sustainable aroma barrier multilayer packaging. Appl Sci. 2019;9(23):5136.
Quinten T, De Beer T, Vervaet C, Remon JP. Evaluation of injection moulding as a pharmaceutical technology to produce matrix tablets. Eur J Pharm Biopharm. 2009;71(1):145–54.
Andrews GP, Jones DS, Diak OA, McCoy CP, Watts AB, McGinity JW. The manufacture and characterisation of hot-melt extruded enteric tablets. Eur J Pharm Biopharm. 2008;69(1):264–73.
Banker GS, Rhodes CT. Modern pharmaceutics. Boca Raton: Taylor & Francis Group; 2019. p. 105–12.
Baishya H. Application of mathematical models in drug release kinetics of carbidopa and levodopa ER tablets. J Dev Drugs. 2017;06(02):1–8.
Acknowledgements
This project was also partially supported by Grant Number P30GM122733-01A1, funded by the National Institute of General Medical Sciences (NIGMS) a component of the National Institutes of Health (NIH) as one of its Centers of Biomedical Research Excellence (COBRE).
Author information
Authors and Affiliations
Contributions
Derick Muhindo: Study conception and design, conduct laboratory experiments, analyze experimental data collected, interpretation of results, manuscript writing/preparation.
Eman A. Ashour: Review and approve the study conception and design, review set up of laboratory experiments, review data and results generated from laboratory experiments, review the drafted manuscript and provide feedback to have the final manuscript ready for submission to the journal.
Mashan Almutairi: Assist in designing and conducting laboratory experiments.
Michael A. Repka: Review and approve the study conception and design, review set up of laboratory experiments, review data and results generated from laboratory experiments, review and approve the final manuscript for submission to the journal.
Corresponding author
Ethics declarations
Conflict of Interest
The authors believe that there are no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muhindo, D., Ashour, E.A., Almutairi, M. et al. Development of Subdermal Implants Using Direct Powder Extrusion 3D Printing and Hot-Melt Extrusion Technologies. AAPS PharmSciTech 24, 215 (2023). https://doi.org/10.1208/s12249-023-02669-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-023-02669-7