Abstract
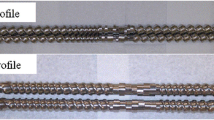
The current study aimed to see the effects of poloxamer P407 on the dissolution performance of hydroxypropyl methylcellulose acetate succinate (AquaSolve™ HPMC-AS HG)-based amorphous solid dispersions (ASD). A weakly acidic, poorly water-soluble active pharmaceutical ingredient (API), mefenamic acid (MA), was selected as a model drug. Thermal investigations, including thermogravimetry (TG) and differential scanning calorimetry (DSC), were conducted for raw materials and physical mixtures as a part of the pre-formulation studies and later to characterize the extruded filaments. The API was blended with the polymers using a twin shell V-blender for 10 min and then extruded using an 11-mm twin-screw co-rotating extruder. Scanning electron microscopy (SEM) was used to study the morphology of the extruded filaments. Furthermore, Fourier-transform infrared spectroscopy (FT-IR) was performed to check the intermolecular interactions of the components. Finally, to assess the in vitro drug release of the ASDs, dissolution testing was conducted in phosphate buffer (0.1 M, pH 7.4) and hydrochloric acid–potassium chloride (HCl-KCl) buffer (0.1 M, pH 1.2). The DSC studies confirmed the formation of the ASDs, and the drug content of the extruded filaments was observed to be within an acceptable range. Furthermore, the study concluded that the formulations containing poloxamer P407 exhibited a significant increase in dissolution performance compared to the filaments with only HPMC-AS HG (at pH 7.4). In addition, the optimized formulation, F3, was stable for over 3 months when exposed to accelerated stability studies.
Graphical Abstract









Similar content being viewed by others
References
Crowley MM, et al. Pharmaceutical applications of hot-melt extrusion: part I. Drug Dev Ind Pharm. 2007;33:909–26.
Jermain SV, et al. In vitro and in vivo behaviors of KinetiSol and spray-dried amorphous solid dispersions of a weakly basic drug and ionic polymer†. Mol Pharm. 2020;17:2789–808.
Thakkar R, Thakkar R, Pillai A, Ashour EA, Repka MA. Systematic screening of pharmaceutical polymers for hot melt extrusion processing: a comprehensive review. Int J Pharm. 2020;576: 118989.
Sherje AP, Jadhav M. β-Cyclodextrin-based inclusion complexes and nanocomposites of rivaroxaban for solubility enhancement. J Mater Sci Mater Med. 2018;29:186.
Mandati P, et al. Hot-melt extrusion–based fused deposition modeling 3D printing of atorvastatin calcium tablets: impact of shape and infill density on printability and performance. AAPS PharmSciTech. 2022;24:13.
Sahakijpijarn S, et al. Using thin film freezing to minimize excipients in inhalable tacrolimus dry powder formulations. Int J Pharm. 2020;586: 119490.
Manish M, Harshal J, Anant P. Melt sonocrystallization of ibuprofen: effect on crystal properties. Eur J Pharm Sci Off J Eur Fed Pharm Sci. 2005;25:41–8.
Bajaj A, Rao MRP, Pardeshi A, Sali D. Nanocrystallization by evaporative antisolvent technique for solubility and bioavailability enhancement of telmisartan. AAPS PharmSciTech. 2012;13:1331–40.
Kittikunakorn N, Sun CC, Zhang F. Effect of screw profile and processing conditions on physical transformation and chemical degradation of gabapentin during twin-screw melt granulation. Eur J Pharm Sci Off J Eur Fed Pharm Sci. 2019;131:243–53.
Repka MA, et al. Pharmaceutical applications of hot-melt extrusion: Part II. Drug Dev Ind Pharm. 2007;33:1043–57.
Maniruzzaman M, et al. Drug-polymer intermolecular interactions in hot-melt extruded solid dispersions. Int J Pharm. 2013;443:199–208.
Ajjarapu S, et al. A rapid tool to optimize process variables for continuous manufacturing of metronidazole ointment using melt extrusion technique. AAPS PharmSciTech. 2020;21:273.
Shettar A, et al. Development and characterization of novel topical oil/PEG creams of voriconazole for the treatment of fungal infections. J Drug Deliv Sci Technol. 2021;66: 102928.
Hussain Shaik, Md Z, Shiva J, Venkateswarlu G, Suthakaran D, Ghouse S. Formulation and evaluation of ritonavir immediate release tablets by hot melt extrusion method. J Drug Deliv Ther. 2019;9:63–71.
Ma X, et al. Influence of carbamazepine dihydrate on the preparation of amorphous solid dispersions by hot melt extrusion. Pharm. 2020;12:379.
Sarabu S, et al. Preliminary investigation of peroxide levels of Plasdone™ copovidones on the purity of atorvastatin calcium amorphous solid dispersions: impact of plasticizers on hot melt extrusion processability. J Drug Deliv Sci Technol. 2022;70: 103190.
Almotairy A, et al. Investigation of hot melt extrusion process parameters on solubility and tabletability of atorvastatin calcium in presence of Neusilin® US2. J Drug Deliv Sci Technol. 2023;79: 104075.
Lin X, et al. Physical stability of amorphous solid dispersions: a physicochemical perspective with thermodynamic, kinetic and environmental aspects. Pharm Res. 2018;35:125.
Feng S, Bandari S, Repka MA. Investigation of poly(2-ethyl-2-oxazoline) as a novel extended release polymer for hot-melt extrusion paired with fused deposition modeling 3D printing. J Drug Deliv Sci Technol. 2022;74: 103558.
Zhang Z, Feng S, Almotairy A, Bandari S, Repka MA. Development of multifunctional drug delivery system via hot-melt extrusion paired with fused deposition modeling 3D printing techniques. Eur J Pharm Biopharm. 2023;183:102–11.
Hurley D, Potter CB, Walker GM, Higginbotham CL. Investigation of ethylene oxide-co-propylene oxide for dissolution enhancement of hot-melt extruded solid dispersions. J Pharm Sci. 2018;107:1372–82.
LaFountaine JS, et al. Thermal processing of PVP- and HPMC-based amorphous solid dispersions. AAPS PharmSciTech. 2016;17:120–32.
Thakkar R, et al. Novel on-demand 3-dimensional (3-D) printed tablets using fill density as an effective release-controlling tool. Polym. 2020;12:1872.
Maniruzzaman M, et al. Taste masking of paracetamol by hot-melt extrusion: an in vitro and in vivo evaluation. Eur J Pharm Biopharm Off J Arbeitsgemeinschaft Pharm Verfahrenstechnik EV. 2012;80:433–42.
Hunter LJ, Wood DM, Dargan PI. The patterns of toxicity and management of acute nonsteroidal anti-inflammatory drug (NSAID) overdose. Open Access Emerg Med OAEM. 2011;3:39–48.
Passerini N, Albertini B, González-Rodríguez ML, Cavallari C, Rodriguez L. Preparation and characterisation of ibuprofen-poloxamer 188 granules obtained by melt granulation. Eur J Pharm Sci Off J Eur Fed Pharm Sci. 2002;15:71–8.
Seo A, Holm P, Kristensen HG, Schaefer T. The preparation of agglomerates containing solid dispersions of diazepam by melt agglomeration in a high shear mixer. Int J Pharm. 2003;259:161–71.
Serajuddin AT. Solid dispersion of poorly water-soluble drugs: early promises, subsequent problems, and recent breakthroughs. J Pharm Sci. 1999;88:1058–66.
Vilhelmsen T, Eliasen H, Schaefer T. Effect of a melt agglomeration process on agglomerates containing solid dispersions. Int J Pharm. 2005;303:132–42.
Alshahrani SM, et al. Stability-enhanced hot-melt extruded amorphous solid dispersions via combinations of Soluplus® and HPMCAS-HF. AAPS PharmSciTech. 2015;16:824–34.
Thakkar R, et al. A comparison between lab-scale and hot-melt-extruder-based anti-inflammatory ointment manufacturing. AAPS PharmSciTech. 2020;21:200.
Yu LX, et al. Understanding pharmaceutical quality by design. AAPS J. 2014;16:771–83.
Alzahrani A, et al. Design and optimization of ciprofloxacin hydrochloride biodegradable 3D printed ocular inserts: full factorial design and in-vitro and ex-vivo evaluations: Part II. Int J Pharm. 2023;631: 122533.
Weissman SA, Anderson NG. Design of experiments (DoE) and process optimization. A review of recent publications. Org Process Res Dev. 2015;19:1605–33.
Chavez P-F, et al. Optimization of a pharmaceutical tablet formulation based on a design space approach and using vibrational spectroscopy as PAT tool. Int J Pharm. 2015;486:13–20.
Goos P, Jones B, Syafitri U. I-Optimal design of mixture experiments. J Am Stat Assoc. 2016;111:899–911.
Politis N, S., Colombo, P., Colombo, G. & M Rekkas, D. Design of experiments (DoE) in pharmaceutical development. Drug Dev Ind Pharm. 2017;43:889–901.
Morott JT, et al. The effects of screw configuration and polymeric carriers on hot-melt extruded taste-masked formulations incorporated into orally disintegrating tablets. J Pharm Sci. 2015;104:124–34.
Dedroog S, Pas T, Vergauwen B, Huygens C, Van den Mooter G. Solid-state analysis of amorphous solid dispersions: why DSC and XRPD may not be regarded as stand-alone techniques. J Pharm Biomed Anal. 2020;178: 112937.
Bhide S, Panda A, Rangappa S, Shettar A, Repka MA, Prado R, Kundu S, Richardson N, Murthy SN. Evaluating the impact of fatty alcohols on permeation of clotrimazole from topical creams. Pharm Technol. 2020;44:24–31.
Karavas E, Georgarakis M, Docoslis A, Bikiaris D. Combining SEM, TEM, and micro-Raman techniques to differentiate between the amorphous molecular level dispersions and nanodispersions of a poorly water-soluble drug within a polymer matrix. Int J Pharm. 2007;340:76–83.
Kolimi P, et al. Development and validation of HPLC method for efinaconazole: application to human nail permeation studies. AAPS PharmSciTech. 2022;23:63.
Research, C. for D. E. and. Q1A(R2) stability testing of new drug substances and products. U.S. Food and Drug Administration https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q1ar2-stability-testing-new-drug-substances-and-products (2020). Accessed 03/05/2018.
Noce L, Gwaza L, Mangas-Sanjuan V, Garcia-Arieta A. Comparison of free software platforms for the calculation of the 90% confidence interval of f2 similarity factor by bootstrap analysis. Eur J Pharm Sci Off J Eur Fed Pharm Sci. 2020;146: 105259.
Yuksel N, Kanik AE, Baykara T. Comparison of in vitro dissolution profiles by ANOVA-based, model-dependent and -independent methods. Int J Pharm. 2000;209:57–67.
Shankar VK, et al. Effect of lipid vehicles on solubility, stability, and topical permeation of delta-9-tetrahydrocannabinol. AAPS PharmSciTech. 2022;23:223.
Zhou W, Gilpin RK. Rapid ESI-MS method for examining the thermal decomposition of pharmaceuticals. J Pharm Sci. 2004;93:1545–56.
Abdul Mudalip SK, et al. Effects of solvents on polymorphism and shape of mefenamic acid crystals. MATEC Web Conf. 2018;150:02004.
Panchagnula R, Sundaramurthy P, Pillai O, Agrawal S, Raj YA. Solid-state characterization of mefenamic acid. J Pharm Sci. 2004;93:1019–29.
Real D, Orzan L, Leonardi D, Salomon CJ. Improving the dissolution of triclabendazole from stable crystalline solid dispersions formulated for oral delivery. AAPS PharmSciTech. 2019;21:16.
Ewing AV, Clarke GS, Kazarian SG. Stability of indomethacin with relevance to the release from amorphous solid dispersions studied with ATR-FTIR spectroscopic imaging. Eur J Pharm Sci Off J Eur Fed Pharm Sci. 2014;60:64–71.
Thenmozhi K, Yoo YJ. Enhanced solubility of piperine using hydrophilic carrier-based potent solid dispersion systems. Drug Dev Ind Pharm. 2017;43:1501–9.
Kuroiwa Y, Higashi K, Ueda K, Yamamoto K, Moribe K. Nano-scale and molecular-level understanding of wet-milled indomethacin/poloxamer 407 nanosuspension with TEM, suspended-state NMR, and Raman measurements. Int J Pharm. 2018;537:30–9.
Hillery AM, Florence AT. The effect of adsorbed poloxamer 188 and 407 surfactants on the intestinal uptake of 60-nm polystyrene particles after oral administration in the rat. Int J Pharm. 1996;132:123–30.
Wolfe JA, et al. Gastritis, duodenitis, and bleeding duodenal ulcer following mefenamic acid therapy. Arch Intern Med. 1976;136:923–5.
Gudis K, Sakamoto C. The role of cyclooxygenase in gastric mucosal protection. Dig Dis Sci. 2005;50(Suppl 1):S16-23.
Anderberg EK, Bisrat M, Nyström C. Physicochemical aspects of drug release. VII. The effect of surfactant concentration and drug particle size on solubility and dissolution rate of felodipine, a sparingly soluble drug. Int J Pharm. 1988;47:67–77.
Mehanna MM, Motawaa AM, Samaha MW. In sight into tadalafil - block copolymer binary solid dispersion: Mechanistic investigation of dissolution enhancement. Int J Pharm. 2010;402:78–88.
Acknowledgements
The authors thank the BASF Corporation, Gattefosse, and Ashland Pharmaceuticals for providing the polymers. The scanning electron microscopy images presented in this work were generated using the instruments and services at the Microscopy and Imaging Center, The University of Mississippi.
Funding
The Microscopy and Imaging Center facility is partly supported by grant 1726880 from the National. Science Foundation.
Author information
Authors and Affiliations
Contributions
Conceptualization: Ashay Shukla, Suresh Bandari, and Michael A Repka; methodology: Ashay Shukla, Nagi Reddy Dumpa; formal analysis and investigation: Ashay Shukla, Eman Ashour, and Suresh Bandari; writing—original draft preparation: Ashay Shukla; writing—review and editing: Ashay Shukla, Rishi Thakkar, and Abhishek Shettar; supervision and advise: Michael A Repka.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shukla, A., Dumpa, N.R., Thakkar, R. et al. Influence of Poloxamer on the Dissolution and Stability of Hot-Melt Extrusion–Based Amorphous Solid Dispersions Using Design of Experiments. AAPS PharmSciTech 24, 107 (2023). https://doi.org/10.1208/s12249-023-02562-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-023-02562-3