Abstract
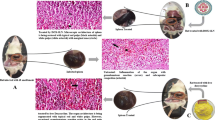
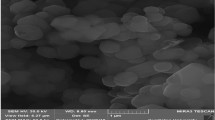
Brucellosis is a common zoonotic infection, particularly in the developing world. The recommended treatment regimens for brucellosis involve the use of two medications such as doxycycline and curcumin in order to avoid relapses and prolonged use of these drugs. Doxycycline has excellent activity in the acidic phagolysosomal environment, while curcumin modulates the immune system function and macrophage activity. Due to the intracellular existence of Brucellae and the different anti-immune mechanisms of Brucella, the treatment of Brucella infection faces many limitations. The design of nanosystems is a promising treatment approach for brucellosis. The objective of this study was to design and evaluate the efficacy of in situ pH-responsive curcumin-loaded niosome hydrogel and doxycycline-loaded chitosan–sodium alginate nanoparticles as chemotherapeutic agents against brucellosis. The prepared formulae showed a spherical nano shape with a slow drug release pattern and small particle size. The prepared formulae were evaluated in vivo using Guinea pigs experimentally infected with Brucella melitensis biovar3. The prepared formula combination gave a significant high reduction rate of Brucella spleen viable count compared with that of untreated controls at p < 0.05. The results showed that the treatment schemes were not fully successful in eliminating Brucella infection in Guinea pigs; however, they significantly (p < 0.05) reduced the viable Brucella count in a shorter time and sub-therapeutic doses. Collectively the novel prepared formulae could be a successful therapy for the effective treatment of brucellosis infection at the recommended therapeutic doses.

Graphical abstract








Similar content being viewed by others
Change history
17 December 2020
A Correction to this paper has been published: https://doi.org/10.1208/s12249-020-01899-3
Abbreviations
- DOX:
-
Doxycycline
- LD50 :
-
Median lethal dose
- GMO:
-
Glyceryl monooleate
- b.wt:
-
Body weight
- h:
-
Hour
- IPB:
-
Isotonic phosphate buffer
- EE:
-
Entrapment efficiency
- PDI:
-
Polydispersity index
- TEM:
-
Transmission electron microscopy
- BPAT:
-
Buffered plate antigen test
- RBT:
-
Rose Bengal test
- BAPA:
-
Buffered acidified plate antigen
- CFU:
-
Colony-forming unit
References
Morales-Estrada AI, Lopez-Merino A, Gutierrez-Mendez N, Ruiz EA, Contreras-Rodriguez A. Partial characterization of bacteriocin produced by halotolerant Pediococcus acidilactici strain QC38 isolated from traditional Cotija cheese. Pol J Microbiol. 2016;65(3):279–85.
Atluri VL, Xavier MN, de Jong MF, den Hartigh AB, Tsolis RM. Interactions of the human pathogenic Brucella species with their hosts. Annu Rev Microbiol. 2011;65:523–41.
Corbel MJ. Brucellosis: an overview. Emerg Infect Dis. 1997;3(2):213–21.
Olsen S, Palmer M. Advancement of knowledge of Brucella over the past 50 years. Vet Pathol. 2014;51(6):1076–89.
Corbel, M.J., Brucellosis in humans and animals. 2006: World Health Organization.
Ranjbar M. Treatment of brucellosis. Teheran: Updates on Brucellosis. InTech; 2015. p. 171–84.
Solera J. Update on brucellosis: therapeutic challenges. Int J Antimicrob Agents. 2010;36:S18–20.
Rabbani-Anari M, et al. Antibiotics for treating human brucellosis. Cochrane Database Syst Rev. 2008;2.
Hussain Z, Thu HE, Amjad MW, Hussain F, Ahmed TA, Khan S. Exploring recent developments to improve antioxidant, anti-inflammatory and antimicrobial efficacy of curcumin: a review of new trends and future perspectives. Mater Sci Eng C. 2017;77:1316–26.
Shao-Ling W, et al. Curcumin, a potential inhibitor of up-regulation of TNF-alpha and IL-6 induced by palmitate in 3T3-L1 adipocytes through NF-kappaB and JNK pathway. Biomed Environ Sci. 2009;22(1):32–9.
Zhao Y, Chen B, Shen J, Wan L, Zhu Y, Yi T, et al. The beneficial effects of quercetin, curcumin, and resveratrol in obesity. Oxidative Med Cell Longev. 2017;2017:1–8.
Jagetia GC, Aggarwal BB. “Spicing up” of the immune system by curcumin. J Clin Immunol. 2007;27(1):19–35.
Hoover DL, Borschel RH. Medical protection against brucellosis, in Biological Weapons Defense. Berlin: Springer; 2005. p. 155–84.
Abhinav K, et al. Review on niosomes as novel drug delivery system. Int Res J Pharma. 2011;2(5):61–5.
Shaker DS, Shaker MA, Hanafy MS. Cellular uptake, cytotoxicity and in-vivo evaluation of Tamoxifen citrate loaded niosomes. Int J Pharm. 2015;493(1–2):285–94.
Ganguly S, Dash AK. A novel in situ gel for sustained drug delivery and targeting. Int J Pharm. 2004;276(1–2):83–92.
He P, Davis SS, Illum L. In vitro evaluation of the mucoadhesive properties of chitosan microspheres. Int J Pharm. 1998;166(1):75–88.
Chifiriuc, M.C., et al., Antibiotic drug delivery systems for the intracellular targeting of bacterial pathogens, in Smart Drug Delivery System. 2016, IntechOpen.
Salouti, M. and A. Ahangari, Nanoparticle based drug delivery systems for treatment of infectious diseases. Vol. 552. 2014: InTech.
Armstead AL, Li B. Nanomedicine as an emerging approach against intracellular pathogens. Int J Nanomedicine. 2011;6:3281.
Imbuluzqueta, E., et al., Drug delivery systems for potential treatment of intracellular bacterial infections. 2010
Salem HF, Kharshoum RM, Abo el-Ela FI, F AG, Abdellatif KRA. Evaluation and optimization of pH-responsive niosomes as a carrier for efficient treatment of breast cancer. Drug Deliv Transl Res. 2018;8(3):633–44.
Salem HF, Kharshoum RM, Gamal F. A, Abo el-Ela FI, Abdellatif KRA. Treatment of breast cancer with engineered novel pH-sensitive triaryl-(Z)-olefin niosomes containing hydrogel: an in vitro and in vivo study. J Liposome Res. 2020;30(2):126–35.
Handjani-Vila R, et al. Dispersions of lamellar phases of non-ionic lipids in cosmetic products. Int J Cosmet Sci. 1979;1(5):303–14.
Kassem MA, Megahed MA, Abu Elyazid SK, Abd-Allah FI, Abdelghany TM, al-Abd AM, et al. Enhancing the therapeutic efficacy of tamoxifen citrate loaded span-based nano-vesicles on human breast adenocarcinoma cells. AAPS PharmSciTech. 2018;19(4):1529–43.
Motwani SK, Chopra S, Talegaonkar S, Kohli K, Ahmad FJ, Khar RK. Chitosan–sodium alginate nanoparticles as submicroscopic reservoirs for ocular delivery: formulation, optimisation and in vitro characterisation. Eur J Pharm Biopharm. 2008;68(3):513–25.
Wahlgren M, Axenstrand M, Håkansson Å, Marefati A, Lomstein Pedersen B. In vitro methods to study colon release: state of the art and an outlook on new strategies for better in-vitro biorelevant release media. Pharmaceutics. 2019;11(2):95.
Guinedi AS, Mortada ND, Mansour S, Hathout RM. Preparation and evaluation of reverse-phase evaporation and multilamellar niosomes as ophthalmic carriers of acetazolamide. Int J Pharm. 2005;306(1–2):71–82.
Sayed OM, et al. Treatment of basal cell carcinoma via binary Ethosomes of Vismodegib: in vitro and in vivo studies. AAPS PharmSciTech. 2020;21(2):51.
Gamal A, et al. Proniosomal microcarriers: impact of constituents on the physicochemical properties of proniosomes as a new approach to enhance inhalation efficiency of dry powder inhalers. AAPS PharmSciTech. 2020;21:1–12.
Gamal FA, et al. Control of basal cell carcinoma via positively charged ethosomes of Vismodegib: in vitro and in vivo studies. J Drug Delivery Sci Technol. 2020;56:101556.
Hao Y, Zhao F, Li N, Yang Y, Li K’. Studies on a high encapsulation of colchicine by a niosome system. Int J Pharm. 2002;244(1):73–80.
Nasr M, Mansour S, Mortada ND, Elshamy AA. Vesicular aceclofenac systems: a comparative study between liposomes and niosomes. J Microencapsul. 2008;25(7):499–512.
Franklin RK, Marcus SA, Talaat AM, KuKanich BK, Sullivan R, Krugner-Higby LA, et al. A novel loading method for doxycycline liposomes for intracellular drug delivery: characterization of in vitro and in vivo release kinetics and efficacy in a J774A. 1 cell line model of Mycobacterium smegmatis infection. Drug Metab Dispos. 2015;43(8):1236–45.
Lorke D. A new approach to practical acute toxicity testing. Arch Toxicol. 1983;54(4):275–87.
Alton, G.G., et al., Techniques for the brucellosis laboratory. 1988: Institut National de la recherche Agronomique (INRA).
OIE, Infection with Brucella abortus, Brucella melitensis and Brucella suis. 2016, OIE (World Organisation for Animal Health) Rome.
Bomann, W., NTN33893-study for acute oral toxicity to mice. Unpublished report from Bayer AG, report, 1989(18593).
Barquero-Calvo E, et al. Bacterial counts in spleen. Bio-protocol. 2013;3:1–6.
García-Yoldi D, et al. Multiplex PCR assay for the identification and differentiation of all Brucella species and the vaccine strains Brucella abortus S19 and RB51 and Brucella melitensis Rev1. Clin Chem. 2006;52(4):779–81.
Bancroft JD, Gamble M. Theory and practice of histological techniques. Amsterdam: Elsevier health sciences; 2008.
da Silva ALL, et al. Preliminary results for genetic transformation of shoot tip of Eucalyptus saligna Sm. via Agrobacterium tumefaciens. J Biotechnol Biodivers. 2011;2(1):1–6.
Nicoletti P, Winter AJ. The immune response to B. abortus: the cell-mediated response to infections. Animal brucellosis. Boca Raton, Fla: CRC Press, Inc.; 1990. p. 83.
Senelar R, et al. Thymic and splenic changes following injection of living Brucella and BCG in the Guinea pig. Cancer Immunol Immunother. 1977;3(1):15–22.
Ying W, Nguyen MQ, Jahre JA. Brucella canis endocarditis: case report. Clin Infect Dis. 1999;29(6):1593–4.
Hensel ME, et al. Characterization of an intratracheal aerosol challenge model of Brucella melitensis in guinea pigs. PLoS One. 2019:14(3).
Grilló M-J, Blasco J, Gorvel J, Moriyón I, Moreno E. What have we learned from brucellosis in the mouse model? Vet Res. 2012;43(1):29.
Morones JR, Elechiguerra JL, Camacho A, Holt K, Kouri JB, Ramírez JT, et al. The bactericidal effect of silver nanoparticles. Nanotechnology. 2005;16(10):2346–53.
Ranjan A, et al. Antibacterial efficacy of core-shell nanostructures encapsulating gentamicin against an in vivo intracellular Salmonella model. Int J Nanomedicine. 2009;4:289.
Misra R, Acharya S, Sahoo SK. Cancer nanotechnology: application of nanotechnology in cancer therapy. Drug Discov Today. 2010;15(19–20):842–50.
Marei A, Boghdadi G, Abdel-Hamed N, Hessin R, Abdoel T, Smits H, et al. Laboratory diagnosis of human brucellosis in Egypt and persistence of the pathogen following treatment. J Infect Dev Ctries. 2011;5(11):786–91.
Heo E-J, Kang SI, Kim JW, Her M, Cho D, Cho YS, et al. In vitro activities of antimicrobials against Brucella abortus isolates from cattle in Korea during 1998-2006. J Microbiol Biotechnol. 2012;22(4):567–70.
Abed N, Couvreur P. Nanocarriers for antibiotics: a promising solution to treat intracellular bacterial infections. Int J Antimicrob Agents. 2014;43(6):485–96.
Weir E, Lawlor A, Whelan A, Regan F. The use of nanoparticles in anti-microbial materials and their characterization. Analyst. 2008;133(7):835–45.
Milward F, Nicoletti P, Hoffmann E. Effectiveness of various therapeutic regimens for bovine brucellosis. Am J Vet Res. 1984;45(9):1825–8.
Nicoletti P, Lenk RP, Popescu MC, Swenson CE. Efficacy of various treatment regimens, using liposomal streptomycin in cows with brucellosis. Am J Vet Res. 1989;50(7):1004–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abo El-Ela, F.I., Hussein, K.H., El-Banna, H.A. et al. Treatment of Brucellosis in Guinea Pigs via a Combination of Engineered Novel pH-Responsive Curcumin Niosome Hydrogel and Doxycycline-Loaded Chitosan–Sodium Alginate Nanoparticles: an In Vitro and In Vivo Study. AAPS PharmSciTech 21, 326 (2020). https://doi.org/10.1208/s12249-020-01833-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-020-01833-7