Abstract
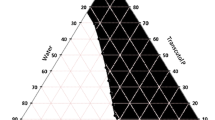
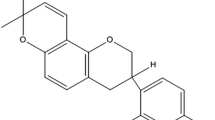
The aim the study was to design, formulate, and evaluate self-nanoemulsifying drug delivery systems (SNEDDS) of itraconazole for improving the topical antifungal properties of the drug by adopting the nanoemulsion intermediate gel of the optimized system. Solubility study was conducted to select the most appropriate oils and surfactants for formulation. Different possible systems were created. Ternary phase diagrams were constructed to select the most promising system for further study. The nanoemulsion intermediate gel of the selected system was evaluated for stability, dilution effect, viscosity, pH, antifungal activity, droplet size, PDI, and zeta potential. In vitro release of the drug from the selected intermediate gel was investigated, and the kinetic model of drug release was determined. Ex vivo permeation of itraconazole was studied, and the amount of drug accumulated in the skin was calculated. Solubility and phase diagrams revealed that the system consisting of 60% cotton seed oil and 40% span 80 provided the nanoemulsion intermediate gel with the highest drug concentration. The selected system had a droplet size of about 236 nm and zeta potential of − 59.8. The viscosity of the corresponding intermediate gel was 1583.47 cp. The system exhibited high stability at 4°C and 25°C for 12 months and improved antifungal activity. In vitro release study showed complete release of itraconazole within 4 h, while the ex vivo permeation study revealed accumulation of the majority of the drug within the skin layers (72.5%).







Similar content being viewed by others
References
Six K, Berghmans H, Leuner C, Dressman J, Van Werde K, Mullens J, et al. Characterization of solid dispersions of itraconazole and hydroxypropylmethylcellulos prepared by melt extrusion, part II. Pharm Res. 2003;20:1047–54.
Ji-Yeon Hong JKK. Yun-Kyoung song, Jeong-Sook Park, Chong-kook Kim. A new self-emulsifying formulation of itraconazole with improved dissolution and oral aabsorption. J Control Release. 2006;110(2):332–8.
Taupitz T, Dressman JB, Buchanan CM, Klein S. Cyclodextrin-water soluble polymer ternary complexes enhance the solubility and dissolution behaviour of poorly soluble drugs. Case example: itraconazole. Eur. J Pharm Biopharm. 2013;83:378–87.
Sriamornsak P, Burapapadh K. Characterization of recrystallized itraconazole prepared by cooling and anti-solvent crystallization. Asian J Pharm Sci. 2015;10(3):230–8.
Sosa L, Clares B, Alvarado HL, Bozal N, Domenech O, Calpena AC. Amphotericin B releasing topical nanoemulsion for the treatment of candidiasis and aspergillosis. Nanomedicine. 2017;13(7):2303–12.
Yamaguchi K, Mitsui T, Aso Y, Sugibayashi K. Structure-permeability relationship analysis of the permeation barrier properties of the stratum corneum and viable epidermis/dermis of rat skin. J Pharm Sci. 2008;97(10):4391–403.
Perez AP, Altube MJ, Schilrreff P, Apezteguia G, Celes FS, Zacchino S, et al. Topical amphotericin B in ultradeformable liposomes: formulation, skin penetration study, antifungal and antileishmanial activity in vitro. Colloids Surf B Biointerfaces. 2016;139:190–8.
Sanchez DA, Schairer D, Tuckman-Vernon C, Chouake J, Kunter a, Makdisi J. et al. Amphotericin B releasing nanoparticle topical treatment of Candida spp. in the setting of a burn wound. Nanomedicine. 2014; 10(1): 269–277.
Salerno C, Chiappetta DA, Arechavala A, Gorzalczany S, Scioscia SL, Bregni C. Lipid-based microtubes for topical delivery of amphotericin B. Colloids Surf B Biointerfaces. 2013;107:160–6.
Kaur L, Jain SK, Manhas RK, Sharma D. Nanoethosomal formulation for skin targeting of amphotericin B: an in vitro and in vivo assessment. J Liposome Res. 2015;25(4):294–307.
Fernández-Campos F, Clares Naveros B, López Serrano O, Alonso Merino C, Calpena Campmany AC. Evaluation of novel nystatin nanoemulsion for skin candidosis infections. Mycoses. 2013;56(1):70–81.
Yi T, Wan J, Xu H, Yang X. A new solid self-microemulsifying formulation prepared by spray-drying to improve the oral bioavailability of poorly water soluble drugs. Eur J Pharm Biopharm. 2008;70(2):439–44.
El-Badry M, Fetih G, Shakeel F. Comparative topical delivery of antifungal drug croconazole using liposome and micro-emulsion-based gel formulations. Drug Deliv. 2014;21(1):34–43.
Asija R, Yadav P, Asija S. Self emulsifying drug delivery system: a promising approach for bioavailability enhancement. IJRDPL. 2014;3:872–6.
Shabnam A, Qurratul A, Shama P. An overview on various approaches used for solubilization of poorly soluble drugs. T Pharm Res. 2009;2:84–104.
Hosny KM, Aldawsari HM, Bahmdan RH, et al. Preparation, optimization, and evaluation of hyaluronic acid-based hydrogel loaded with miconazole self-nanoemulsion for the treatment of oral thrush. AAPS PharmSciTech. 2019;20(7):297.
Date AA, Nagarsenker MS. Design and evaluation of self-nanoemulsifying drug delivery systems (SNEDDS) for cefpodoxime proxetil. Int J Pharm. 2007;329(1–2):166–72.
Srilatha R, Aparna CS, Srinivas P, Sadanandam M. Formulation, evaluation and characterization of glipizide nanoemulsion. AJPCR. 2013;6:66–71.
Asija R, Dhaker PC, Nama N. Formulation & evaluation of voriconazole ointment for topical delivery. JDDTBP. 2015;3:7–14.
Aparna C, Srinivas P, Rao Patnaik KSK. Formulation and evaluation of solid self emulsifying drug delivery system of voriconazole. J Pharm Pharm Sci. 2015;4(2):17.
Danielli LJ, Dos Reis M, Bianchini M, Camargo GS, Bordignon SAL, Guerreiro IK, et al. Antidermatophytic activity of volatile oil and nanoemulsion of Stenachaenium megapotamicum (Spreng.) baker. Ind. Crops Prod. 2013;50:23–8.
Gupta R, Mukherjee B. Development and in vitro evaluation of diltiazem hydrochloride transdermal patches based on povidone–ethylcellulose matrices. Drug Dev Ind Pharm. 2003;29(1):1–7.
Scott RC, Corrigan MA, Smith F, Mason H. The influence of skin structure on permeability: an intersite and interspecies comparison with hydrophilic penetrants. J Investig Dermatol. 1991;96(6):921–5.
Mukherjee B, Mahapatra S, Gupta R, Patra B, Tiwari A, Arora P. A comparison between povidone-ethylcellulose and povidone-eudragit transdermal dexamethasone matrix patches based on in vitro skin permeation. Eur J Pharm Biopharm. 2005;59(3):475–83.
Durrheim H, Flvnn GL, Himchi WI, Behl CR. Permeation of hairless mouse skin I: experimental methods and comparison with human epidermal permeation by alkanols. J Pharm Sci. 1980;69(7):781–6.
Xi J, Chang Q, Chan CK, Meng ZY, Wang GN, Sun JB. Formulation development and bioavailability evaluation of a self-nanoemulsified drug delivery system of oleanolic acid. AAPS PharmSciTech. 2009;10(1):172–82.
Jaiswal P, Aggarwal G, Harikumar S, Kaur A. Bioavailability enhancement of poorly soluble drugs by SMEDDS: a review. JDDT. 2013;3(1):98–109.
Balakumar K, Raghavan CV. Selvan NT, prasad RH, Abdu S. Self nanoemulsifying drug delivery system (SNEDDS) of rosuvastatin calcium: design, formulation, bioavailability and pharmacokinetic evaluation. Colloids Surf B Biointerfaces. 2013;112:337–43.
Pįętka-Ottlik M, Lewińska A, Jaromin A, Krasowska A, Wilk KA. Antifungal organoselenium compound loaded nanoemulsions stabilized by bifunctional cationic surfactants. Colloids Surf A Physicochem Eng Asp. 2016;510:53–62.
Müller RH, Jacobs C, Kayser O. Nanosuspensions as particulate drug formulations in therapy. Rationale for development and what we can expect for the future. Adv Drug Deliv Rev. 2001;47(1):3–19.
Peltola S, Saarinen-Savolainen P, Kiesvaara J, Suhonen TM, Urtti A. Microemulsions for topical delivery of estradiol. Int J Pharm. 2003;254(2):99–107.
Gasco MR, Gallarate M, Pattarino F. In vitro permeation of azelaic acid from viscosized microemulsions. Int J Pharm. 1991;69:193–6.
El Maghraby GM. Transdermal delivery of hydrocortisone from eucalyptus oil microemulsion: effects of cosurfactants. Int J Pharm. 2008;355(1–2):285–92.
Hirano E, Morimoto K, Takeeda T, Nakamoto Y, Morisaka K. Pharmaceutical studies of polyacrylic acid aqueous gel bases. II. Absorption of ibuprofen from gel preparations following rectal administration in rats. Chem Pharm Bull (Tokyo). 1980;28(12):3521–6.
El-Badry M, Fetih G. Preparation, charactarization and anti-inflammatory activity of celecoxib chitosan gel formulations. JDDST. 2011;21(2):201–6.
Yildirim S, Oztop MH, Soyer Y. Cinnamon oil nanoemulsions by spontaneous emulsification: formulation, characterization and antimicrobial activity. LWT Food Sci Technol. 2017;84:122–8.
Makoid MC, Dufoure A, Banakar UV. Modelling of dissolution behaviour of controlled release systems. STP Pharma. 1993;Prat. 3:49–58.
Gupta M, Goyal AK, Paliwal SR, Paliwal R, Mishra N, Vaidya B, et al. Development and characterization of effective topical liposomal system for localized treatment of cutaneous candidiasis. J Liposome Res. 2010;20(4):341–50.
Acknowledgments
The authors would like to thank the staff member assistants of pharmaceutics department, Faculty of Pharmacy, Minia University, for their help in the ex vivo study.
Author information
Authors and Affiliations
Contributions
Amal K. Hussein and Heba F. Mansour planned and supervised the project. Sara R. Botros formulated the systems and performed experimental work. Heba F. Mansour and Sara R. Botros contributed to writing the manuscript. All the authors contributed to editing the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Applied for Egyptian patent
Electronic Supplementary Material
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Botros, S.R., Hussein, A.K. & Mansour, H.F. A Novel Nanoemulsion Intermediate Gel as a Promising Approach for Delivery of Itraconazole: Design, In Vitro and Ex Vivo Appraisal. AAPS PharmSciTech 21, 272 (2020). https://doi.org/10.1208/s12249-020-01830-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-020-01830-w