Abstract
The interpretation of immunogenicity results for a mAb product and prediction of its clinical consequences remain difficult, despite enormous advances in methodologies and efforts toward the best practice for consistent data generation and reporting. To this end, the contribution from the clinical pharmacology discipline has been largely limited to comparing descriptively the pharmacokinetic (PK) profiles by antidrug antibodies (ADA) status or testing the significance of ADA as a covariate in a population PK setting, similar to the practice for small-molecule drugs in investigating the effect of an intrinsic/extrinsic factor on the drug disposition. There is a need for a mAb disposition framework that captures the dynamics of ADA formation and drug’s interactions with the ADA and target as parts of the drug distribution and elimination. Here we describe such a framework and examine it against the PK, ADA, and clinical response data from a phase 3 trial in patients treated with adalimumab. The proposed framework offered a generalized understanding of how the dose, target affinity, and drug/ADA analyte forms affects the manifestation of ADA response with regard to its detections and alterations of drug disposition and effectiveness. Furthermore, as an example, its utility for dose considerations was demonstrated through predicting for late-stage trials of a PCSK9 inhibitor in terms of development in ADA incidence and titers, and consequences on the drug disposition, interaction with target, and downstream lowering effect on LDL-C.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Therapeutic monoclonal antibodies (mAbs) have achieved unprecedented success in treating various diseases, including cancers, immune disorders, and infectious diseases, in recent years (1, 2). The mAbs share distinctive advantages of having high specificity towards their targets. Despite their clinical success, mAbs have the potential to be highly immunogenic and elicit high affinity anti-drug antibodies (ADA) that can neutralize the drug or accelerate clearance, leading to a lack of efficacy, or increase the risk of adverse reactions (3,4,5)
Numerous factors, some product related, such as non-human sequence, process related impurities, and other patient related, such as genetic predisposition and disease type/concomitant medication, and their interplay have been suggested to influence the immunogenicity of a mAb product (6, 7). The ADA response was initially thought to be related to the murine origin of the mAbs. In the effort of reducing the non-human portions, the antibody constructs have evolved over years via developing chimeric, humanized, and fully human mAbs. Unfortunately, this effort did not result in abolishing the immunogenicity potential of mAbs (8). The consequences of immunogenicity response range from no evidence of clinical effect to the severe adverse immune reactions and/or loss of drug effectiveness (4, 5, 7, 9).
Immunogenicity testing and appropriate interpretations of the results are, therefore, the critical aspects of the safety and efficacy profiles of a mAb product. The immunogenicity testing involves detection, confirmation, and characterization of ADA in terms of its incidence and binding and/or neutralizing capacity (10). Despite impressive advances in methodologies, as well as harmonization in data generation and reporting (9), the interpretation of immunogenicity results and prediction of its clinical consequences remain difficult (7, 11). To this end, the contribution from the clinical pharmacology discipline has been largely limited to comparing descriptively the PK profiles by ADA status or testing the significance of ADA as a covariate in a population PK setting (12). These analyses have been widely used for small-molecule drugs in investigating the effect of an intrinsic/extrinsic factor on the drug disposition, under the assumption that the concentration of or exposure to drug (usually in the unbound form) is a good surrogate for predicting the clinical outcomes. However, these analyses are often not predictive of the clinical consequences of an ADA response for a given mAb at a specific dose (13), as they offer little or no insight into the key aspects of drug disposition of a mAb, i.e., the drug-ADA interplay and its influence on the drug-target interaction.
In this communication, we describe a framework for characterizing the mAb disposition, including the ADA formation and elimination, following dose administration, based on the drug and ADA analytes from commonly used assays, with a focus on its utility in predicting the ADA impact on the drug disposition and effectiveness. For this purpose, unlike those originally developed for small-molecule drugs, the mAb disposition framework revolves around drug’s interplay with the ADA and interaction with the intended target, and the net effect on the drug bound target (or occupied receptor) or unbound target, as the surrogate endpoint, depending on the specific mAb under consideration. We carried out 3 case studies: (1) to examine the validity of the framework against the PK, ADA, and clinical response data collected from a phase 3 trial in patients with rheumatoid arthritis (RA) treated with adalimumab (Humira®); (2) to provide a generalized understanding of how the dose, along with other factors, such as the affinity to and abundance of target, and total drug/ADA vs. their unbound forms, affects the manifestation of ADA response in terms of its detections and alterations of the drug disposition and effectiveness; and (3) to show the utility of the framework for dose optimization considerations through trial simulations.
Materials and Methods
The mAb Disposition Framework
The Core Structure
Figure 1 represents the core structure of the proposed mAb disposition framework based on commonly used analytes for mAb concentrations, ADA titers, and target concentrations. The corresponding differential equations in terms of the total amount of each analyte may be written as follows:
where \({In}_{D}, {In}_{T}, {\text{and}}\; {In}_{A}\) are the rates (nmol/day) of drug delivery, target production, and ADA input, respectively; \(\gamma\) is the fraction of the full ADA input into the blood sampling compartment at time t (see “The ADA Input Function” section); X with subscripts tD and D, tT and T, and tA and A are the amounts (nmol) of total and unbound drug, target and ADA, respectively; Those with subscripts DT and DA are the amounts of drug-target and drug-ADA complexes, respectively; similarly, V and CL are the volume (L) and clearance (L/day) terms for the species specified by the subscripts. The core structure captures two possible mechanisms by which ADA response can influence treatment effectiveness (14), i.e., formation of the drug-ADA complex leading to accelerated clearance, and the formation of neutralizing antibodies preventing the mAb from binding to its target. The full mathematical representations, including the relationships among analytes in various forms under the assumption that the drug is in respective equilibriums with the ADA and target (15,16,17), are provided in Table S1.
The schematic diagram represents the core structure of the proposed framework for describing the disposition of a mAb, including the ADA formation and elimination, following dose administration, in terms of commonly used drug and ADA analytes. It embraces the dynamic movement between the drug bindings to target and ADA, and increased clearance via the complex mediated pathways, as parts of the drug distribution and elimination processes (“The mAb Disposition Framework” section). KD1 and KD2 are the dissociation constants governing the drug bindings to target and ADA, respectively (Table S1). [ADA*] represents a collection of anti-drug antibodies in VA, XA/VA (or CA) and may be expressed in nM of a reference monoclonal ADA on a titer equivalent basis (Table S2)
The ADA Input Function
In Eq. (3), the ADA input (\(\gamma {In}_{A}\)) is a function of time. Here \(\gamma\) is approached by a transit compartments structure (15, 18), with modifications to reflect the ADA development pattern exhibiting a delayed onset followed by the escalation in intensity over subsequent repeated dose administration that eventually plateaus toward a maximum (see Fig. 2a), and to allow the ADA input to wane after the response intensification phase of a variable duration comes to an end. The expression can be written as follows:
where \({k}_{tr}\) is the transit rate constant, n is the number of postulated transit steps with the nth step occurring in the blood sampling compartment, and \({T}_{w}\) is the time to the end of the response intensification phase during which \({T}_{w}=t\) and \(\gamma\) increases at time-varying rates, and after which \(\gamma\) decreases from the maximum at a rate according to the rate constant \({k}_{w}\) (Figure S1).
The interplay between ADA response and drug disposition. a The boxplots of total ADA titers (CtA) over 182 days in two groups of adalimumab treated patients, one positive only for ADAt (ADAt + /ADAf- or ADAt +) and the other also positive for ADAf (ADAt + /ADAf + or ADAf + ). b Paired titers of ADAt (CtA) and ADAf (CA), with the unbound drug concentrations. The insert shows that among the ADAf + individuals the drug concentrations in their ADAf + samples were considerably lower (mostly BQL) than those in their ADAf- samples. c The visual predictive check plots for adalimumab PK profiles consisting of trough concentrations (except for the one on day 7) in the ADAt + (blue symbols) and ADAf + (gray symbols) groups as well as in the ADA- (orange symbols) group, where the filled and open circles represent the medians and 25th/75th percentiles for the observed concentrations, respectively, and the solid lines represent the medians of the simulated concentrations and the areas shaded or bordered by dashed lines indicate the corresponding 25th/75th percentiles. d The simulated (lines) unbound drug concentrations (CD), and total (CtA) and unbound (CA) ADA titers for an individual from the ADAf + group in comparison with the respective observations (symbols in matching color), which shows that the representation by the framework captures the moment-to-moment ADA development and its impact on the drug concentrations
Case Study 1
In case study 1, the validity of the proposed framework in terms of a full representation of mAb disposition, including drug’s interplay with the ADA, was examined using the PK, ADA, and clinical response data from RA patients treated with Humira, which were part of a long-term comparative safety and efficacy study of PF-06410293, a proposed adalimumab biosimilar, (ClinicalTrials.gov ID: NCT02480153). The study design and primary results have been described elsewhere (19). This case study was focused on the following aspects: (1) the time courses of ADA titer development, (2) the specific forms of PK and ADA analytes and their utilities for predicting the ADA consequences, and (3) the model representation for the interplay between the ADA formation and drug disposition during repeated dose administration.
Blood samples for assessing the total (ADAt) and unbound (ADAf) antidrug antibodies, as well as the unbound adalimumab, were collected periodically prior to and during a 26-week treatment period and analyzed using validated bioanalytical procedures (see Tables S3 and S4 for details). For this case study, only the data collected from patients receiving Humira in treatment period 1 were used. The model representation was evaluated using a nonlinear mixed-effect model approach (see Table S5 for details).
Case Study 2
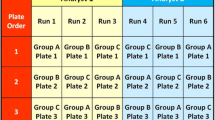
For predicting the efficacy consequences of ADA response, it is essential to recognize there are common patterns associated with dose and specific drug/ADA analyte forms. As illustrated in this case study, these patterns are readily generalizable in the proposed framework. To simplify the illustration of the dose-dependent patterns, the following 2 assumptions were made. The mAb doses are determined by the treatment needs to achieve certain levels of drug-bound (or drug-unbound) target, i.e., the greater abundance the intended target has, the higher the mAb doses are needed for the treatment. The ADA response may develop with the intensity increasing over time and eventually plateauing at its maximum, and the maximum is not, in any meaningful way, dose dependent in the dose range used in this case study. As described in Tables I, 3 simulations were performed using a hypothetical mAb, with the first two aimed at exploring the dose-dependent patterns and the third at predicting the efficacy consequences utilizing a clinical response model structure (20, 21). Furthermore, the potential influences of the target-binding affinity in predicting the consequences of ADA response were accounted for, with all 3 simulations carried out twice, each with a low or high affinity assigned to the mAb.
Case Study 3
Case study 3 was carried out to explore the utility of the proposed framework for dose optimization considerations. For this purpose, a hypothetical proprotein convertase subtilisin–kexin type 9 (PCSK9) inhibitor was created and the PK/ADA and LDL cholesterol (LDL-C) profiles were simulated based on the literature data (16, 22, 23), including the choices of unbound ADA, total drug, and total target analytes. The case study background was that the immunogenicity data emerging from a phase 2b study, where patients were treated with the PCSK9 inhibitor for 6 months via SC administration once every 2 weeks (q2w) at 100 mg, showed the ADA response occurred at a greater rate and with higher titers, relative to the phase 2a study where the same treatment was given for 3 months, and the ADA response was negligible. In this context, trial simulations (Table II) were performed to aid the dose optimization considerations.
Results
A total of 288 patients were included in case study 1, 138 patients (269 samples) were tested positive by the ADAt assay, of which 36 were also positive by the ADAf assay during the 26-week adalimumab treatment. The time courses of ADAt titers for patients positive only for ADAt (ADAt + /ADAf- or “ADAt + ”) and those also positive for ADAf (ADAt + /ADAf + or “ADAf + ”) were largely parallel, in a sigmoidal form (Fig. 2a). The onsets for the ADAt detections were delayed, by approximately 2 weeks and 6 weeks for the ADAt + /ADAf + and ADAt + /ADAf- patients, respectively, with large inter-subject variability, and the later segments toward the respective plateaus were considerably less variable. The ADAt detections occurred with samples containing adalimumab at various concentrations, whereas the ADAf detection happened when the drug concentrations were low, mostly below the quantification limit (BQL) (Fig. 2b). The observed and model-predicted drug concentration–time profiles for the ADAt + and ADAf + patients, as well as those negative for ADAt (or “ADA-”), are shown in Fig. 2c, and those with the concurrent ADA profiles for an ADAf + individual in Fig. 2d.
In case study 2, the time courses of unbound drug concentration, percent average drug-bound target over 15 doses given q2w were generated, in the presence and absence of a given ADA response, for each of the selected doses ranging from 20 to 2000 mg. As an example, those at 20 mg are shown in Fig. 3a. The impact of ADA response, as measured by the extent of the alteration in either drug disposition or drug-target interaction, diminished as the dose escalated, while each measure having a separate relationship with dose (Fig. 3b and c). In addition, the dose is shown to be a major factor affecting the unbound ADA detection compared to others such as the affinity to and abundance of target (Fig. 3d). To extend beyond the impact assessments in terms of alterations in drug disposition and drug-target interaction in the 20 mg example shown in Fig. 3a, an estimate of the efficacy consequences based on a ACR20 responder model is provided in Fig. 3e.
General patterns for predicting the ADA impact on drug disposition and effectiveness. a The time courses of unbound drug concentration (solid lines), percent average drug-bound target over the dose interval (dashed lines) with and without ADA response, namely ADA + (blue) and ADA- (orange) scenarios, over 15 doses of 20 mg, with the ADA response displayed in titer (cross). The impact of ADA response on the drug disposition and drug-target interaction was measured, respectively, using the following 2 methods: (1) the percent additional dose required in the ADA + scenario to bring the unbound drug exposure to the level in the ADA- scenario or required for the ΔAUC (shaded area in orange) to be zero, labelled as “%DoseAddl (ΔAUC = 0)”, and (2) the ratio of average drug-bound target in the ADA + scenario to that in ADA- scenario, labelled as “ADA + to ADA- ratio of drug-bound target.” b, c The impact of ADA response decreased as dose increased in terms of %DoseAddl (ΔAUC = 0) (solid lines) and ADA + to ADA- ratio of drug-bound target (dashed lines), with a high (filled symbols) and low (open symbols) affinity to the target, respectively. The low (green), medium (blue) and high (red) target production rates were used, corresponding to 3 dose segments (see Table S6). Panel a provides the details of the data points at 20 mg in b with the assumption of high affinity. d The availability of unbound ADA for the given ADA response to be detected at the end of the last dose interval decreased with dose increasing, whether the drug had the high (filled symbols) or low (open symbols) affinity to the target. e A prediction of the relative loss of clinical response for the ADA + (blue line) vs. ADA- (orange line) scenarios in a by applying the respective estimates of percent average drug-bound target to a % ACR20 responder model with the reference placebo effect (open square) and full effect of anti-TNF inhibition (open circle) (see Table S7), where the dashed line is the predicted placebo effect
Case study 3 simulated a clinical trial in 2000 patients receiving an anti-PCSK9 mAb q2w over 364 days, mimicking the reference study (23), in terms of the concentration–time profiles of total drug (Fig. 4a), total PCSK9 (Fig. 4b), and LDL-C (Fig. 4c) at various levels of ADA response. These profiles were divided into 4 ADA response groups, with 5% patients in the top ADA response group suffering from the most severe loss of the LDL-C lowering effect, and 50% in the bottom group experiencing no loss of the drug effectiveness. In addition, case study 3 simulated an alternative scenario (Fig. 4d) in which an increased dose (by approximately 70%) was administered, starting on day 126, for the top 5% patients to achieve comparable LDL-C lowering effects to those in the bottom ADA response group at the base dose. The median unbound ADA level for the top 5% patients was 1171 ng/mL on day 126, considerably higher than that (130.8 ng/mL) for the second highest ADA response group.
Median concentration–time profiles of total drug, total PCSK9 and LDL-C in 4 groups of subjects in terms of their total ADA levels (Table S8). a The ADA response had no or minimal effect on the drug trough concentrations for the lower half of the study population, group I (N = 1000), whose median maximum unbound ADA levels, \({C}_{A,max}\), was negligible at 25.0 ng/mL, and the effect became more and more appreciable as the ADA response increased through the upper half consisting of group II (N = 600) with a median \({C}_{A,max}\) of 127.7 ng/mL, group III (N = 300) with a median \({C}_{A,max}\) of 489.4 ng/mL, and group IV (N = 100) with a median \({C}_{A,max}\) of 3093 ng/mL. b, c Total PCSK9 and LDL-C levels, respectively, over time in the 4 groups of patients. d With an increased dose (by approximately 70%) starting on day 126, those in group IV (or 5% in the top ADA response group) would have the subsequent LDL-C levels (CLDL) dropped, achieving comparable LDL-C lowering effects to those in group I at the base dose. In addition, with the increased dose, the availability of unbound ADA for the given ADA response to be detected in group IV decreased drastically as evident from the fall of the median maximum unbound ADA levels (\({C}_{A,max}\))
Discussion
The interpretation of immunogenicity results for a mAb product and prediction of the clinical consequences remain challenging. This research work took on the challenge through addressing the underlying need for a disposition framework specific for mAbs that captures the dynamics of ADA formation and drug’s interactions with ADA and target, as parts of the mAb distribution and elimination processes. Such a framework can relate the ADA response to the alterations in drug disposition and effectiveness, as well as connect other factors, such as dose and drug/ADA analyte forms, to the overall picture regarding ADA manifestation and consequences that otherwise may be incomplete and skewed. As such, the applications may cover the data analyses for characterizing/defining the PK/immunogenicity profile for the given mAb and study population, and making subsequent predictions, as appropriate, with changes in factors captured in the framework (Fig. 1). Therefore, this approach is distinguishable, in one way, from those aimed at predicting the immunogenicity response a priori based on presumptive patient- and product-related factors (e.g., Kierzek et al. (24)), and, in another way, from those using a conventional PK compartment model with the ADA status added as a static covariate (12) in terms of model representation and predictive capabilities, as discussed below.
Case Study 1
The time course of ADA development is one of the important aspects in predicting the ADA consequences (also see the “Case Study 3” section). Sigmoidal patterns of ADA titer development were evident in the two groups of patients treated with Humira over 26 weeks (Fig. 2a). The observations added support for the use of Eq. (4) to characterize the time-varying ADA response. The ADA development for the group tested also positive by the ADAf assay had an earlier onset and higher titers, reflecting different roles of the unbound vs. total ADA forms, as elaborated below, as well as different assay sensitivities (Table S4).
Another important aspect is that assessing the ADA response and its impact requires one to take into account not only the analyte contents but also the analyte forms and their relationships with the counterparts (Fig. 1) in the system. Results from an assay, in isolation, may only shed light on part of the picture about the ADA response. By design, the ADAf assay targets only the ADA in unbound form, in contrast to the ADAt assay. As delineated in the framework (Fig. 1), the unbound ADA is the portion of ADA in excess of what takes part of the drug-ADA complex, and the lower the drug concentration is, the more unbound ADA is available for detection by the ADAf assay, consistent with the observations in this case study. As shown in Fig. 2b, while the ADAt detection occurred independent of the adalimumab concentrations, the ADAf detection happened only with samples from those whose drug concentrations were low or who had accelerated drug clearance. Here the potential difference in specificity between the 2 procedures should not play a meaningful role, as essentially all anti-adalimumab antibodies are directed against the TNF binding region of adalimumab (25). Furthermore, among the 36 ADAf + patients, there were 28 samples negative for ADAf, while positive for ADAt, and these samples contained adalimumab at considerably higher concentrations than the remaining 61 samples positive for ADAf (the insert of Fig. 2b). On the other hand, while more effective in determining if the ADA was present, the ADAt detection, in itself, contained no information regarding whether the drug disposition was impacted. Clearly, each assay can give only part of the picture about the ADA response. As shown in Fig. 2c and d, the framework allowed one to integrate results from the 2 different ADA assays with those from the unbound drug assay, establishing a whole picture about the ADA response and its impact on drug disposition (also see the “Case Study 2” section).
Case Study 2
In this case study, the impact of a given ADA response was quantified, in terms of the extent of the alterations in drug disposition and interaction with the target (Fig. 3a), and its general relationships with dose were examined, among other factors such as the specifics of drug-target interaction and drug/ADA analytes (Fig. 3b and c), utilizing the proposed mAb disposition framework. There were a few interesting highlights. Firstly, as a measure of the PK alteration by the given ADA response, the additional dose required in the ADA + scenario to bring the unbound drug exposure to the level in the ADA- scenario, DoseAddl(ΔAUC = 0), was shown to be the same (approximately 20 mg) across the dose range studied, reflecting the same drug loss to the binding to ADA and increased clearance. Therefore, the DoseAddl(ΔAUC = 0) provides a unique measure of the magnitude of ADA response, in terms of its resultant PK alteration, independent of any particular ADA assay, as well as dose. Consequently, the ADA impact, as measured by %DoseAddl(ΔAUC = 0) (relative to the corresponding base dose), diminished with dose increasing. This held true whether the drug had a high or low affinity to the target (Fig. 3b and c). The dose-dependent PK alterations presumably due to the ADA response were reported back to early days of the clinical investigation of infliximab in RA patients, when the PK profiles over 26 weeks were studied at doses of 1, 3, 10 mg/kg (26). The simulation results (Fig. 3b and c) offered a generalized understanding of how the dose affects the manifestation of ADA response in terms of the PK alteration. In addition, it would explain at least in part the experiences of ours and others with PK studies of various mAbs in healthy subjects, such as the extensive ADA detections and PK alterations with adalimumab at 40 mg (15, 27) versus much less or none with infliximab at 5 or 10 mg/kg (28, 29), or trastuzumab at 6 mg/kg (30, 31), recognizing the comparison is across different mAbs, with only adalimumab being a fully human mAb.
Secondly, coinciding with the ADA impact diminishing, the availability of unbound ADA for the given ADA response to be detected also fell as the dose increased (Fig. 3d). The ADA impact was essentially negligible, measured either by %DoseAddl(ΔAUC = 0) or the ADA + /ADA- ratio of drug-bound target, at doses above 200 mg (Fig. 3b and c). Consequently, the detection of unbound ADA at levels below 100 ng/mL (Fig. 3d) would not be indictive of a meaningful alteration in drug disposition or drug-bound target.
Lastly, the extent of alteration in unbound drug exposure may not be as a good predictor for the efficacy consequences as one might expect. At 20 mg, as an example, the exposure reduced in the ADA + scenario to 5.8% (Fig. 3a) and 14.2%, respectively, for drug binding to the target being of high and low affinity, relative to that in the ADA- scenario. However, the secondary effect through the substantially reduced exposure on the percent drug-bound target was quite different, with ADA + /ADA- ratios of 84.2% and 23.5% under the high and low affinity assumptions, respectively. As illustrated in Fig. 3e, the substantially reduced unbound drug exposure may translate to only a minimal loss of efficacy with a high affinity drug. This is consistent with the ACR20 results at week 26 between the ADAt + (84.3%, p = 0.703) and ADA- (86.2%) patients receiving Humira referenced in case study 1 (Fig. 2c), though here the affinity could not be estimated. Therefore, the alteration in unbound drug exposure should be examined in terms of its net effect on the drug-target interaction.
In brief, the general patterns emerging from case study 2, with which one can make some predictions, in the absence of more specific information, regarding the ADA impact on drug disposition and effectiveness, may be summarized as follows:
-
a.
ADA response is more likely to be a phenomenon at lower doses in terms of being more readily detectable in its unbound form and having greater potential to impact the drug disposition and effectiveness (Fig. 3b, c, and d).
-
b.
The magnitude of ADA response can be uniquely characterized by DoseAddl(ΔAUC = 0), the additional dose required to bring the unbound drug exposure to the same level as in the absence of ADA response (Fig. 3a, b, and c).
-
c.
The PK alteration based on unbound drug exposure tends to exaggerate the efficacy consequences for mAbs with high affinity to the target (Fig. 3a and e).
-
d.
Supersensitive unbound assays may not be very useful for identifying patients with meaningful alterations of the drug disposition/effectiveness due to the ADA response (Fig. 3d).
Case Study 3
Case study 3 showed an example of utilizing the proposed framework for predicting the efficacy consequences of the ADA response that would occur in the supposed late-stage trials with a longer treatment duration, from a perspective of dose optimization. It was shown that there would be more patients who were ADA positive and at higher ADA levels as the treatment went beyond 6 months. Additionally, the impact on the LDL-C lowering effect increased as the ADA further developed, with 5% patients in the top ADA response group suffering from an increased loss of efficacy by approximately 60% at the end of the 12-month treatment (Fig. 4c). Figure 4d supported a dose adaptation study aimed at having the small portion of individuals with the highest ADA response benefit from the full efficacy. In this case, with a 70% dose increase beginning on day 126 by which their ADA levels had been markedly higher than the rest population, those in the top 5% group were able to achieve comparable LDL-C lowering effects to the bottom 50% group with no or negligible ADA response. In addition, with the increased dose, the same unbound ADA assay would reflect considerably lower ADA response for otherwise the same group of individuals (Fig. 4d). Perhaps more importantly, the unbound ADA levels/titers can be utilized in identifying individuals for whom the base dose is no longer adequate due to the ADA response (also see the “Case Study 1” section).
While a thorough debate on the dose optimization strategy is outside the scope of this case study, the proposed framework offers a quantitative way to understand how the efficacy consequences of ADA response can be seriously underestimated during the early development stages, where the study durations are often limited relative to the time required for capturing the full ADA development, and how the immunogenicity testing and its consequences can be profoundly affected by the dose. Without this understanding, one would likely be surprised by the unexpectedly high ADA impact occurring in late-stage clinical trials with longer treatment durations, and, as a result, left with little or no opportunities for dose optimization considerations.
Conclusion
A mAb disposition framework was proposed which revolves around the dynamics of ADA formation and drug’s interactions with the ADA and target as parts of the drug distribution and elimination processes. The disposition framework described well the PK, ADA, and clinical response data from a phase 3 trial in RA patients treated with adalimumab. The framework offered a generalized understanding of how the dose, along with other factors, affects the manifestation of ADA response with regard to its detections and alterations of drug disposition and effectiveness. In addition, as an example, its utility for dose optimization considerations was demonstrated through predicting for late-stage trials of a PCSK9 inhibitor with longer treatment durations, in terms of further developments in ADA incidence and titers, and consequences on the drug disposition and interaction with PCSK9, as well as the LDL-C lowering effect.
Data Availability
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de-identified patient data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
References
Lu RM, Hwang YC, Liu IJ, Lee CC, Tsai HZ, Li HJ, et al. Development of therapeutic antibodies for the treatment of diseases. J Biomed Sci. 2020;27(1):1. https://doi.org/10.1186/s12929-019-0592-z.
Lyu X, Zhao Q, Hui J, Wang T, Lin M, Wang K, et al. The global landscape of approved antibody therapies. Antib Ther. 2022;5(4):233–57. https://doi.org/10.1093/abt/tbac021.
Hansel TT, Kropshofer H, Singer T, Mitchell JA, George AJ. The safety and side effects of monoclonal antibodies. Nat Rev Drug Discov. 2010;9(4):325–38. https://doi.org/10.1038/nrd3003.
Vaisman-Mentesh A, Rosenstein S, Yavzori M, Dror Y, Fudim E, Ungar B, et al. Molecular landscape of anti-drug antibodies reveals the mechanism of the immune response following treatment with TNFalpha antagonists. Front Immunol. 2019;10:2921. https://doi.org/10.3389/fimmu.2019.02921.
Vincent FB, Morand EF, Murphy K, Mackay F, Mariette X, Marcelli C. Antidrug antibodies (ADAb) to tumour necrosis factor (TNF)-specific neutralising agents in chronic inflammatory diseases: a real issue, a clinical perspective. Ann Rheum Dis. 2013;72(2):165–78. https://doi.org/10.1136/annrheumdis-2012-202545.
Bloem K, Hernandez-Breijo B, Martinez-Feito A, Rispens T. Immunogenicity of therapeutic antibodies: monitoring antidrug antibodies in a clinical context. Ther Drug Monit. 2017;39(4):327–32. https://doi.org/10.1097/FTD.0000000000000404.
Gunn GR 3rd, Sealey DC, Jamali F, Meibohm B, Ghosh S, Shankar G. From the bench to clinical practice: understanding the challenges and uncertainties in immunogenicity testing for biopharmaceuticals. Clin Exp Immunol. 2016;184(2):137–46. https://doi.org/10.1111/cei.12742.
Nelson AL, Dhimolea E, Reichert JM. Development trends for human monoclonal antibody therapeutics. Nat Rev Drug Discov. 2010;9(10):767–74. https://doi.org/10.1038/nrd3229.
Shankar G, Arkin S, Cocea L, Devanarayan V, Kirshner S, Kromminga A, et al. Assessment and reporting of the clinical immunogenicity of therapeutic proteins and peptides-harmonized terminology and tactical recommendations. AAPS J. 2014;16(4):658–73. https://doi.org/10.1208/s12248-014-9599-2.
US Food and Drug Administration. Immunogenicity testing of therapeutic protein products —developing and validating assays for anti-drug antibody detection Guidance for Industry <https://www.fda.gov/media/119788/download> (2019). Accessed November 13, 2023.
Wadhwa M, Knezevic I, Kang HN, Thorpe R. Immunogenicity assessment of biotherapeutic products: An overview of assays and their utility. Biologicals. 2015;43(5):298–306. https://doi.org/10.1016/j.biologicals.2015.06.004.
Wang YM, Wang J, Hon YY, Zhou L, Fang L, Ahn HY. Evaluating and reporting the immunogenicity impacts for biological products–a clinical pharmacology perspective. AAPS J. 2016;18(2):395–403. https://doi.org/10.1208/s12248-015-9857-y.
Sailstad JM, Amaravadi L, Clements-Egan A, Gorovits B, Myler HA, Pillutla RC, et al. A white paper–consensus and recommendations of a global harmonization team on assessing the impact of immunogenicity on pharmacokinetic measurements. AAPS J. 2014;16(3):488–98. https://doi.org/10.1208/s12248-014-9582-y.
van Schouwenburg PA, Kruithof S, Votsmeier C, van Schie K, Hart MH, de Jong RN, et al. Functional analysis of the anti-adalimumab response using patient-derived monoclonal antibodies. J Biol Chem. 2014;289(50):34482–8. https://doi.org/10.1074/jbc.M114.615500.
Liao KH, Udata C, Yin D, Sewell KL, Kantaridis C, Alvarez DF, et al. A mechanistic pharmacokinetic model with drug and antidrug antibody interplay, and its application for assessing the impact of immunogenicity response on bioequivalence testing. Br J Clin Pharmacol. 2020;86(11):2182–91. https://doi.org/10.1111/bcp.14312.
Udata C, Garzone PD, Gumbiner B, Joh T, Liang H, Liao KH, et al. A mechanism-based pharmacokinetic/pharmacodynamic model for bococizumab, a humanized monoclonal antibody against proprotein convertase subtilisin/kexin type 9, and its application in early clinical development. J Clin Pharmacol. 2017;57(7):855–64. https://doi.org/10.1002/jcph.867.
Williams JH, Udata C, Ganguly BJ, Bucktrout SL, Joh T, Shannon M, et al. Model-based characterization of the pharmacokinetics, target engagement biomarkers, and immunomodulatory activity of PF-06342674, a humanized mAb against IL-7 receptor-alpha, in adults with type 1 diabetes. AAPS J. 2020;22(2):23. https://doi.org/10.1208/s12248-019-0401-3.
Savic RM, Jonker DM, Kerbusch T, Karlsson MO. Implementation of a transit compartment model for describing drug absorption in pharmacokinetic studies. J Pharmacokinet Pharmacodyn. 2007;34(5):711–26. https://doi.org/10.1007/s10928-007-9066-0.
Fleischmann RM, Alten R, Pileckyte M, Lobello K, Hua SY, Cronenberger C, et al. A comparative clinical study of PF-06410293, a candidate adalimumab biosimilar, and adalimumab reference product (Humira(R)) in the treatment of active rheumatoid arthritis. Arthritis Res Ther. 2018;20(1):178. https://doi.org/10.1186/s13075-018-1676-y.
Hutmacher MM, Krishnaswami S, Kowalski KG. Exposure-response modeling using latent variables for the efficacy of a JAK3 inhibitor administered to rheumatoid arthritis patients. J Pharmacokinet Pharmacodyn. 2008;35(2):139–57. https://doi.org/10.1007/s10928-007-9080-2.
Williams JH, Hutmacher MM, Zierhut ML, Becker JC, Gumbiner B, Spencer-Green G, et al. Comparative assessment of clinical response in patients with rheumatoid arthritis between PF-05280586, a proposed rituximab biosimilar, and rituximab. Br J Clin Pharmacol. 2016;82(6):1568–79. https://doi.org/10.1111/bcp.13094.
Ballantyne CM, Neutel J, Cropp A, Duggan W, Wang EQ, Plowchalk D, et al. Results of bococizumab, a monoclonal antibody against proprotein convertase subtilisin/kexin type 9, from a randomized, placebo-controlled, dose-ranging study in statin-treated subjects with hypercholesterolemia. Am J Cardiol. 2015;115(9):1212–21. https://doi.org/10.1016/j.amjcard.2015.02.006.
Ridker PM, Tardif JC, Amarenco P, Duggan W, Glynn RJ, Jukema JW, et al. Lipid-reduction variability and antidrug-antibody formation with bococizumab. N Engl J Med. 2017;376(16):1517–26. https://doi.org/10.1056/NEJMoa1614062.
Kierzek AM, Hickling TP, Figueroa I, Kalvass JC, Nijsen M, Mohan K, et al. A quantitative systems pharmacology consortium approach to managing immunogenicity of therapeutic proteins. CPT Pharmacometrics Syst Pharmacol. 2019;8(11):773–6. https://doi.org/10.1002/psp4.12465.
van Schouwenburg PA, van de Stadt LA, de Jong RN, van Buren EE, Kruithof S, de Groot E, et al. Adalimumab elicits a restricted anti-idiotypic antibody response in autoimmune patients resulting in functional neutralisation. Ann Rheum Dis. 2013;72(1):104–9. https://doi.org/10.1136/annrheumdis-2012-201445.
Maini RN, Breedveld FC, Kalden JR, Smolen JS, Davis D, Macfarlane JD, et al. Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 1998;41(9):1552–63. https://doi.org/10.1002/1529-0131(199809)41:9%3c1552::AID-ART5%3e3.0.CO;2-W.
Shin D, Lee Y, Kim H, Kornicke T, Fuhr R. A randomized phase I comparative pharmacokinetic study comparing SB5 with reference adalimumab in healthy volunteers. J Clin Pharm Ther. 2017;42(6):672–8. https://doi.org/10.1111/jcpt.12583.
Palaparthy R, Udata C, Hua SY, Yin D, Cai CH, Salts S, et al. A randomized study comparing the pharmacokinetics of the potential biosimilar PF-06438179/GP1111 with Remicade(R) (infliximab) in healthy subjects (REFLECTIONS B537–01). Expert Rev Clin Immunol. 2018;14(4):329–36. https://doi.org/10.1080/1744666X.2018.1446829.
Shin D, Kim Y, Kim YS, Kornicke T, Fuhr R. A randomized, phase I pharmacokinetic study comparing SB2 and infliximab reference product (Remicade((R))) in healthy subjects. BioDrugs. 2015;29(6):381–8. https://doi.org/10.1007/s40259-015-0150-5.
Pivot X, Curtit E, Lee YJ, Golor G, Gauliard A, Shin D, et al. A randomized phase I pharmacokinetic study comparing biosimilar candidate SB3 and trastuzumab in healthy male subjects. Clin Ther. 2016;38(7):1665-73 e3. https://doi.org/10.1016/j.clinthera.2016.06.002.
Yin D, Barker KB, Li R, Meng X, Reich SD, Ricart AD, et al. A randomized phase 1 pharmacokinetic trial comparing the potential biosimilar PF-05280014 with trastuzumab in healthy volunteers (REFLECTIONS B327–01). Br J Clin Pharmacol. 2014;78(6):1281–90. https://doi.org/10.1111/bcp.12464.
Acknowledgements
We would like to thank Timothy Nicholas for his review of the manuscript and Sherry Cai for her assistance in validations of the adalimumab and ADA assays and analyses of the clinical samples.
Funding
This work was sponsored by Pfizer.
Author information
Authors and Affiliations
Contributions
J.H.W., K.H.L., D.Y., and X.M. designed the research and wrote the manuscript. J.H.W., K.H.L., and X.M. performed the research and analyzed the data.
Corresponding author
Ethics declarations
Conflict of Interest
J.H.W. and D.Y. are employees of Pfizer and hold Pfizer stock. K.H.L. and X.M. were employees of Pfizer at the time of this analysis and hold Pfizer stock.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jason H. Williams and Kai H. Liao contributed equally to this work.
ClinicalTrials.gov ID: NCT02480153.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Williams, J.H., Liao, K.H., Yin, D. et al. Implications of Immunogenicity Testing for Therapeutic Monoclonal Antibodies: A Quantitative Pharmacology Framework. AAPS J 26, 31 (2024). https://doi.org/10.1208/s12248-024-00901-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-024-00901-1