Abstract
During biotherapeutic drug development, immunogenicity is evaluated by measuring anti-drug antibodies (ADAs). The presence and magnitude of ADA responses is assessed using a multi-tier workflow where samples are screened, confirmed, and titered. Recent reports suggest that the assay signal to noise ratio (S/N) obtained during the screening tier correlates well with titer. To determine whether S/N could more broadly replace titer, anonymized ADA data from a consortium of sponsors was collected and analyzed. Datasets from clinical programs with therapeutics of varying immunogenicity risk levels (low to high), common ADA assay platforms (ELISA and MSD) and formats (bridging, direct, solid-phase extraction with acid dissociation), and titration approaches (endpoint and interpolated) were included in the analysis. A statistically significant correlation between S/N and titer was observed in all datasets, with a strong correlation (Spearman’s r > 0.8) in 11 out of 15 assays (73%). For assays with available data, conclusions regarding ADA impact on pharmacokinetics and pharmacodynamics were similar using S/N or titer. Subject ADA kinetic profiles were also comparable using the two measurements. Determination of antibody boosting in patients with pre-existing responses could be accomplished using similar approaches for titer and S/N. Investigation of factors that impacted the accuracy of ADA magnitude measurements revealed advantages and disadvantages to both approaches. In general, S/N had superior precision and ability to detect potentially low affinity/avidity responses compared to titer. This analysis indicates that S/N could serve as an equivalent and in some cases preferable alternative to titer for assessing ADA magnitude and evaluation of impact on clinical responses.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The assessment of immunogenicity of biotherapeutics is a regulatory requirement to determine the effects of anti-drug antibodies (ADA) on patient safety, drug concentrations, or product efficacy. A multi-tiered approach for ADA characterization is typically used in clinical trials (1). In this approach, the magnitude of ADA response is characterized by testing a serial dilution of confirmed positive samples to obtain titer values. The titer value of a given sample is expressed as the reciprocal of the highest dilution that still yields a positive result in the assay (endpoint titer) or as an interpolated value from the sample dilution curve at a predetermined cut point (interpolated titer) (2).
Titer has been widely applied in the pharmaceutical industry and medical community as an indirect way to measure antibody levels in clinical samples. Historically, many legacy clinical serological tests, such as viral hemagglutination and complement fixation test assays, utilized titer values guided by references specific to a particular antigen or antibody (3, 4). The first generation of ADA assays were ELISAs, with limited sensitivity and dynamic range that required sample titration to assess response magnitude (5). Current industry-standard ADA assays have significantly improved sensitivity (low ng/mL) and dynamic range (several orders of magnitude) compared to older techniques such as ELISA (6). These technological advances, combined with the generally lower magnitude of ADA responses to biologics compared to vaccines, may reduce the need for titration.
While titer determination is useful for the stratification of ADA levels and evaluation of their impact on safety and efficacy, it can suffer from multiple limitations. Additional manipulation of the sample and interpolation of titer results from signals located in the lower plateau of the assay range often result in poor precision. The endpoint titer approach may lead to inferior result resolution and an inability to differentiate low-level ADA responses. As titration is the third tier of ADA testing, samples analyzed for titer may have undergone extensive handling (e.g., refrigerated storage, multiple freeze-thaw cycles) which can impact ADA integrity and reproducibility. Titration is performed by diluting samples in a pool of a qualified drug-naïve matrix which may result in foreign matrix components blocking a subset of the ADA population. Titer may not be effective in detecting samples with low-affinity ADA as they may be prone to dilutional nonlinearity. In certain types of studies, such as those with pediatric patients, there may be challenges collecting a sufficient sample volume to allow for three ADA analysis tiers or assessment of other analytes. Finally, performing titration for large clinical studies increases the cost of pharmaceutical development and delays the availability of potentially important patient safety data. While some of these limitations can be avoided by assay optimization (e.g., titer cut point adjustment), it is desirable to identify additional options for measuring the magnitude of ADA to biologic drugs.
A recent report proposes an alternative approach to titer that utilizes the signal to noise ratio (S/N) to assess ADA magnitude in clinical samples (7). S/N is defined as the signal of the sample derived from the screening assay or untreated portion of the confirmatory assay, divided by the signal of the negative control analyzed on the same plate. Normalization of the sample signal using a negative control to represent the biological background reduces sample result variability across plates or runs. This report demonstrated that S/N data correlated well with titer in three clinical trials. In addition, a robust correlation of the assay signal with titer assay results was recently reported for a flow cytometry immunogenicity assay for a chimeric antigen receptor (CAR) T-cell therapeutic (8).
To determine whether the S/N approach could be suitable as an alternative to traditional titer assessment for different therapeutic modalities with varied immunogenicity risk profiles and assay formats, a consortium was formed from nine pharmaceutical and biotechnology companies. Fifteen independent and anonymized clinical ADA datasets provided by the contributing organizations were analyzed for S/N versus titer correlation. In addition, ADA magnitude results determined using both approaches were used to perform the standard ADA characterization analyses including the impact of ADA on pharmacokinetics (PK) and pharmacodynamics (PD) and evaluation of ADA kinetics within a subject.
Materials and Methods
Data Collection
Sponsor companies provided the statistician with therapeutic information, assay characteristics, validation summary data, and study data in a standardized data collection template. Requested study data included S/N and titer results from ADA-positive subjects, PK data (drug concentration of the same sample or same sampling time point corresponding to the ADA result), primary and/or secondary pharmacodynamic marker data (optional), and inter-assay precision data of the positive control and titer assay control. Requested validation data included assay range (positive control dose-response curve results spanning low to high concentrations), inter-assay precision results for S/N and titer, and drug tolerance results for S/N and titer. The statistician anonymized data sources and shared the collated dataset with working group members. Nine sponsor companies contributed data from 15 assays, referred to as assays or datasets A1 to A15 within this manuscript.
ADA Assays
ADA assays were performed according to the format and platform indicated in Table I as described previously (9,10,11,12). S/N was calculated by dividing the mean clinical study sample signal by the mean signal of the negative control analyzed on the same screening assay plate. Titration was performed by serially diluting samples in pooled serum using a 2-fold dilution scheme. Titer results were determined by linear interpolation at the titer cut point from dilutions producing signals above and below the titer cut point (interpolated titer) or by reporting the reciprocal of the last dilution testing above the titer cut point (endpoint titer).
Assay Validation Parameters
ADA assays were validated according to applicable white papers and regulatory agency guidance available at the time of validation (1, 13, 14). For the purposes of this analysis, assay precision (%CV) was based on in-study precision data for the low and high positive controls (S/N) or the titer positive control whenever possible. For assays that lacked in-study precision data for both measurements, precision was estimated using sensitivity curve data when at least 6 separate runs were available. S/N precision was based on the highest %CV detected across any concentration producing values above the assay cut point. For titer precision, the serial dilution of the highest concentration of the sensitivity curve was used to determine a titer result according to the method used for clinical samples. Titer inter-assay precision was based on the %CV of the titer results. S/N linearity was determined using validation assay range data after confirming that it covered at least 90% of clinical study responses. For concentrations testing above the screening assay cut point, acceptable linearity was concluded if the observed S/N value, after subtracting 1 for background (i.e., S/N − 1), was within ±50% of the S/N value expected based on the next lower concentration and the dilution factor. The percentage of samples located in the upper S/N assay plateau of clinical study data was calculated by dividing the number of samples that had a differentiation of titer values accompanied by saturation of S/N values divided by the total number of samples. Drug impact on ADA magnitude measurements was not evaluable for most assays because it was not determined for titer results in any assay validations. In addition, the impact of drug on S/N could not be assessed for most assays as the lowest drug concentrations that had an impact on S/N recovery during validation were higher than drug concentrations present in clinical study samples.
Statistical Analysis
The strength of the relationship between S/N and titer, and S/N or titer and PK or PD, was assessed using log-transformed S/N, titer, PK, and PD data and Spearman’s rank correlation coefficient (r). ADA-positive samples that had both a S/N and titer result were used in the analysis. Very strong and moderate correlation were defined as Spearman’s r > 0.8 and r > 0.6, respectively (15). Correlations with p-value < 0.05 were considered statistically significant. For correlation of S/N or titer vs. PK or PD, datasets that had nonzero PK or PD data available for at least 50% of ADA-positive samples were included in the analysis (6 out of 15 assays for PK, and 3 out of 15 assays for PD).
One assay (A7) was selected for more detailed PK association analysis as it had a rich dataset due to intense PK/ADA sampling and available dosing information. For this analysis, drug trough concentrations were dose-normalized to the actual dose given and ADA responses were stratified into S/N or titer quartiles (2). The small sample size of each subgroup precluded the application of statistics for subgroup comparison.
Evaluation of ADA Kinetics and Treatment Boosting in Pre-existing Antibody-Positive Subjects
Within each dataset, the subject with the highest S/N response and at least 4 available time points was selected for the evaluation of the kinetics of ADA development over time. Titer and S/N values were plotted on the left and right y-axes, respectively.
Dataset A15 was selected as a case study for treatment boosting because it contained the highest number of pre-existing antibody-positive subjects with full ADA profiles. As the provided titer results only captured the titration dilution, these results were multiplied by the assay’s minimum required dilution (MRD) (100) to reflect current guidance for titer reporting (1). Samples producing S/N values between the screening and titer cut points and samples whose first dilution tested below the titer cut point were reported with a titer result equivalent to the MRD (16). To calculate the fold increase in ADA magnitude following drug exposure, the postdose result (titer, S/N, or S/N − 1) was divided by the pre-dose result. Treatment boosting was determined by applying a simple criterion (4-fold, to reflect the 2-fold endpoint titer dilution scheme for this method) or the minimum significant ratio (MSR). The median MSR was calculated using in-study log-transformed low and high positive control S/N or S/N − 1 values as described in (16). In-study precision data was used because validation data covering precision across a wide range of ADA magnitudes was not available for this dataset.
Results
Clinical Dataset Characteristics and S/N vs. Titer Correlations
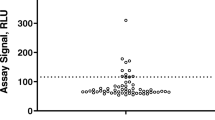
Fifteen datasets from nine different sponsors were assessed for correlation of the ADA magnitude outputs measured as either S/N or titers. ADA results were derived from ELISA- or MSD-based platforms, represented multiple assay formats (13 bridging, 1 indirect, and 1 SPEAD), and spanned diverse modalities of biologics including monoclonal antibodies, fusion proteins, and bispecifics (Table I). The treatment-emergent clinical immunogenicity incidences varied from low (2%) to high (100%) in autoimmune, oncology, and inflammatory disease indications. A statistically significant correlation between S/N and titer values was observed in all 15 assays (Table II and Fig. 1). In 11 out of 15 assays (73%), the correlation was very strong (Spearman’s r > 0.8). In 14 out of 15 assays (93%), the correlation was moderate to strong (Spearman’s r > 0.6).
Impact on PK and PD
The impact of immunogenicity (by either S/N or titer) on pharmacokinetics (PK) and/or pharmacodynamic (PD) markers was assessed for 6 and 3 of the datasets, respectively. A modest negative correlation between ADA level and PK was observed for most datasets with the strongest correlation detected for dataset A7 (Table II). The negative correlation indicates a decline in drug concentrations with the increase in ADA magnitude as measured by either S/N or titer. For most cases, S/N and titer had comparable levels of correlation with PK.
Similar conclusions for impact of ADA on PD were also found in the 3 datasets using S/N and titer (Table II). For datasets A4 and A6, a decline in PD marker levels was associated with an increase in ADA magnitude whether measured by S/N or titer. Another PD marker (PD2) for dataset A6 was not significantly correlated with ADA magnitude, whether measured by S/N or titer. Finally, dataset A2 showed a positive correlation of increased PD marker levels associated with increased ADA titer and S/N.
A more detailed analysis of the association of ADA with PK was performed using the A7 dataset by grouping ADA-positive subjects into quartiles based on their magnitudes. A similar trend of decreasing drug trough concentrations was detected as the ADA magnitude increased across the first and second quartiles of S/N or titer, with the lowest drug trough concentrations present in the third and fourth quartiles (Fig. 2).
Impact of ADA magnitude on dose-normalized drug mean trough concentrations for assay A7. Each box plot shows the distribution of drug concentrations as lower extreme (lower whisker), first quartile (lower hinge), median (middle line), mean (open diamond), third quartile (upper hinge), and upper extreme (upper whisker). The outliers (>1.5 times the box length) are shown as closed circles. Q1 to Q4 indicate S/N or titer quartiles
Overall, the evaluation of impact of immunogenicity on PK or PD markers produced the same conclusions independent of the approach used to assess ADA magnitude (S/N or titer).
ADA Kinetics and Pre-existing Antibody Boosting
ADA magnitude results are used to monitor ADA kinetics within a subject over the course of the study. Titer and S/N values were plotted over time for the subject with the highest S/N and at least four positive postdose time points within each dataset (Fig. 3). For the majority of samples in all assays, a similar trend of increasing or decreasing ADA response was observed compared to the previous time point regardless of whether S/N or titer was used.
In subjects with pre-existing antibodies, ADA magnitude results can also be used to determine whether there was an increase in antibody response following drug administration, referred to as treatment boosting. Recommendations for criteria used to define a significant increase in the ADA response in a postdose sample compared to a pre-dose sample have been described in regulatory guidance and white papers (1, 2). For methods using endpoint titer, an increase in postdose titer equal to or greater than 2 dilution steps (e.g., 4-fold or 9-fold, depending on the titration dilution scheme) is defined as treatment-boosted. For methods using interpolated titer, the proposed criterion for treatment boosting is based on the minimum significant ratio (MSR), a measure of assay variability calculated using validation precision data.
These criteria for treatment boosting were evaluated for both measures of ADA magnitude (S/N and titer) using a clinical dataset with the highest number of pre-existing positive subjects (A15). Treatment boosting was determined by applying the 4-fold or the MSR criterion to postdose titer or S/N results. In addition, as the S/N measure includes the contribution of the assay background, which is not expected to increase following drug administration, determination of boosting was also performed using pre-dose and postdose S/N values after subtracting the background (S/N − 1). Treatment boosting results are shown in Table III for four subjects representing each scenario encountered in the study. In two subjects, the timing of detection of initial treatment boosting was different depending on which measure of ADA magnitude (titer, S/N, or S/N − 1) was used. For subject 17, S/N and S/N − 1 approaches identified treatment boosting at an earlier time point (day 15) compared to titer (day 169). For subject 16, the S/N − 1 or the S/N approach combined with the MSR criterion was the only method that resulted in determination of treatment boosting at an early ADA time point (day 29). Both of these subjects had very low pre-existing antibody responses just above the screening assay cut point. At later study time points in subjects 16 and 17 and at all time points for subjects 1 and 46, treatment boosting conclusions were equivalent irrespective of the ADA magnitude measure or boosting criteria.
Factors That Impact Titer and S/N Assessments
S/N Signal Plateau with High ADA Responses
Most assays had an adequate S/N assay range, as the clinical data demonstrated good titer and S/N correlation throughout the response range including at high titer (Fig. 1) and acceptable S/N linearity during validation (Table IV). Datasets A4, A8, A10, A14, and A15 had a strong overall correlation of S/N and titer; however, there was some evidence of a S/N plateau (Fig. 1). Four of these assays (A8, A10, A14, and A15) used the MSD platform with a much wider dynamic range compared to spectrophotometric ELISAs. In these cases, saturation of the S/N response occurred at very high S/N values (S/N > 1000) and affected only a small number of clinical study samples (between 2 and 9%; Table IV). Dataset A4, however, used an ELISA platform and saturation occurred at fairly low S/N values (S/N ~ 20) and impacted 37% of study samples.
Three of the MSD assays (A8, A10, and A15) had assay range validation data spanning the breadth of clinical ADA responses. Nonlinearity of the positive control S/N response during method validation was detected starting at approximately the same level seen in clinical study data. For example, study S/N responses in assay A8 did not show signs of saturation below S/N ~ 1000 (Fig. 1). Similarly, positive control S/N responses during validation were also linear up until S/N ~ 1000 (Supplemental Figure 1).
Improved Precision of S/N Measurements Compared to Titer
Precision is a critical component for any assay, including for ADA magnitude determination. In-study precision data was available for low and high positive controls (S/N precision) and titer positive control (titer result precision) for three datasets. In all these cases, precision of S/N was substantially better than titer precision (Table IV, bold values). For the two methods using endpoint titer or one method using interpolated titer, the titer positive control varied 4-fold or 2-fold from the median value, respectively. Within those methods, sample titer results can be expected to deviate up to 4-fold from the true result. The remaining datasets did not monitor titer precision during clinical sample analysis and did not formally evaluate this parameter during validation. For those assays, titer precision was estimated using sensitivity curves which included a serial dilution (titration) of the positive control across at least 6 separate runs. Although this approach underestimates titer imprecision as the highest point of the curve was generally at a low to medium concentration, in all evaluable assays, titer precision was inferior to S/N precision.
Titer imprecision can impact samples with high ADA responses due to the extensive serial dilution required to produce the titer result. In addition, samples with low ADA responses suffer from poor titer result resolution, especially when endpoint titer is used. In assay A11 (S/N vs. titer correlation Spearman’s r = 0.618), almost 90% of the samples had low-titer ADA responses (MRD or the next lowest dilution) and the less robust correlation was likely due to the inherent lack of endpoint titer resolution within the lower range of the assay.
Although interpolated titer is preferable to endpoint titer in terms of improved result resolution, it can also be imprecise due to sample manipulation and result interpolation in the lower assay range. In dataset A7, the titer cut point was located in the lower plateau of the assay (equivalent to the screening cut point). Several subjects in this dataset had individual time points for which the titer result did not match the S/N measurement and noticeably deviated from the rest of the subject’s ADA profile (Supplemental Figure 2a, red circles), suggesting titer imprecision.
Drug and Target Interference
Drug interference with either S/N or titer measurements can also impact the accuracy of ADA magnitude results. Although all assays evaluated drug tolerance in terms of the ability to correctly detect positives in the presence of drug, the impact of drug on titer results was not tested in any of the assay validations. Despite acceptable overall drug tolerance in terms of identifying positives, S/N results were affected to some degree by the presence of drug in most assays. However, the lowest drug levels tested in validation were much higher than drug levels detected in clinical study samples. Therefore, the effect of drug on ADA magnitude measurements (S/N or titer) could not be robustly evaluated using validation data. In one assay (A3; S/N vs. titer correlation Spearman’s r = 0.553), the validated drug tolerance limit was close to or below drug concentrations present in study samples, suggesting that circulating drug may have interfered with S/N and/or titer measurements. In addition, this dataset had the smallest sample size and narrow range of positive responses, which may have impacted endpoint titer accuracy.
Another assay with a less robust S/N vs. titer correlation (A12, Spearman’s r = 0.697) was reported to have significant target interference, requiring an additional target confirmatory assay and potentially affecting the correlation analysis.
Low Affinity/Avidity Responses
Clinical data from assays A1, A2, A5, and A8 suggests that the screening (S/N) and titer tiers may capture the contributions of affinity/avidity on final results differently. In these datasets, a small subset of confirmed positive samples had relatively high S/N values but low titer values (equivalent to the MRD or within 2 dilutions; Fig. 1). Interestingly, all of these samples were from subjects that were either positive for pre-existing antibodies and/or treated with placebo. In assays A5 and A8, pre-existing positive subjects had significant increases in S/N values postdose despite titer results remaining low (Supplemental Figure 2b). Upon dilution in the titer assay, these potentially lower affinity/avidity antibodies could dissociate faster or be blocked by the exogenous matrix added during titration. S/N may therefore be preferable for appropriate quantification of at least a subset of ADA responses that may be prone to dilutional nonlinearity.
Discussion
Sample titration is a valuable tool to assess the magnitude of response in assays with readouts that have a limited dynamic range or for measurement of the significantly higher immune responses to vaccines compared to biologics. However, titration-based methods are operationally more complex and have numerous drawbacks that are frequently overlooked. Plate-based immunoassays with numerical responses as a readout (S/N) and the advent of new technologies — such as electrochemiluminescence (ECL), the use of bridging assay formats, and novel approaches to minimize drug interference — have improved the concentration-response range, sensitivity, specificity, and drug tolerance of immunogenicity assays. These advances enable the evaluation of the assay S/N ratio as a simpler alternative to titration.
This study found a statistically significant correlation of S/N and titer in all 15 clinical immunogenicity datasets representing various biotherapeutic modalities, with a very strong correlation (Spearman’s r > 0.8) in 11 out of 15 assays (73%). Cases where a less robust (but still positive) correlation was observed revealed factors that impacted accuracy for either titer or S/N (or both), suggesting that titer may not always be the gold standard for evaluating magnitude of an ADA response.
Broad dynamic range was determined to be the most important assay requirement for the use of S/N. Compared to the limited range of ELISAs, which may be problematic, the wide dynamic range of the electrochemiluminescence-based (MSD) platform was suitable for accurate measurement of the majority of clinical ADA responses. Responses that were located in the upper plateau of the MSD assay signal comprised a small number (<10%) of study samples. Although these responses were not in the linear assay range, they would nevertheless be categorized in the high–ADA magnitude group and therefore not affect the overall impact analysis conclusions. Due to the high sensitivity of the MSD platform, the assay range can be proactively optimized during method development by increasing the assay’s MRD and/or adjusting the concentration of capture and detection reagents (biotin- and ruthenium-labeled drug). Consequently, when the validated assay has an adequate dynamic range (e.g., >3-logs), and is confirmed to cover the majority of clinical study responses (e.g., >80%), a sample titration step is not technically necessary.
Secondary assay parameters that can be evaluated during validation of both approaches are precision and drug interference. In our analysis, S/N precision was found to be superior to titer precision. Titer imprecision results from a number of factors: the large dilutions required for samples with high ADA, the lack of resolution of endpoint titer across the response range but especially in the lower assay plateau, and the addition of exogenous matrix to clinical study samples during titration. Although the presence of high levels of drug can interfere with both measurements, it may impact S/N to a greater extent than titer (7). However, it may only affect a subset of samples, and assay optimization and numerous sample pre-treatment approaches can be utilized to minimize drug interference with S/N results (9, 11, 17,18,19). Importantly, the lack of precision in the titer format is likely to impact all ADA samples and may be difficult to mitigate due to the inherent need for extensive sample manipulation. The absence of titer validation data for precision and drug impact for almost all assays in these datasets illustrates the lower validation rigor historically implemented for titer assays. These gaps should be addressed in the future for methods that select the titer format. Similarly, the impact of drug on S/N and not just the ability to detect positives should be validated for methods that select the S/N format. Finally, potential target interference should be evaluated and addressed during method development to ensure the accuracy of both measures of ADA magnitude.
One of the main analyses performed using semi-quantitative ADA data is the assessment of its potential impact on PK and/or PD. The objective of the impact analysis in this manuscript was to determine if the use of S/N instead of titer would change the conclusions, rather than to illustrate best practices for impact analysis which would require more comprehensive datasets (2). In our analysis, comparable conclusions were reached whether S/N or titer was used to assess the association with PK/PD.
A challenge with the use of S/N is the evaluation of treatment-boosted responses in samples that are positive at baseline. However, titration-based methods suffer from the same limitation. We propose an analogous solution for S/N: a treatment-boosted response must be greater than the baseline response by a reasonable margin (e.g., 2- or 4-fold). Application of this approach would be similar to the current standards for titer methods with 2-fold dilution schemes where treatment-boosted responses must be ≥ 4-fold the baseline titer. This simple criterion would be adequate for most clinical development programs. For therapeutics with a high immunogenicity risk that require early identification of treatment-boosted responses (e.g., therapeutics with an endogenous counterpart), a more complex method (MSR) based on S/N assay variability can be implemented (16). The MSR can be calculated using validation inter-assay precision data for the low, medium, and high positive controls to represent assay variability across various ADA concentrations. To ensure that it reflects long-term assay variability, the MSR can also be revised to incorporate in-study precision data from early phase studies. For the most sensitive detection of boosting, the MSR can be calculated using S/N − 1 (subtracting background) and applied to S/N − 1 sample values. These MSR-based methods are technically more accurate but require assay-specific biostatistics table programming. Furthermore, the S/N MSR is usually very low due to the excellent precision of current ADA methods and may therefore result in a conclusion of boosting for responses that may be minimal and not clinically relevant.
Bioanalytical processes should periodically be scrutinized to ensure they are up to date and continue to provide value. Incurred sample re-analysis (ISR) and duplicate analysis are two examples where extensive examination of industry data has been performed to assess the utility of the established approaches. ISR is intended to confirm that the results from QC samples used during method validation faithfully reflect the data from study samples. Based on health authority guidance (20), ISR is routinely performed for many studies despite evidence that it rarely fails to meet acceptance criteria (21,22,23,24). Similarly, duplicate analysis is the industry standard for ligand-binding assays (LBAs). Extensive comparison of industry data has shown that data generated using singlicate LBA bioanalysis is as robust and reproducible as duplicate analysis, with the obvious advantages of increased throughput and reduced costs (25,26,27,28).
For quantifying the magnitude of ADA responses, published data has demonstrated that with modern assay platforms, the raw assay signal is well correlated with titer results to assess immunogenicity to protein therapeutics and CAR-T therapies (7, 8). The wide-ranging industry datasets compared in this manuscript demonstrate that S/N and titer provide very similar information. S/N may in fact be preferred, for example, to minimize errors and ambiguous results from repeat analysis and to provide better precision than titer measurements. The selection of the optimal ADA magnitude format (S/N or titer) to support clinical studies should be dependent on the evaluation of assay characteristics of both approaches determined during assay development and validation, with an emphasis on assay range followed by drug impact and precision (Fig. 4). A direct comparison of S/N and titer data from clinical studies is not necessary unless a decision cannot be made based on validation data. In such cases, a titration assay can be implemented in early phase studies and replaced by S/N for registrational studies if acceptable performance is observed. Given the novelty of this alternate approach, industry sponsors may need to consult regulators early in program development if opting for S/N over the traditional titer method. In addition, a suitable justification should be provided in the respective ADA assay validation report submitted to eCTD 5.3.1.4 and in other appropriate sections such as in 2.7.1 Summary of Bioanalytical Methods and in 5.3.5.3 Integrated Summary of Immunogenicity.
Bioanalytical best practices should continually evolve to take advantage of new technologies and replace traditional methods. ISR, singlicate analysis, and S/N for ADA assessment are examples where industry-wide evaluation of clinical data has identified potential improvements to current bioanalytical practices. In each case, a new analytical paradigm offers substantial potential advantages — such as decreasing time to data availability, reducing the time and cost of drug development with little or no loss of analytical rigor.
Conclusion
For methods with an adequate assay range, determination of ADA magnitude and evaluation of clinical impact of immunogenicity can be successfully accomplished using the S/N ratio. Implementation of the S/N approach in a program-specific manner should be done with appropriate scientific justification. This simple approach allows a quasi-quantitative readout from the same sample used to determine the screening result, superior precision, improved detection of low affinity/avidity responses, and a more time- and cost-effective analytical workflow.
Abbreviations
- ADAs:
-
Anti-drug antibodies
- ECL:
-
Electrochemiluminescence
- ELISA:
-
Enzyme-linked immunosorbent assay
- mAbs:
-
Monoclonal antibodies
- S/N :
-
Signal to noise ratio (also known as signal-to-negative control ratio)
- MSD:
-
Meso Scale Discovery
- MRD:
-
Minimum required dilution
- PD:
-
Pharmacodynamics
- PK:
-
Pharmacokinetics
- SPEAD:
-
Solid-phase extraction with acid dissociation
References
FDA. Immunogenicity testing of therapeutic protein products — developing and validating assays for anti-drug antibody detection. Guidance for industry. 2019.
Shankar G, Arkin S, Cocea L, Devanarayan V, Kirshner S, Kromminga A, et al. Assessment and reporting of the clinical immunogenicity of therapeutic proteins and peptides-harmonized terminology and tactical recommendations. AAPS J. 2014;16(4):658-673.
Hirst GK. The quantitative determination of influenza virus and antibodies by means of red cell agglutination. J Exp Med. 1942;75(1):49–64.
Adone R, Ciuchini F. Complement fixation test to assess humoral immunity in cattle and sheep vaccinated with Brucella abortus RB51. Clin Diagn Lab Immunol. 1999;6(6):787–90.
Song S, Yang L, Trepicchio WL, Wyant T. Understanding the supersensitive anti-drug antibody assay: unexpected high anti-drug antibody incidence and its clinical relevance. J Immunol Res. 2016;2016:3072586.
Collet-Brose J, Couble PJ, Deehan MR, Nelson RJ, Ferlin WG, Lory S. Evaluation of multiple immunoassay technology platforms to select the anti-drug antibody assay exhibiting the most appropriate drug and target tolerance. J Immunol Res. 2016;2016:5069678.
Starcevic Manning M, Kroenke MA, Lee SA, Harrison SE, Hoofring SA, Mytych DT, et al. Assay signal as an alternative to titer for assessment of magnitude of an antidrug antibody response. Bioanalysis. 2017;9(23):1849-1858.
Potthoff B, McBlane F, Spindeldreher S, Sickert D. A cell-based immunogenicity assay to detect antibodies against chimeric antigen receptor expressed by tisagenlecleucel. J Immunol Methods. 2020;476:112692.
Patton A, Mullenix MC, Swanson SJ, Koren E. An acid dissociation bridging ELISA for detection of antibodies directed against therapeutic proteins in the presence of antigen. J Immunol Methods. 2005;304(1-2):189–95.
Brickelmaier M, Hochman PS, Baciu R, Chao B, Cuervo JH, Whitty A. ELISA methods for the analysis of antibody responses induced in multiple sclerosis patients treated with recombinant interferon-beta. J Immunol Methods. 1999;227(1-2):121–35.
Smith HW, Butterfield A, Sun D. Detection of antibodies against therapeutic proteins in the presence of residual therapeutic protein using a solid-phase extraction with acid dissociation (SPEAD) sample treatment prior to ELISA. Regul Toxicol Pharmacol. 2007;49(3):230–7.
Mire-Sluis AR, Barrett YC, Devanarayan V, Koren E, Liu H, Maia M, et al. Recommendations for the design and optimization of immunoassays used in the detection of host antibodies against biotechnology products. J Immunol Methods. 2004;289(1-2):1-16.
Shankar G, Devanarayan V, Amaravadi L, Barrett YC, Bowsher R, Finco-Kent D, et al. Recommendations for the validation of immunoassays used for detection of host antibodies against biotechnology products. J Pharm Biomed Anal. 2008;48(5):1267-1281.
EMA. Guideline on Immunogenicity assessment of biotechnology-derived therapeutic proteins (Draft) 2015.
Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18(3):91–3.
USP. United States Pharmacopoiea General Chapter 1106: immunogenicity assays – design and validation of immunoassays to detect anti-drug antibodies. 2014. p. 909–22
Bourdage JS, Cook CA, Farrington DL, Chain JS, Konrad RJ. An affinity capture elution (ACE) assay for detection of anti-drug antibody to monoclonal antibody therapeutics in the presence of high levels of drug. J Immunol Methods. 2007;327(1-2):10–7.
Xu W, Sank M, Cummings J, Carl S, Juhel M, Gleason C, et al. Bead-extraction and heat-dissociation (BEHD): a novel way to overcome drug and matrix interference in immunogenicity testing. J Immunol Methods. 2018;462:34-41.
Zoghbi J, Xu Y, Grabert R, Theobald V, Richards S. A breakthrough novel method to resolve the drug and target interference problem in immunogenicity assays. J Immunol Methods. 2015;426:62–9.
EMA. ICH guideline M10 on bioanalytical method validation (draft). 2019.
Lee LB, Wickremsinhe ER. A decade of incurred sample reanalysis: failures, investigations and impact. Bioanalysis. 2018;10(21):1767–72.
Verhaeghe T. ISR: what have we learned after a decade of experience? Bioanalysis. 2018;10(21):1747–53.
Fluhler EN. Incurred sample reanalysis: ‘too much of a good thing?’. Bioanalysis. 2018;10(21):1719–21.
Kall MA, Michi M, van der Strate B, Freisleben A, Stoellner D, Timmerman P. Incurred sample reproducibility: 10 years of experiences: views and recommendations from the European Bioanalysis Forum. Bioanalysis. 2018;10(21):1723–32.
Jiang H, Kozhich A, Cummings J, Gambardella J, Zambito F, Titsch C, et al. Singlicate ligand binding assay using an automated microfluidic system: a clinical case study. AAPS J. 2017;19(5):1461-1468.
Birnboeck HF, Schick E, Justies N. Singlicate analysis in regulated bioanalysis using ligand-binding assays: where are we heading? Bioanalysis. 2017;9(18):1357–9.
Barfield M, Goodman J, Hood J, Timmerman P. European Bioanalysis Forum recommendation on singlicate analysis for ligand binding assays: time for a new mindset. Bioanalysis. 2020;12(5):273–84.
Jiang Z, Kamerud J, You Z, Basak S, Seletskaia E, Steeno GS, et al. Feasibility of singlicate-based analysis in bridging ADA assay on Meso-Scale Discovery platform: comparison with duplicate analysis. Bioanalysis. 2021;13(14):1123-1134.
Acknowledgements
The authors would like to thank the following individuals for their assistance with data collection: Diana Montgomery (Merck), Stefanie Elm and Klaus Brischwein (Amgen), Nicholas Colletti (BMS) and Sarah Simchik (on behalf of BMS), Brittany Timmons (PPD, a part of Thermo Fisher Scientific), Kimberly Zinnack (Biogen). The authors would like to thank the following FDA regulators for their editorial comments: Leopold Kong, Lin Zhou, Haoheng Yan, Joao Pedras-Vasconcelos, Yow-Ming Yan, and Bruce Huang. These editorial comments are not meant to represent official FDA policy.
Funding
Immunogenicity data used in the analysis was derived from assay validations and clinical studies funded by sponsor companies.
Author information
Authors and Affiliations
Contributions
M.S.M., M.H., M.A.P., V.J., J.M., J.R., and V.D. wrote the manuscript. All authors were involved in contributing and interpreting data, reviewed the final version of the manuscript, and have met the criteria for authorship as established by the ICMJE.
Corresponding author
Ethics declarations
Disclaimer
The views expressed in this article are those of the authors and do not reflect the official policy of their employers.
Conflict of Interest
The authors are employees and may hold stock and/or stock options of the companies listed in their respective affiliation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information

Supplementary Figure 1
Linearity of Positive Control S/N Assessed during Validation of Assay A8 Positive control antibody was serially diluted in matrix and analyzed in assay A8. Linearity of S/N was demonstrated up to S/N ~1000. At higher positive control concentrations, lower than expected S/N values were observed, indicating assay saturation. In clinical study samples, an upper S/N plateau was detected above S/N ~1000 (Figure 1). (PNG 22 kb)

Supplementary Figure 2
S/N values are more consistent with ADA kinetic profiles than titer results. A) Examples of likely titer imprecision at individual timepoints (red circles) in 2 subjects from Assay A7. B) Examples of ADA boosting detected with S/N but not titer in 2 subjects in Assay A5 and Assay A8. (PNG 71 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Starcevic Manning, M., Hassanein, M., Partridge, M.A. et al. Comparison of Titer and Signal to Noise (S/N) for Determination of Anti-drug Antibody Magnitude Using Clinical Data from an Industry Consortium. AAPS J 24, 81 (2022). https://doi.org/10.1208/s12248-022-00728-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-022-00728-8