Abstract
A computational model was developed to better understand the impact of elevated skin temperatures on transdermal drug delivery and dermal clearance. A simultaneous heat and mass transport model with emphasis on transdermal delivery system (TDS) applications was developed to address transient and steady-state temperature effects on dermal absorption. The model was tested using representative data from nicotine TDS applied to human skin either in vitro or in vivo. The approximately 2-fold increase of nicotine absorption with a 10°C increase in skin surface temperature was consistent with a 50–65 kJ/mol activation energy for diffusion in the stratum corneum, with this layer serving as the primary barrier for nicotine absorption. Incorporation of a dermal clearance component into the model revealed efficient removal of nicotine via the dermal capillaries at both normal and elevated temperatures. Two-compartment pharmacokinetic simulations yielded systemic drug concentrations consistent with the human pharmacokinetic data. Both in vitro skin permeation and in vivo pharmacokinetics of nicotine delivered from a marketed TDS under normal and elevated temperatures can be satisfactorily described by a simultaneous heat and mass transfer computational model incorporating realistic skin barrier properties and dermal clearance components.








Similar content being viewed by others
References
Scheuplein RJ. Analysis for permeability data for the case of parallel diffusion pathways. Biophys J. 1966;6:1–17.
Blank IH, Scheuplein RJ, MacFarlane DJ. Mechanism of percutaneous absorption III. The effect of temperature on the transport of non-electrolytes across the skin. J Invest Dermatol. 1967;49(6):582–9.
Peck KD, Ghanem A-H, Higuchi WI. The effect of temperature upon the permeation of polar and ionic solutes through human epidermal membrane. J Pharm Sci. 1995;84(8):975–82.
Akomeah F, Nazir T, Martin GP, Brown MB. Effect of heat on the percutaneous absorption and skin retention of three model penetrants. Eur J Pharm Sci. 2004;21:337–45.
Mitragotri S. Temperature dependence of skin permeability to hydrophilic and hydrophobic solutes. J Pharm Sci. 2007;96(7):1832–9.
Wood DG, Brown MB, Jones SA. Understanding heat-facilitated drug transport across human epidermis. Eur J Pharm Biopharm. 2012;81:642–9.
Ashrafi P, Sun Y, Davey N, Wilkinson SC, Moss GP. The influence of diffusion cell type and experimental temperature on machine learning models of skin permeability. J Pharm Pharmacol. 2020;72:197–208.
Prodduturi S, Sadrieh N, Wokovich AM, Doub WH, Westenberger BJ, Buhse L. Transdermal delivery of fentanyl from matrix and reservoir systems: effect of heat and compromised skin. J Pharm Sci. 2010;99:2357–66.
Shin SH, Thomas S, Raney SG, Ghosh P, Hammell DC, El-Kamary SS, et al. In vitro-in vivo correlations for nicotine transdermal delivery systems evaluated by both in vitro skin permeation (IVPT) and in vivo serum phramacokinetics under the influence of transient heat application. J Control Release. 2018;270:76–88.
Gupta SK, Southam M, Hwang SS. System functionality and physicochemical model of fentanyl transdermal system. J Pain Symptom Manag. 1992;7:S17–26.
Vanakoski J, Seppala T, Sievi E, Lunell E. Exposure to high ambient temperature increases absorption and plasma concentrations of transdermal nicotine. Clin Pharmacol Ther. 1996;60:308–15.
Shomaker TS, Zhang J, Ashburn MA. Assessing the impact of heat on the systemic delivery of fentanyl through the transdermal fentanyl delivery system. Pain Med. 2000;1:225–30.
Gourlay GK. Treatment of cancer pain with transdermal fentanyl. Lancet Onol. 2001;2:165–72.
Ashburn MA, Ogden LL, Zhang J, Love G, Basta SV. The pharmacokinetics of transdermal fentanyl delivered with and without controlled heat. J Pain. 2003;4(6):291–7.
Petersen KK, Rousing ML, Jensen C, Arendt-Nielsen L, Gazerani P. Effect of local controlled heat on transdermal delivery of nicotine. Int J Physiol Pathophysiol Pharmacol. 2011;3:236–42.
Moore KJ, Sathyan G, Richarz U, Natarajan J, Vandenbossche J. Randomized 5-treatment crossover study to assess the effects of external heat on serum fentanyl concentrations during treatment with transdermal fentanyl systems. J Clin Pharmacol. 2012;52:1174–85.
Clarys P, Alewaeters K, Jadoul N, Barel A, Manadas RO, Preat V. In vitro percutaneous penetration through hairless rat skin: influence of temperature, vehicle, and penetration enhancers. Eur J Pharm Biopharm 1998;46:279–283.
Oliveira G, Leverett JC, Emamzadeh M, Lane ME. The effect of heat on skin barrier function and in vivo dermal absorption. Int J Pharm. 2014;464:145–51.
Park J-H, Lee J-W, Kim Y-C, Prausnitz MR. The effect of heat on skin permeability. Int J Pharm. 2008;359:94–103.
Klemsdal TO, Gjesdal K, Bredesen J-E. Heating and cooling of the nitroglycerin patch application area modify the plasma level of nitroglycerin. Eur J Clin Pharmacol. 1992;43:625–8.
Gazerani P, Arendt-Nielsen L. Cutaneous vasomotor reactions in response to controlled heat applied in various body regions of healthy humans: evaluation of time course and application parameters. Int J Physiol Pathophysiol Pharmacol. 2011;3:202–9.
Widmer RJ, Stewart RH, Young MF, Laurinec JE, Laine GA, Quick CM. Application of local heat induces capillary recruitment in the pallid bat wing. Am J Phys Regul Integr Comp Phys. 2007;292:R2312–7.
Charkoudian N. Skin blood flow in human thermoregulation: how it works, when it does not, and why. Mayo Clin Proc. 2003;78:603–12.
Boron WF, Boulpaep EL. Medical physiology: a cellular and molecular approach. Philadelphia: Saunders; 2012.
Kellogg DL, Liu Y, Kosiba IF, O'Donnell D. The role of nitric oxide in the vascular effects of local warming of the skin in humans. J Appl Physiol. 1999;86:1185–90.
Pergola PE, Kellogg DL, Johnson JM, Kosiba WA, Solomon DE. Role of sympathetic nerves in the vascular effects of local temperature in human forearm skin. Am J Physiol (Heart). 1993;265:H785–92.
Singh P, Robert MS. Blood flow measurements in skin and underlying tissues by microsphere method-application to dermal pharmacokinetics of polar nonelectrolytes. J Pharm Sci. 1993;82:873–9.
Singh P, Roberts MS. Effects of vasoconstriction on dermal pharmacokinetics and local tissue distribution of compounds. J Pharm Sci. 1994;83:783–91.
Clough GF, Boutsiouki P, Church MK, Michel CC. Effects of blood flow on the in vivo recovery of a small diffusible molecule by microdialysis in human skin. J Pharmacol Exp Ther. 2002;302:681–6.
Higaki K, Nakayama K, Suyama T, Amnuaikit C, Ogawara K, Kimura T. Enhancement of topical delivery of drugs via direct penetration by reducing blood flow rate in skin. Int J Pharm. 2005;288:227–33.
Cross SE, Roberts MS. Dermal blood flow, lymphatics, and binding as determinates of topical absorption, clearance and distribution. In: Riviere JE, editor. Dermal absorption models in toxicology and pharmacology. Boca Raton: CRC Press; 2006. p. 251–82.
Kretsos K, Miller MA, Zamora-Estrada G, Kasting GB. Partitioning, diffusivity and clearance of skin permeants in mammalian dermis. Int J Pharm. 2008;346(1–2):64–79.
Dancik Y, Anissimov YG, Jepps OG, Roberts MS. Convective transport of highly plasma protein bounds drug facilitates direct penetration into deep tissues after topical application. Brit J Clin Pharmacol. 2011;73:564–78.
Anissimov YG, Roberts MS. Modelling dermal drug distribution after topical application in human. Pharm Res. 2011;28:2119–29.
Ibrahim R, Nitsche JM, Kasting GB. Dermal clearance model for epidermal bioavailability calculations. J Pharm Sci. 2012;101:2094–108.
McNeill S, Potts RO, Francoeur ML. Local enhanced topical delivery (LETD) of drugs: does it truly exist? Pharm Res. 1992;9:1422–7.
Dancik Y, Miller M, Jaworska J, Kasting GB. Design and performance of a spreadsheet-based model for estimating bioavailability of chemicals from dermal exposures. Adv Drug Deliv Rev. 2013;65:221–36.
Kapoor Y, Milewski M, Mitra A, Kasting GB. Clarifications: dermal clearance model for epidermal bioavailability calculations. J Pharm Sci. 2016;105:1341–4.
La Count TD, Zhang Q, Murawsky M, Hao J, Ghosh P, Dave K, Raney SG, Talattof A, Kasting GB, Li SK. Evaluation of heat effects on transdermal nictoine delivery in vitro and in silico using heat-enhanced transport model analysis; AAPS Journal, online in advance of print.
Dedrick RL, Flessner MF, Collins JM, Schultz JS. Is the peritoneum a membrane? ASAIO J. 1982;5:1–8.
Gupta E, Wientjes MG, Au JL-S. Penetration kinetics of 2′,3′-dideoxyinosine in dermis is described by the distributed model. Pharm Res. 1995;12:108–12.
Rippe B, Haraldsson B. Transport of macromolecules across microvascular walls: the two-pore theory. Physiol Rev. 1994;74:163–219.
Riviere JE. Pharmacokinetic implications of changing blood flow in skin. J Pharm Sci. 1992;81:601–2.
Ryan TJ. Cutaneous circulation. In: Goldsmith LA, editor. Biochemistry and physiology of the skin. New York: Oxford University Press; 1983. p. 817–77.
Braverman IM. The cutaneous microcirculation: ultrastructure and microanatomical organization. Microcirc. 1997;4(3):329–40.
Pennes HH. Analysis of tissue and arterial blood temperatures in resting human forearm. J Appl Physiol. 1948;1:93–122.
Çetingül MP, Herman C. A heat transfer model of skin tissue for the detection of lesions: sensitivity analysis. Phys Med Biol. 2010;55:5933–51.
Diller KR, Hayes LJ. A finite element model of burn injury in blood-perfused skin. ASME Trans. 1983;105:300–7.
Wilson SB, Spence VA. A tissue heat transfer model for relating dynamic skin temperature changes to physiological parameters. Phys Med Biol. 1988;33:895–912.
Becker SM, Kuznetsov AV. Local temperature rises influence in vivo electroporation pore development: a numerical stratum corneum lipid phase transition model. J Biomech Eng. 2007;129:712–21.
Becker SM, Kuznetsov AV. Numerical assessment of thermal response associated with in vivo skin electroporation: the importance of the composite skin model. J Biomech Eng. 2007;129:330–40.
Pavselj N, Miklavcic D. Resistive heating and electropermeabilization of skin tissue during in vivo electroporation: a coupled nonlinear finite element model. Int J Heat Mass Transf. 2011;54:2294–302.
Mitchell JW, Galvez TL, Hengle J, Myers GE, Siebecker KL. Thermal response of human legs during cooling. J Appl Physiol. 1970;29:859–65.
Elia M. Organ and tissue contribution to metabolic rate. In: Kinney J, Tucker H, editors. Energy metabolism: tissue determinants and cellular corollaries. New York, NY: Raven Press; 1992. p. 61–80.
Wang Z, Ying Z, Bosy-Westphal A, Zhang J, Schautz B, Later W, et al. Specific metabolic rates of major organs and tissues across adulthood: evaluation by mechanistic model of resting energy expenditure. Am J Clin Nutr. 2010;92:1369–77.
Werner J, Buse M. Temperature profiles with respect to inhomogeneity and geometry of human body. J Appl Physiol. 1988;65:1110–8.
Morales M, Rathbun E, Smith R, Pace N. Studies on body composition: II. Theoretical considerations regarding the major tissue components, with suggestions for application to man. J Biol Chem. 1945;158:677–84.
Duck FA. Physical properties of tissue: a comprehensive reference book. London: Academic Press; 1990.
Zhang Q, Murawsky M, LaCount TD, Hao J, Kasting GB, Newman B, et al. Characterization of temperature profiles in skin and transdermal delivery system when exposed to temperature gradients in vivo and in vitro. Pharm Res. 2017;34:1491–504.
Zhang X, Chinkes D, Wolfe R. Measurement of protein metabolism in epidermis and dermis. Am J Physiol Endocrinol Metab. 2003;284:E1191–201.
Duncan RF, Hershey JWB. Protein synthesis and protein phosphorylation during heat stress, recovery and adaptation. J Cell Biol. 1989;109:1467–81.
Arens EA, Zhang H. The skin’s role in human thermoregulation and comfort. In. Indoor Environmental Quality (IEQ). Berkeley, CA: University of California Berkeley; 2006. pp. 560–602.
Wagner JG. Fundamentals of clinical pharmacokinetics. Hamilton, IL: Drug Intelligence Publications; 1975.
EPA. Estimation Program Interface (EPI) Suite v 4.11. U.S. Environmental Protection Agency. Available from: http://www.epa.gov/oppt/exposure/pubs/episuite.
Chen L, Lian G, Han L. Modeling transdermal permeation. Part I. Predicting skin permeability of both hydrophobic and hydrophilic solutes. AICHE J. 2010;56:1136–46.
Baba H, Ueno Y, Hashida M, Yamashita F. Quantitative prediction of ionization effect on human skin permeability. Int J Pharm. 2017;522:222–33.
Potts RO, Guy RH. Predicting skin permeability. Pharm Res. 1992;9:663–9.
Compton R, Sandborn W, Lawson G, Sheets A, Mays D, Zins B, et al. A dose-ranging pharmacokinetic study of nicotine tartrate following single-dose delayed-release oral and intravenous administration. Aliment Pharmacol Ther. 1997;11:865–74.
Mello NK, Peltier MR, Duncanson H. Nicotine levels after IV nicotine and cigarette smoking in men. Exp Clin Psychopharmacol. 2013;21:188–95.
Wang T-F, Kasting GB, Nitsche JM. A multiphase microscopic model for stratum corneum permeability. II. Estimation of physicochemical parameters and application to a large permeability database. J Pharm Sci. 2007;96:3024–51.
Ash R, Barrer RM, Palmer DG. Diffusion in multiple laminates. Brit J Appl Phys. 1965;16:873–84.
Shin SH, Ghosh P, Newman B, Hammell DC, Raney SG, Hassan HE, et al. On the road to development of an in vitro permeation test (IVPT) model to compare heat effects on transdermal delivery systems: exploratory studies with nicotine and fentanyl. Pharm Res. 2017;34:1817–30.
Kasting GB, Miller MA, LaCount TD, Jaworska J. A composite model for the transport of hydrophilic and lipophilic compounds across the skin. J Pharm Sci. 2019;108:337–49.
Zhang Q, Murawsky M, LaCount TD, Hao J, Ghosh P, Raney SG, Kasting GB, Li SK. Evaluation of heat effects on fentanyl transdermal delivery systems using in vitro permeation and in vitro release methods, unpublished data.
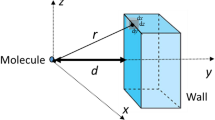
Kretsos K, Kasting GB. A geometrical model of dermal capillary clearance. Math Biosci. 2007;208:430–53.
Calcutt JJ, Anissimov YG. Physiologically based mathematical modeling of solute transport in the epidermis and dermis. Int J Pharm. 2019;569:118547.
Cevc G, Vierl U. Spatial distribution of cutaneous microvasculature and local drugclearance after drug application on the skin. J Control Release. 2007;118:18–26.
Charny CK, Hagmann MJ, Levin RL. A whole body thermal model of man during hyperthermia. IEEE Trans Biomed Eng. 1987;34:375–87.
Johnson JM, Brengelmann GL, Hales JRS, Vanhoutte PM, Wenger CB. Regulation of cutaneous circulation. Fed Proc. 1986;45:2841–50.
Acknowledgments
Funding for this project was made possible, in part, by the US Food and Drug Administration (FDA) through a cooperative agreement (Research Award U01FD004942). In response to funding opportunity announcement RFA-FD-13-015, separate research projects were awarded in parallel to the University of Cincinnati and the University of Maryland, and each institution was requested by the FDA to perform independent research with the same drug products under comparable study conditions in a manner coordinated by the FDA. The views expressed in this paper do not reflect the official policies of the Department of Health and Human Services; nor does any mention of trade names, commercial practices, or organization imply endorsement by the United States Government.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. Steady-state temperature profile in the skin and subcutaneous tissues
Appendix. Steady-state temperature profile in the skin and subcutaneous tissues
Following the analysis of Wilson and Spence (49), steady-state temperatures in the tissue and TDS layers can be calculated by solving Eq. 6 and simplifications thereof with appropriate boundary conditions and blood flows in the various layers. The solution for the case in which the upper boundary of the SC (z = 0) is held at temperature T0 and the lower boundary of the muscle layer (z = z5) is assumed to be equal to the core temperature Tc is given below.
Stratum corneum (q = 0, ω = 0; i = 1):
Viable epidermis (ω = 0; i = 2):
Dermis, subcutaneous fat and muscle (i = 3, 4, 5):
There are 10 constants of integration, Ai, two for each layer. The boundary conditions at z = 0 and z = z5 give A1 = T0 and A9 = ϕ5 / \( {\gamma}_5^2 \). The other 8 constants are determined by the continuity conditions on temperature and heat flux at the four internal interfaces. The non-linear system of 8 equations and 8 unknowns can be solved by standard methods. We found that the Solver add-in to Microsoft Excel™, set to the GRG non-linear option, worked very well. Note that this method of solution differs from the sequential optimization routine described by Wilson and Spence (49).
Rights and permissions
About this article
Cite this article
LaCount, T.D., Zhang, Q., Hao, J. et al. Modeling Temperature-Dependent Dermal Absorption and Clearance for Transdermal and Topical Drug Applications. AAPS J 22, 70 (2020). https://doi.org/10.1208/s12248-020-00451-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-020-00451-2