Abstract
Background
Low awareness of chronic conditions raises the risk of poorer health outcomes and may result in healthcare utilization and spending in response to symptoms of undiagnosed conditions. Little evidence exists, particularly from lower-middle-income countries, on the health and healthcare use of undiagnosed people with an indication of a condition. This study aimed to compare health (physical, mental, and health-related quality of life (HRQoL)) and healthcare (inpatient and outpatient visits and out-of-pocket (OOP) medical spending) outcomes of undiagnosed Sri Lankans with an indication of coronary heart disease (CHD), hypertension, diabetes, and depression with the outcomes of their compatriots who were diagnosed or had no indication of these conditions.
Methods
This study used a nationally representative survey of Sri Lankan adults to identify people with an indication of CHD, hypertension, diabetes, or depression, and ascertain if they were diagnosed. Outcomes were self-reported measures of physical and mental functioning (12-Item Short Form Survey (SF-12)), HRQoL (EQ-5D-5L), inpatient and outpatient visits, and OOP spending. For each condition, we estimated the mean of each outcome for respondents with (a) no indication, (b) an indication without diagnosis, and (c) a diagnosis. We adjusted the group differences in these means for socio-demographic covariates using ordinary least squares (OLS) regression for physical and mental function, Tobit regression for HRQoL, and a generalized linear model (GLM) for healthcare visits and OOP spending.
Results
An indication of each of CHD and depression, which are typically symptomatic, was associated with a lower adjusted mean of physical (CHD -2.65, 95% CI -3.66, -1.63; depression -5.78, 95% CI -6.91, -4.64) and mental functioning (CHD -2.25, 95% CI -3.38, -1.12; depression -6.70, 95% CI -7.97, -5.43) and, for CHD, more annual outpatient visits (2.13, 95% CI 0.81, 3.44) compared with no indication of the respective condition. There were no such differences for indications of hypertension and diabetes, which are often asymptomatic.
Conclusions
Living with undiagnosed CHD and depression was associated with worse health and, for CHD, greater utilization of healthcare. Diagnosis and management of these symptomatic conditions can potentially improve health partly through substitution of effective healthcare for that which primarily responds to symptoms.
Similar content being viewed by others
Background
The burden of non-communicable diseases (NCDs) is large and growing in low- and middle-income countries (LMICs) [1]. In Sri Lanka, cardiovascular and metabolic diseases account for more than a quarter of the disease burden, compared to less than one-fifth in high-income countries [2].
A large proportion of people living with NCDs or their risk factors are undiagnosed [3,4,5,6]. In South Asia, around two-thirds of men with hypertension are undiagnosed, compared to 31% in high-income, Western countries [3]. Over half of diabetics in LMICs are undiagnosed [4]. In Sri Lanka, 47% and 38% of people with indications of hypertension and diabetes, respectively, are undiagnosed [7, 8]. There is also substantial underdiagnosis of CHD [9,10,11], and likely underdiagnosis of depression [12], a condition with a bidirectional relationship with CHD [13], diabetes [14], and their risk factors [15] in LMICs.
People in the early stages of developing a chronic condition are often asymptomatic, particularly for hypertension and diabetes. When symptoms do emerge, treatment may primarily respond to the symptoms without managing the underlying, still undiagnosed, condition [16,17,18,19,20,21]. If undiagnosed people with indications of chronic conditions experience worse health, make greater use of healthcare, and incur more OOP spending, then there may be potential for earlier diagnosis and management not only to slow or prevent disease onset but also to improve health immediately and reduce pressures on health systems and household finances.
There is little evidence from LMICs to determine whether people with an indication but not a diagnosis of a chronic health condition do experience worse health and make greater use of healthcare. An Indonesian study found that people with an indication of diabetes or hypertension that was undiagnosed did not have significantly higher healthcare utilization and expenditures, but undiagnosed people with an indication of a heart problem were more frequent users of outpatient care than people without these conditions [22]. In China, physical and mental functioning of people with an indication of hypertension without diagnosis were similar to those of people with no indication [23]. Even for high-income countries, there is limited evidence on health and healthcare utilization associated with having an indication of a chronic condition without a diagnosis. One small-scale study in Finland found that the physical functioning of people with an indication of hypertension without diagnosis was lower than that of people without hypertension [24]. A subnational study in Japan found that people with undiagnosed depression had lower physical and mental functioning, HRQoL, and more healthcare utilization than people without depression [25]. Each of these studies focused on a limited set of outcomes of one or two chronic conditions.
Using nationally representative data from Sri Lanka, this study aimed to add to the limited evidence from LMICs on the association between having an indication without diagnosis of each of four major chronic conditions—CHD, hypertension, diabetes, and depression—and both health (physical, mental, and HRQoL) and healthcare (inpatient and outpatient utilization, and OOP medical spending) outcomes.
Methods
We used data from the Sri Lanka Health and Ageing Study (SLHAS) conducted from 9 November 2018 to 14 November 2019 [26]. A multi-stage cluster random sampling design, stratified by district, residential sector, and area socioeconomic status (SES) was used to collect data in 297 sampling units selected by probability-proportionate-to-size sampling in all districts of Sri Lanka [27]. Within each sampling unit (smallest administrative division), households were randomly selected, and one adult (18 years and older) was randomly chosen from each household roster, with oversampling of those aged ≥ 70 years. After the application of sampling weights, the sample was representative of the adult population of Sri Lanka in 2019 by gender, age, geographical region, area SES, and ethnicity [27].
Data were collected using a computer-assisted personal interviewing platform, iFormBuilder (Zerion Software Inc., Herndon, VA, USA), with built-in skip logic and checks for unlikely values during data entry. During data cleaning, less likely values were cross-checked using manually recorded clinic checklists.
Identification of chronic conditions
In addition to completing a questionnaire, each respondent was asked to bring their medical records to the interview and to give consent for the enumerator to consult these records. An inventory of each respondent’s medicines was taken. Blood pressure, weight, and height were measured, and a blood sample was taken. Blood pressure was measured two times, 10 min apart, on one occasion using an OMRON HEM-7320 blood pressure monitor (OMRON Healthcare Co., Ltd., Kyoto, Japan) by a trained enumerator following standard procedure [7]. We used the mean of the two measurements. Participants were asked to fast for 12 h prior to attending the clinic for data collection. A venous blood sample was taken from all consenting participants, and those who provided an initial fasting sample underwent an oral glucose tolerance test [8]. Samples were stored within 6–10 h of initial collection in a field freezer (TwinBird Freezer SC-DF25, Twinbird Corporation, Niigata, Japan, and Glacio 55L Portable Cooler Fridge PFN-E-WEA-L-GR, New Aim Pty Ltd, Melbourne, Australia) at − 40 to − 20 °C for transport to the Sri Lanka Medical Research Institute (Colombo) for testing.
For each of four chronic conditions—CHD, hypertension, diabetes, and depression—we distinguished between respondents who (a) had been diagnosed (diagnosed), (b) showed an indication but had not been diagnosed (indicated), and (c) showed no indication and had not been diagnosed (no condition). A respondent was defined as diagnosed with CHD if they reported ever being diagnosed with angina, myocardial infarction or coronary artery disease, or their medical records indicated such a diagnosis. They were defined as indicated for CHD if they were not diagnosed but they satisfied the criteria on the Rose angina questionnaire of ever having chest pain that appeared upon exertion, was situated at any level of the sternum or left anterolateral chest and arm, which caused the respondent to slow down or stop while walking, and was relieved within ten minutes of rest, or they reported ever having severe chest pain across the front of the chest for thirty minutes or more [28, 29]. The Rose angina questionnaire is a standardized tool for detecting angina based on self-reported symptoms that has been used in a wide range of research and clinical settings [11, 28] and has been validated for use in Sri Lanka [30].
A respondent was categorized as diagnosed with hypertension if they reported a diagnosis or their medical records showed this, or they reported taking antihypertensives in the past 14 days. They were defined as indicated for hypertension if they were not diagnosed and had a systolic blood pressure of at least 140 mmHg or a diastolic blood pressure of at least 90 mmHg.
A respondent was identified as diagnosed with diabetes if they reported a diagnosis or their medical records showed this, or they reported taking oral hypoglycaemics or insulin in the past 14 days. They were defined as indicated for diabetes if they were not diagnosed but had a fasting plasma sugar of 126 mg/dL or more, or a random (6 participants had not fasted) or oral glucose tolerance test showed a plasma sugar of 200 mg/dL or more [8].
A respondent was categorized as diagnosed with depression if they reported a diagnosis or their medical records showed this. They were indicated for depression if it had not been diagnosed but they scored 10 or more on the Patient Health Questionnaire (PHQ-9) questionnaire [31]. A score ≥ 10 maximizes sensitivity and specificity for major depression [32] and is the threshold validated and used in Sri Lanka [31].
Outcomes
We used the physical component score (PCS) and mental component score (MCS) from the SF-12 questionnaire [33] to measure physical and mental health functioning, respectively. Both scores were calculated for each respondent using an algorithm developed from a sample in the USA, where scores were standardized to give a mean score of 50 and a standard deviation of 10 [33]. Scores below 50 indicate poorer function.
For each respondent, HRQoL was obtained from their responses to the EQ-5D-5L questionnaire [34]. The EQ-5D-5L is a multi-attribute utility instrument used to measure health status in five domains (mobility, self-care, usual activities, pain and discomfort, anxiety, and depression) with five levels of severity ranging from “no problems” to “extreme/unable”. Each combination of responses was mapped to a utility value using tariffs derived from Sri Lankan data [35], where 1 represents “perfect health” and 0 represents death, and where negative values (states worse than death) are possible.
We measured healthcare utilization with self-reported inpatient stays, which included any admission to a bed in a public or private hospital, and outpatient visits. Outpatient visits covered any visit to a facility that did not require admission or an overnight stay, and included public and private specialist and general clinics, allied health visits (e.g., to see a physiotherapist or dietician), public health clinics, such as medical officer of health and midwife clinics, visits to a pharmacy, laboratory or imaging center, and non-Western medicine clinics. The SLHAS randomly varied recall periods across participants in order to analyze the impact of recall periods on reported healthcare utilization in a study separate from this one. They were 1, 6, and 12 months (22%, 18%, and 60% of the sample) for inpatient visits and 7, 14, and 28 days (20%, 20%, and 60% of the sample) for outpatient visits. Data on the number of inpatient and outpatient encounters over a specified recall period were annualized.
Self-reported OOP spending for direct medical costs, including hospitalization and consultation fees, medicine and medical supplies, investigations, and informal payments were annualized. Amounts were converted to US dollars using the average US dollar exchange rate for the month the respondent was interviewed, as reported by the Central Bank of Sri Lanka, as an appropriate way to handle the devaluation of the local currency [36].
Covariates
Socio-demographic characteristics included age in 10-year age groups (18–29, 30–39, 40–49, 50–59, 60–69, 70–79, 80 +), sex (male, female), ethnicity (Sinhala, Tamil, Muslim/Moor/Malay, Other), education (no formal, primary, secondary, and tertiary), sector (urban, rural, estate, rural/estate) and province of residence, SES, household size (number of persons), and proportions of household members aged under 15 years and above 60 years. SES was proxied by quintile groups of an index obtained as the first principal component of an analysis of household assets, water and sanitation facilities, housing quality, and other assets [37] (Additional file 1: Supplementary methods). Standard body mass index (BMI) categories (normal < 25 kg/m2, overweight 25–29.9 kg/m2, obese ≥ 30 kg/m2), which were used in the sensitivity analysis, were calculated based on the weight in kilograms measured by an OMRON BF511 Body Composition Monitor (OMRON Healthcare Co., Ltd., Kyoto, Japan) and height measured in centimeters by a seca 240 mechanical measuring rod (stadiometer) (seca, Hamburg, Germany).
Statistical analysis
We estimated the mean of each outcome for each group defined as having no condition, being indicated, and being diagnosed for each of the four chronic conditions (CHD, hypertension, diabetes, and depression). We used a z-test to test the null of no difference in the means for indicated vs no condition, and diagnosed vs no condition. We used multivariate regression to estimate differences in the mean of each outcome between the three groups (no condition, indicated, and diagnosed) adjusted for the covariates (with age groups interacted with sex). For regressions of PCS and MCS scores, which are normally distributed, we used OLS. For HRQoL, following much analysis [38,39,40], we assumed a Tobit model to account for censoring at 1 that arose from anchoring EQ-5D-based utility values at that value for “full health”, and used maximum likelihood estimation. For regressions of inpatient and outpatient visits, which are counts data, and OOP spending, which are skewed data with many zero values, we used a GLM with a Poisson distribution, a log link, and robust standard errors. Correct specification of the conditional mean is sufficient for the consistency of this pseudo-maximum-likelihood estimator [41], which performs well with many zeros [40] and is often used to model medical spending data [41]. We present estimates from these models of average marginal effects (AME): the change in the mean of the outcome associated with a unit change in an independent variable that is estimated for each observation and averaged over the sample. We repeated the multivariate regressions extended to include BMI, which is usually positively associated with higher risk of CHD, hypertension, and diabetes [42, 43] but can also be associated with poorer health outcomes after controlling for these and other conditions [44]. In all analyses, we applied sample weights and estimated robust standard errors adjusted for sample stratification and clustering. A p-value less than 0.05 was considered statistically significant.
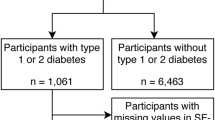
Data were missing for PCS, MCS and HRQoL (< 5%), inpatient and outpatient visits (< 3.5%), OOP spending (< 3%), and covariates (< 1%). To avoid selection bias that may result if participants with missing data were excluded, we assumed that data were missing at random and imputed them using multiple imputations with chained equations and predictive mean matching using 10 nearest neighbors (Additional file 1: Supplementary methods). As a sensitivity analysis, we also performed a complete case analysis instead of using multiply-imputed data. All analyses were performed using Stata 17.0 [45].
Results
Table 1 shows characteristics of the analysis sample after imputation. The mean age was 50.1 years (standard deviation (SD) 17.2) and 51% were female. A majority (82.1%) had secondary education or above. More than half (54.9%) of the sample were in the rural sector. The average household size was 2.98 (SD 1.4), with the proportion of household members aged above 60 years and below 15 years being 0.23 (SD 0.33) and 0.07 (SD 0.16), respectively, on average. Characteristics of the complete cases sample were very similar (Additional file 1: Table S1).
Table 2 shows, for each of the four chronic conditions, estimates of the population percentages with an indication but no diagnosis (indicated), a diagnosis (diagnosed), and with neither an indication nor diagnosis (no condition). We estimated that 5.7% (95% CI 5.0, 6.5) of the adult population of Sri Lanka had an indication of CHD but had not been diagnosed and 3.9% (95% CI 3.4, 4.4) had been diagnosed with CHD. Meanwhile, 13.0% (95% CI 11.8, 14.2) of the population had an indication of hypertension with no diagnosis, and 16.7% (95% CI 15.5, 17.8) had diagnosed hypertension. For diabetes, 7.2% (95% CI 6.4, 8.0) of the population had an indication of diabetes, and 13.6% (95% CI 12.3, 14.8) had a diagnosis. We estimated that 4.3% (95% CI 3.6%, 4.9%) of the population had an indication of depression and only 1.0% (0.7%, 1.3%) of the population had a diagnosis.
There was substantial multimorbidity (Additional file 1: Table S2). For example, we estimated that among those who had an indication or diagnosis of CHD, 52.0% (95% CI 47.0, 57.1) also had an indication or diagnosis of hypertension and 32.7% (95% CI 27.6, 37.7) had an indication or diagnosis of diabetes. Of those with an indication or diagnosis of depression, we estimated that 42.2% (95% CI 35.0, 49.4) had an indication/diagnosis of hypertension, 32.5% (95% CI 25.7, 39.4) had an indication/diagnosis of diabetes, and 22.3% (95% CI 16.6, 27.9) had an indication/diagnosis of CHD. There was also a substantial overlap between hypertension and diabetes.
Table 3 shows the estimated mean of each outcome by category of each chronic condition, and Fig. 1 shows the estimated adjusted difference in means between those indicated with each condition and those without that condition as well as the respective difference between those diagnosed with each condition and those without that condition (point estimates in Additional file 1: Table S3). Without and with adjustment, the mean PCS scores with an indication and with a diagnosis of CHD were lower—indicating lower physical functioning—than the mean score of those without any indication or diagnosis of CHD. After adjustment, the mean PCS score of those with an indication of CHD was 2.7 points (95% CI 1.6, 3.7) lower than the mean score of those without CHD. The mean difference between those diagnosed with CHD and those without the condition was the same (2.7, 95% CI 1.5, 3.8). Having an indication of CHD was associated with an adjusted mean MCS score that was 2.3 points (95% CI 1.1, 3.4) lower (worse mental functioning) than the respective score without CHD. Compared with not having CHD, a diagnosis of that condition was not associated with any difference in mental functioning even before adjusting for covariates. Point estimates show that respondents with an indication of CHD had lower mental functioning than those diagnosed with the condition, although the 95% CIs of the adjusted mean differences overlap. Compared with not having CHD, mean HRQoL was lower among those with an indication of CHD, and lower still for those with a diagnosis, with only the difference for those with a diagnosis statistically significant at the 0.05 level.
Compared with not having CHD, an indication of the condition and a diagnosis of it were each associated with more outpatient visits and higher OOP spending on healthcare, on average. Those diagnosed with CHD also had more inpatient admissions, on average. After adjustment, an indication of CHD was estimated to be associated with 2.1 (95% CI 0.8, 3.4) more outpatient visits per annum and $29.08 (95% CI − $1.49, $59.64) higher OOP spending per annum than the respective means for those without CHD. After adjustment, only mean inpatient admissions remained significantly higher for those with a CHD diagnosis than for those without the condition (0.18, 95% CI 0.03, 0.34), with no significant differences seen in outpatient visits and OOP spending.
An indication of hypertension and an indication of diabetes were both associated with lower mean PCS scores and HRQoL compared with not having the respective condition. After adjustment for covariates, these differences were not statistically significant, while diagnosed hypertension and diagnosed diabetes were associated with lower PCS scores (hypertension 3.15 95% CI 2.46, 3.84; diabetes 1.53 95% 0.86, 2.21) and HRQoL (hypertension 0.04 95% CI 0.03, 0.06; diabetes 0.02 95% CI, 0.01, 0.04), and with more outpatient visits (hypertension 2.63 95% CI 1.67, 3.60; diabetes 2.79 95% 1.75, 3.82) and OOP spending (hypertension $20.42 95% CI $8.59, $32.26; diabetes $25.10, 95% CI $11.15, $39.05), on average, compared with not having the respective conditions.
Mean PCS, MCS, and HRQoL scores were all significantly lower both for people with an indication of depression and for those diagnosed with depression than for those without depression. This was true without and with adjustment for covariates. Both unadjusted and adjusted estimates indicate that those with an indication of depression and those diagnosed with the condition had similar mean PCS and HRQoL scores. After adjustment, diagnosed depression was associated with a mean MCS score that was 12.58 points (95% CI 9.59, 15.58) lower than the mean for those with no depression, while those with an indication of depression also had a lower MCS score, though half as large in magnitude (6.70, 95% CI 5.43, 7.97).
Adding BMI as an additional covariate in the multivariate models had little impact on the magnitude and significance of the estimates of the partial associations of the outcomes with both an indication of each condition and its diagnosis (Additional file 1: Table S4). Complete case analysis yielded partial associations of similar direction, magnitude, and significance as those estimated using the multiply-imputed dataset (Additional file 1: Table S5).
Discussion
In LMICs, high prevalence of undiagnosed chronic conditions [3,4,5,6, 12], particularly cardiovascular disease risk factors, has rightly aroused concern about an iceberg of NCD that could strain health systems ill-prepared to respond to a double burden of disease [46]. These concerns motivate a push for earlier diagnosis of chronic conditions, which could well be a health system priority. Assessment of the likely consequences of such a policy requires better evidence on the health and healthcare utilization of people with an indication but not a diagnosis of chronic conditions. If they have poor health and make heavy use of healthcare, then diagnosis, and consequent treatment, may bring immediate improvement in health while straining a health system less than would be the case if the newly diagnosed were previously light users of healthcare.
This study of a representative sample of the adult population of Sri Lanka revealed heterogeneity by type of chronic condition in the health and healthcare utilization of those with an indication but not a diagnosis of a condition. We found that having an indication but not a diagnosis of either CHD or depression—both symptomatic conditions—was associated with worse physical and mental health functioning and, for depression, worse HRQoL, after adjustment for age, ethnicity, education, sector and province of residence, wealth quintile, household size and composition, and the other chronic conditions of interest. Point estimates suggest that indications of these two conditions may also be associated with greater utilization of healthcare and higher OOP medical spending, although most of these estimates do not reach conventional levels of statistical significance after adjustment. In contrast, having an indication but not a diagnosis of either hypertension or diabetes—two conditions that can remain asymptomatic for some time—was not partially associated with worse health functioning and HRQoL, nor with higher healthcare utilization and OOP spending, after adjustment. These findings suggest that the health, healthcare, and economic burdens of undiagnosed chronic conditions may well depend, as would be logical, on the degree to which any condition is symptomatic. Those suffering symptoms of an undiagnosed condition may seek relief through medical treatment. Asymptomatic conditions would not be expected to induce the same loss of health and level of healthcare seeking.
We found that for each of CHD and depression, the likelihood of being diagnosed was lower than the likelihood of having an undiagnosed indication, while the opposite was true for hypertension and diabetes. This discrepancy may be partly due to the relatively higher cost and complexity of diagnosing the first two conditions. Health system constraints may slow the diagnosis of CHD and depression, which may partly explain the lower functioning and HRQoL of people with undiagnosed indications of these conditions. Less technology and skills are required to diagnose hypertension and diabetes, which may contribute to quicker diagnosis and less health impact among those not yet diagnosed.
We found that people with an indication of CHD had similar limitations in physical functioning and more limitations in mental functioning than people diagnosed with CHD, after adjustment. We estimated that an indication of CHD was associated with lower physical and mental functioning equal in magnitude to about 4–5% in the respective score. An indication of CHD was estimated to be associated with at least two outpatient visits per year more than the average with no indication of CHD after adjustment—a 46% increase. The absolute increase in the number of outpatient visits was similar to that associated with being diagnosed with CHD without adjustment. This is similar to findings in Indonesia, where people with undiagnosed “heart problems” had an additional 1.9 outpatient visits per year than those who did not have heart problems [22]. After adjusting for covariates, we found that OOP spending of those with an indication of CHD was almost 85% higher than those with no indication of CHD, on average. As a result of these increases, the utilization of outpatient care and the OOP spending of people with an indication of CHD were similar to the average levels of those with diagnosed CHD, hypertension, and diabetes. In Indonesia, people with undiagnosed heart problems did report higher outpatient and inpatient medical expenses, though this was not statistically significant, but they also reported higher expenditures on self-treatment [22]. The findings in Sri Lanka suggest that targeting people with an indication of CHD but not yet diagnosed should be prioritized given health and healthcare outcomes that are on par with people already diagnosed with CHD risk factors. For hypertension and diabetes, screening to identify people with indications of these conditions can still be worthwhile to reverse or slow progression to worse outcomes observed among those who are eventually diagnosed [47].
After adjusting for covariates, we found that the lower levels of physical functioning and HRQoL associated with an indication of depression were as large as the respective reductions associated with diagnosed depression. As would be expected, an indication of depression was associated with a reduction in mental functioning that was a little more than half the magnitude of the reduction associated with diagnosed depression. However, on average, those with an indication of depression scored 13% lower in mental functioning than those with no indication of depression after full adjustment. These findings suggest that people with symptoms of depression experience substantial losses of health and related quality of life that, with the exception of mental functioning, were similar to those experienced by those diagnosed with depression. There were similarities with findings in Japan, where people with undiagnosed depression had lower physical and mental functioning than those without depression, and similar to those with diagnosed depression [25]. The fact that reductions in health and quality of life associated with an indication of depression were substantially larger than those estimated for an indication of CHD gives further reason to increase efforts to identify Sri Lankans living with undiagnosed depression.
We found that indications of hypertension and diabetes were not associated with worse health and greater healthcare utilization, while these outcomes were associated with diagnosed hypertension and diabetes. These findings are consistent with evidence from Indonesia showing that outpatient use and OOP spending were higher for people with self-reported hypertension and diabetes, but these outcomes were not higher for people with undiagnosed hypertension and diabetes [22]. Our estimates are also consistent with other evidence that people with undiagnosed hypertension report better physical health than people diagnosed with the condition [24, 48]. There are several potential explanations for these consistencies. First, people who are undiagnosed may have had the condition for a shorter period and are less likely to be symptomatic, and so may not have experienced a loss of health which would also cause their demand for healthcare to increase [22]. Second, the association of diagnosed diabetes and hypertension with more outpatient visits and OOP spending is expected as these people should have had regular follow-up visits to manage their condition, while people with indications of diabetes and hypertension may not have sought additional healthcare as they had no perceived requirement. Lastly, among those with indications of hypertension and diabetes based on measurements taken in a single encounter, there are likely to be many false positives [22]. As with awareness–treatment–control studies of hypertension and diabetes, there is a risk of misclassifying individuals without these conditions as having an indication of them. This would dilute associations between true indications of hypertension or diabetes and health and healthcare outcomes.
There were several limitations in our study. Due to the nature of the field survey, we were limited to one measurement of biomarkers. The biomarkers used to define diabetes in this study were likely to be more precise than the symptomatic criteria used in a related study [22]. Furthermore, single biomarker measurements for hypertension and diabetes are commonly used in cascades of care studies to assess the performance of healthcare systems [4, 49].
To identify undiagnosed heart problems [22] and depression [25], we used methods that are commonly used to estimate the prevalence of these conditions. While an indication of a chronic condition is often used to identify undiagnosed cases [22, 24, 25], there is variation in the positive predictive values of the indicator tools. Nevertheless, our study suggests, at the very least, that people with symptoms that are indicative of CHD and depression were likely to experience poorer health and healthcare outcomes than those without indications of these conditions. We did not assess whether the duration since diagnosis was associated with worse outcomes.
The algorithm used to calculate physical and mental health functioning scores has been validated in several other countries [50] but not in Sri Lanka. For comparisons within a country, it is expected that the US-based algorithm will provide similar results to a country-derived one [51], although we cannot be sure of this.
Conclusions
Undiagnosed people with indications of symptomatic conditions like CHD and depression are likely to have poorer health and use more healthcare than people without these conditions. Outcomes can even be worse for the undiagnosed than for the diagnosed. This suggests that management of people with indications of CHD and depression should be prioritized as the burden of these undiagnosed conditions was almost as high as it was for those diagnosed with these conditions. Getting these people diagnosed and onto effective disease management programmes that pay attention to follow-up and treatment compliance may not raise demands on health systems by so much since the undiagnosed are already heavy users of healthcare. In contrast, people with indications of typically asymptomatic conditions like hypertension and diabetes, show similar outcomes to those without these conditions. Here, diagnosis and effective management and control could still generate important health benefits by slowing disease progression.
Availability of data and materials
The data that support the findings of this study are available from the SLHAS Consortium but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. The SLHAS Consortium, which has adopted an open data policy, will provide access to SLHAS Wave 1 data from 2024, on application to the Consortium by interested researchers. The specific data file used for this paper can be obtained from Nilmini Wijemunige upon reasonable request (nilmini@ihp.lk), and with permission of the SLHAS Consortium.
Abbreviations
- AME:
-
Average marginal effects
- BMI:
-
Body mass index
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- GLM:
-
Generalized linear model
- HRQoL:
-
Health-related quality of life
- LMICs:
-
Low- and middle-income countries
- MCS:
-
Mental component summary
- NCD:
-
Non-communicable diseases
- OLS:
-
Ordinary least squares
- OOP:
-
Out-of-pocket
- PCS:
-
Physical component summary
- PHQ:
-
Patient Health Questionnaire
- SD:
-
Standard deviation
- SES:
-
Socioeconomic status
- SF-12:
-
12-Item Short Form Survey
- SLHAS:
-
Sri Lanka Health and Ageing Study
References
Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22. https://doi.org/10.1016/S0140-6736(20)30925-9.
Institute for Health Metrics and Evaluation. GBD Compare | IHME Viz Hub. Available from: https://vizhub.healthdata.org/gbd-compare/.
Collaboration NCDRF. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–80. https://doi.org/10.1016/S0140-6736(21)01330-1.
Manne-Goehler J, Geldsetzer P, Agoudavi K, Andall-Brereton G, Aryal KK, Bicaba BW, et al. Health system performance for people with diabetes in 28 low- and middle-income countries: a cross-sectional study of nationally representative surveys. PLoS Med. 2019;16(3):e1002751. https://doi.org/10.1371/journal.pmed.1002751.
Brewer LC, Svatikova A, Mulvagh SL. The challenges of prevention, diagnosis and treatment of ischemic heart disease in women. Cardiovasc Drugs Ther. 2015;29(4):355–68. https://doi.org/10.1007/s10557-015-6607-4.
Zuchi C, Tritto I, Ambrosio G. Angina pectoris in women: focus on microvascular disease. Int J Cardiol. 2013;163(2):132–40. https://doi.org/10.1016/j.ijcard.2012.07.001.
Rannan-Eliya RP, Wijemunige N, Perera P, Kapuge Y, Gunawardana N, Sigera C, et al. Prevalence and associations of hypertension in Sri Lankan Adults: estimates from the SLHAS 2018–19 survey using JNC7 and ACC/AHA 2017 guidelines. Glob Heart. 2022;17(1):50. https://doi.org/10.5334/gh.1135.
Rannan-Eliya RP, Wijemunige N, Perera P, Kapuge Y, Gunawardana N, Sigera C, et al. Prevalence of diabetes and pre-diabetes in Sri Lanka: a new global hotspot-estimates from the Sri Lanka Health and Ageing Survey 2018/2019. BMJ Open Diabetes Res Care. 2023;11(1). https://doi.org/10.1136/bmjdrc-2022-003160
Bodegard J, Erikssen G, Bjornholt JV, Thelle D, Erikssen J. Possible angina detected by the WHO angina questionnaire in apparently healthy men with a normal exercise ECG: coronary heart disease or not? A 26 year follow up study. Heart. 2004;90(6):627–32. https://doi.org/10.1136/hrt.2003.012542.
Graff-Iversen S, Selmer R, Lochen ML. Rose angina predicts 23-year coronary heart disease mortality in women and men aged 40–49 years. Heart. 2008;94(4):482–6. https://doi.org/10.1136/hrt.2007.115931.
Hemingway H, Langenberg C, Damant J, Frost C, Pyorala K, Barrett-Connor E. Prevalence of angina in women versus men: a systematic review and meta-analysis of international variations across 31 countries. Circulation. 2008;117(12):1526–36. https://doi.org/10.1161/CIRCULATIONAHA.107.720953.
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8(1):2861. https://doi.org/10.1038/s41598-018-21243-x.
Wium-Andersen MK, Wium-Andersen IK, Prescott EIB, Overvad K, Jorgensen MB, Osler M. An attempt to explain the bidirectional association between ischaemic heart disease, stroke and depression: a cohort and meta-analytic approach. Br J Psychiatry. 2020;217(2):434–41. https://doi.org/10.1192/bjp.2019.130.
Alexandre K, Desrichard O, Burnand B, Peytremann-Bridevaux I. Factors influencing self-management in adults with diabetes: an umbrella review protocol. JBI Database System Rev Implement Rep. 2017;15(11):2630–7. https://doi.org/10.11124/JBISRIR-2016-003318.
Neupane D, Panthi B, McLachlan CS, Mishra SR, Kohrt BA, Kallestrup P. Prevalence of undiagnosed depression among persons with hypertension and associated risk factors: a cross-sectional study in urban Nepal. PLoS ONE. 2015;10(2):e0117329. https://doi.org/10.1371/journal.pone.0117329.
Chu RY, Dong D, Wong SY, Lee EK. Barriers and determinants to the underutilized hypertension screening in primary care patients in Hong Kong: a mixed-method study. Int J Environ Res Public Health. 2023;20(2):985. https://doi.org/10.3390/ijerph20020985.
Soliman SSA, Guseman EH, Haile ZT, Ice G. Prevalence and determinants of hypertension unawareness among Egyptian adults: the 2015 EHIS. J Hum Hypertens. 2021;35(10):927–34. https://doi.org/10.1038/s41371-020-00431-1.
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–68. https://doi.org/10.1001/jama.2013.184182.
Green CA, Johnson KM, Yarborough BJ. Seeking, delaying, and avoiding routine health care services: patient perspectives. Am J Health Promot. 2014;28(5):286–93. https://doi.org/10.4278/ajhp.120702-QUAL-318.
Taber JM, Leyva B, Persoskie A. Why do people avoid medical care? A qualitative study using national data. J Gen Intern Med. 2015;30(3):290–7. https://doi.org/10.1007/s11606-014-3089-1.
Teo CH, Ng CJ, Booth A, White A. Barriers and facilitators to health screening in men: a systematic review. Soc Sci Med. 2016;165:168–76. https://doi.org/10.1016/j.socscimed.2016.07.023.
Finkelstein EA, Chay J, Bajpai S. The economic burden of self-reported and undiagnosed cardiovascular diseases and diabetes on Indonesian households. PLoS ONE. 2014;9(6):e99572. https://doi.org/10.1371/journal.pone.0099572.
Mi B, Dang S, Li Q, Zhao Y, Yang R, Wang D, et al. Association between awareness of hypertension and health-related quality of life in a cross-sectional population-based study in rural area of northwest China. Medicine (Baltimore). 2015;94(29):e1206. https://doi.org/10.1097/MD.0000000000001206.
Korhonen PE, Kivela SL, Kautiainen H, Jarvenpaa S, Kantola I. Health-related quality of life and awareness of hypertension. J Hypertens. 2011;29(11):2070–4. https://doi.org/10.1097/HJH.0b013e32834bbca7.
Yamabe K, Liebert R, Flores N, Pashos CL. Health-related quality of life outcomes, economic burden, and associated costs among diagnosed and undiagnosed depression patients in Japan. Clinicoecon Outcomes Res. 2019;11:233–43. https://doi.org/10.2147/CEOR.S179901.
Rannan-Eliya RP, Dissanayake V, Perera P, Herath H, Perera B, Wijemunige N, et al. Sri Lanka Health and Ageing Study, Wave 1 Data. 2019.
Rannan-Eliya RP, Dissanayake VH, Perera P, Perera B, Herath HMM, Wijemunige N, et al. Cohort profile: the Sri Lanka Health and Ageing Study (SLHAS). Int J Epidemiol. 2024;53(2). https://doi.org/10.1093/ije/dyae044
Rose G, McCartney P, Reid DD. Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med. 1977;31(1):42–8. https://doi.org/10.1136/jech.31.1.42.
Lawlor DA, Adamson J, Ebrahim S. Performance of the WHO Rose angina questionnaire in post-menopausal women: are all of the questions necessary? J Epidemiol Community Health. 2003;57(7):538–41. https://doi.org/10.1136/jech.57.7.538.
Mendis S, Ekanayake EM. Prevalence of coronary heart disease and cardiovascular risk factors in middle aged males in a defined population in central Sri Lanka. Int J Cardiol. 1994;46(2):135–42. https://doi.org/10.1016/0167-5273(94)90034-5.
Hanwella R, Ekanayake S, de Silva VA. The validity and reliability of the Sinhala translation of the Patient Health Questionnaire (PHQ-9) and PHQ-2 Screener. Depress Res Treat. 2014;2014:768978. https://doi.org/10.1155/2014/768978.
Spitzer R, Williams J, Kroenke K, Colleagues. Test review: Patient Health Questionnaire–9 (PHQ-9). Rehabilitation Counseling Bulletin. 2014;57(4):246–8. https://doi.org/10.1177/0034355213515305.
Ware JE, Kosinski M, Keller SD. How to score the SF-12 Physical and Mental Health Summary Scales (2nd Edition). Boston: The Health Institute, New England Medical Center; 1995.
EuroQOL Research Foundation. EQ-5D-5L User Guide, 20192021.
Kularatna S, Whitty JA, Johnson NW, Jayasinghe R, Scuffham PA. Valuing EQ-5D health states for Sri Lanka. Qual Life Res. 2015;24(7):1785–93. https://doi.org/10.1007/s11136-014-0906-2.
Turner HC, Lauer JA, Tran BX, Teerawattananon Y, Jit M. Adjusting for inflation and currency changes within health economic studies. Value Health. 2019;22(9):1026–32. https://doi.org/10.1016/j.jval.2019.03.021.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32. https://doi.org/10.1353/dem.2001.0003.
Sullivan PW. Are utilities bounded at 1.0? Implications for statistical analysis and scale development. Med Decis Making. 2011;31(6):787–9. https://doi.org/10.1177/0272989X11400755.
Sullivan T, Turner RM, Derrett S, Hansen P. New Zealand population norms for the EQ-5D-5L constructed from the personal value sets of participants in a national survey. Value Health. 2021;24(9):1308–18. https://doi.org/10.1016/j.jval.2021.04.1280.
Shiroiwa T, Noto S, Fukuda T. Japanese population norms of EQ-5D-5L and Health Utilities Index Mark 3: disutility catalog by disease and symptom in community settings. Value Health. 2021;24(8):1193–202. https://doi.org/10.1016/j.jval.2021.03.010.
Gourieroux C, Monfort A, Trognon A. Pseudo maximum likelihood methods: applications to Poisson models. Econometrica: J Econ Soc. 1984;52(3):701–20.
Scherer PE, Hill JA. Obesity, diabetes, and cardiovascular diseases: a compendium. Circ Res. 2016;118(11):1703–5. https://doi.org/10.1161/CIRCRESAHA.116.308999.
Iliodromiti S, Celis-Morales CA, Lyall DM, Anderson J, Gray SR, Mackay DF, et al. The impact of confounding on the associations of different adiposity measures with the incidence of cardiovascular disease: a cohort study of 296 535 adults of white European descent. Eur Heart J. 2018;39(17):1514–20. https://doi.org/10.1093/eurheartj/ehy057.
Katz DA, McHorney CA, Atkinson RL. Impact of obesity on health-related quality of life in patients with chronic illness. J Gen Intern Med. 2000;15(11):789–96. https://doi.org/10.1046/j.1525-1497.2000.90906.x.
StataCorp. Stata Statistical Software: Release 17. College Station: StataCorp LLC; 2021.
Collaborators GBDV. Five insights from the global burden of disease study 2019. Lancet. 2020;396(10258):1135–59. https://doi.org/10.1016/S0140-6736(20)31404-5.
Zygmuntowicz M, Owczarek A, Elibol A, Chudek J. Comorbidities and the quality of life in hypertensive patients. Pol Arch Med Wewn. 2012;122(7–8):333–40.
Mena-Martin FJ, Martin-Escudero JC, Simal-Blanco F, Carretero-Ares JL, Arzua-Mouronte D, Herreros-Fernandez V. Health-related quality of life of subjects with known and unknown hypertension: results from the population-based Hortega study. J Hypertens. 2003;21(7):1283–9. https://doi.org/10.1097/00004872-200307000-00015.
Geldsetzer P, Manne-Goehler J, Marcus ME, Ebert C, Zhumadilov Z, Wesseh CS, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1.1 million adults. Lancet. 2019;394(10199):652–62. https://doi.org/10.1016/S0140-6736(19)30955-9.
Ware JE Jr, Gandek B, Kosinski M, Aaronson NK, Apolone G, Brazier J, et al. The equivalence of SF-36 summary health scores estimated using standard and country-specific algorithms in 10 countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1167–70. https://doi.org/10.1016/s0895-4356(98)00108-5.
Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1171–8. https://doi.org/10.1016/s0895-4356(98)00109-7.
Acknowledgements
The authors thank their colleagues in the Sri Lanka Health and Ageing Study consortium, consisting of the Institute for Health Policy, University of Colombo, University of Ruhuna, and University of Peradeniya, for their input into the design of the survey tools and support of data collection, in particular Dr Renuka Jayatissa (Medical Research Institute) whose staff supported the laboratory analyses; and colleagues in the Ministry of Health, who facilitated the SLHAS, in particular, Dr Sridharan (Deputy Director General (Planning), Ministry of Health), and Dr Anuji Gamage (Kotelawala Defence University). The authors also thank colleagues who were instrumental in the management of fieldwork, in particular Ms. Ruwanthi Elwalagedara and Dr. Prasadini Perera.
Funding
The data collection underlying this research, and analysis, was supported by the Swiss Agency for Development Cooperation (SDC) and the Swiss National Science Foundation (SNSF) through the Swiss Programme for Research on Global Issues for Development (r4d programme) by the grant “Inclusive social protection for chronic health problems” (Grant number 400640_160374), and the Institute for Health Policy Public Interest Research Fund (Grant number PIRF-2018–02).
Author information
Authors and Affiliations
Contributions
NW, RRE, and OOD conceived and designed the study. NW and RRE carried out data collection. NW carried out the analysis and NW, PVB, and OOD carried out the interpretation of data. NW wrote the first draft. OOD and PVB provided input for critical revisions. All authors contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for Sri Lanka Health and Ageing Study data collection and analysis was obtained from the Sri Lanka Medical Association (ERC/18–022). Informed written consent was obtained from all individual participants included in the study. The analysis for this paper was done on deidentified data which cannot be linked back to individuals. Data collection and analysis was carried out in accordance with relevant guidelines and regulations in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary methods (Estimation of household SES using principal components analysis; Multiple imputation method) and Supplementary results (Complete case and imputed sample characteristics; Contingency table showing percentage of people with comorbid conditions; Adjusted differences in mean health and healthcare outcomes; AME controlling for BMI; and AME using complete case analysis).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wijemunige, N., van Baal, P., Rannan-Eliya, R.P. et al. Health outcomes and healthcare utilization associated with four undiagnosed chronic conditions: evidence from nationally representative survey data in Sri Lanka. BMC Global Public Health 2, 45 (2024). https://doi.org/10.1186/s44263-024-00075-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44263-024-00075-0