Abstract
Background
The high readmission rate following chronic obstructive pulmonary disease (COPD) has created a significant global health challenge, with high healthcare costs and a growing burden of care. Digital interventions, including telemonitoring, Telehealth, web, or mobile-based, can address these challenges, but there has yet to be a systematic review of the impact of digital interventions on reducing hospital readmission for patients with COPD. The aim of this systematic review was to assess the effectiveness of digital interventions in lowering hospitalization and rehospitalization for patients with COPD.
Methods
We conducted a systematic literature search from PubMed and Scopus to identify randomized controlled trials (RCTs) published in English with outcomes related to hospital admission or readmission within 30 days of hospital discharge.
Results
The search and selection process followed PRISMA guidelines and resulted in a final sample of 12 RCTs. We found mixed results. Of the 12 included studies, only four studies [mobile-based (n=1), Telehealth (n=1), Telemonitoring (n=2)] found positive effect of a digital intervention on hospital readmission. Seven studies [mobile-based (n=1), Telehealth (n=1), Telemonitoring (n=3), Web-based (n=2)] did not demonstrate clear evidence of a significant reduction in hospitalization rate. Based on these findings, the primary factors contributing to the outcome variation were differences in intervention components used and their operator, COPD severity, patient age, and sample size.
Conclusions
Systematic review provides the first insight into the impact of digital intervention on hospital readmission among patients with COPD . While some studies showed positive results, the evidence is mixed, and further research is needed. COVID-19 has accelerated the use of digital intervention and created the opportunity for comprehensive research and investigation with more updated information and further impact on readmission.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Chronic obstructive pulmonary disease (COPD) is a chronic lung disease that results in restricted airflow and breathing problems caused by smoking, active or passive tobacco exposure, occupational exposure to biomass fuel, and air pollution as a significant contributor. (World Health Organization 2023) COPD is one of the third leading causes of death worldwide [1], and the USA spends $9,800 per COPD patient every year. [2] The World Health Organization predicts that by 2030, COPD will become the top cause of death worldwide. [3] One of the reasons that the economic burden of COPD is so high relates to 30-day readmission. Globally, 22.6 % of patients with COPD get hospitalized within 30 days of discharge. However, 90-day readmission rates are as high as 43% [2] COPD. The average cost of readmission for COPD patient is 118% of the initial hospitalization, which average $7,100 (Elixhauser et al., 2011) [4]. The direct COPD patient care cost is almost $50 billion annually in the USA, and out of this, over $ 15 billion is spent due to hospital readmission (Press et al., 2018) [5].
Hospital readmission rate within 30 days of discharge is the benchmark of quality of healthcare services, and readmission has also increased the overall healthcare cost. It is thus critical to explore efficient methods of healthcare delivery as patients age and live longer with the disease. [6]. Digital intervention in the form of telehealth, telemonitoring, web, and mobile-based have the potential to manage better and improve the patient’s health. This may involve using mobile phones, tablets, Telemonitoring equipment with gateway devices for data transmission, and individualized training.
It has been suggested that healthcare delivery for patients with COPD will be better managed and efficient by introducing some form of digital intervention. [7, 8]. Digital intervention can connect patients directly with providers to better manage healthcare services for improved outcomes [9] This study found that the mobile health apps had demonstrated potential to improve patients’ self-management behavior, oxygen saturation level monitoring, adherence to medication, and overall mood. In turn, these may improve patients’ overall self-management and as a result, in theory, could potentially reduce avoidable hospitalization and readmissions.
An editorial review by Seemungal et al. (2009) [10] found that self-management can reduce COPD hospital readmission by 40%, and digital intervention can play a critical role in efficiently managing patients with COPD using electronic devices. McLean et al. (2011) found positive results of telehealth intervention for patients with COPD rehospitalization. Published research concluded that telehealthcare, which includes real-time interactions with healthcare professionals using internet-based video communication, reduced emergency department visits and hospital admissions to improve the overall quality of life of patients with COPD than usual care. However, further research was needed to precisely clarify the impact of intervention as telehealth was included as part of a more complex package.
Williams et al. (2014) found digital intervention have potential to connect with healthcare providers earlier in process to prevent progression of pulmonary diseases and a significant improvement in hospitalized or re hospitalized patients with COPD. However, they could only partially confirm that specific patterns of digital intervention will always have positive outcomes due to limited evidence. The use of digital intervention and technological advancement in mobile, web, and telemonitoring has improved drastically during the COVID-19 pandemic.
Despite a series of studies which indicate that digital interventions have promise for improving patient self-management, to our knowledge there have yet to be recent systematic reviews which evaluate whether this translates into actual reductions hospitalizations or hospital readmissions for COPD. Further, the most recent systematic reviews were from prior to the COVID-19 pandemic, after which a significant advance occurred in the development and uptake of digital technologies for health. Two prior systematic reviews from (Janjua et al., 2021) [3], (Janjua et al., 2018) [11] and (McCabe et al., 2017) [12] evaluated the effectiveness of digital intervention on overall management and treatment effectiveness for patients with COPD . They found remote monitoring interventions were among the most favorable interventions. Here, we aim to plug these gaps by performing a systematic review of the effectiveness of digital interventions in lowering hospitalization and rehospitalization for patients with COPD.
Methods
We performed a systematic review following PRISMA (Preferred Reporting items for Systematic Review and Meta-Analyses) guidelines and registered the study with the protocol published in PROSPERO CRD42023445702.)
Search strategy and study selection
We searched PubMed and Scopus databases on May 23, 2023, for peer-reviewed articles focusing on 1) digital interventions and 2) avoidable hospitalization. We operationalized different combinations of each keyword based on previously validated searches for both “avoidable hospitalization” [13,14,15] and “Digital Interventions” [16, 17]. We applied the fields in the title /abstract in the search of PubMed and Scopus databases. Full details of the search terms and corresponding PICO model are available in Supplementary material S1_Search strategies.
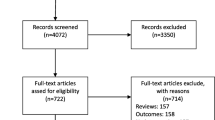
Figure 1 details the PRISMA flow diagram of literature search and selection criteria. 951 articles were retrieved through electronic database, including 376 from PubMed and 575 articles from Scopus. These articles were then imported to Zotero, which identified 167 as duplicates, leaving 784 for screening and eligibility stages.
Inclusion/exclusion criteria
We defined our inclusion/exclusion criteria using the PICOS framework (see Table 1 below)
Articles were included if they were: 1) published in Peer reviewed journals 2) written in the English language 3) randomized controlled trials only; 4) outcomes including Hospital admission /readmission within 30-day of initial discharge. Hence, we excluded conference papers, books, editorials, reviews, and surveys as well as pilot studies and RCT protocols.
We further screened the remaining 784 articles based on title and articles, identifying 51 which were not relevant articles were initially analyzed using title and abstract to exclude additional 51 articles which includes 46 irrelevant (not related to digital intervention), four additional duplicates and one unpublished article. Subsequently
Based on full text screening total of 619 articles were excluded which includes non RCT (n=213), reviews and analyses (n=188), pilot studies (n=105) and out of scope study categories (n=56) as the major contributor.
Finally, 12 RCTs (randomized control trial) were included part of this review focusing on COPD (chronic obstructive pulmonary disease) patients’ part of final sample.
Data extraction and data synthesis
V.M. and D.S. designed the framework and topic. Three review authors (V.M., D.S., and CM) finalized the search strategy and screening criteria to flag the articles as eligible, potentially eligible, or unclear. V.M. retrieved full-text study reports of all potentially eligible studies, which are further reviewed by D.S. and C.M. for inclusion, listing reasons for exclusions on ineligible studies and all disagreements resolved through multiple discussions. V.M. and D.S. worked together on the data extraction strategy. V.M. extracted the outcome data from a mutually agreed strategy among three review authors (V.M., D.S., and CM). D.S. and C.M. have further reviewed extracted data independently to check the consistency of the result.
We used Microsoft excel to create a summary table extracting study characteristics, interventions, and outcome. From included studies, we extracted data for Published Year, Author, Article Title, Objective, Geography/country, Intervention, Intervention Grouping, Study population, Randomization method, results, and conclusions. Because of heterogeneity across studies, results were summarized narratively, and results organized by type of digital intervention.
In terms of data synthesis, we undertook a narrative review because the studies were too heterogeneous for meta-analysis. Specifically, we synthesized results by identifying four broad types of intervention (‘Web-based,’ ‘Mobile,’ ‘Telehealth, ‘And Telemonitoring’) and then grouped the included study into one of these categories. Finally, the categorized study is reviewed thoroughly to find the detailed results, which are subclassified as ‘positive results’, “No significant difference in rehospitalization rate,” and “No evidence of non-inferiority,” respectively.
Results
Our final analysis included 12 RCTs (randomized control trials). Of these, four were conducted in Denmark and 2 in the US. Italy, Scotland (UK), Norway, Spain, Sweden, and Taiwan each had 1 RCT in the sample. Finally, one multi-country study covered Australia and Denmark.
These trial study populations ranged from 57 (Jakobsen et al., 2015) [18] to 511 patients (Ritchie et al., 2016) [19], with durations ranging between a couple of weeks to a 2-year time frame.
Studies fell into the below-mentioned categories of digital interventions (Table 1): ‘Web-based’(n=2), ‘Mobile based’ (n=2), ‘Telehealth’(n=3), and ‘Telemonitoring’ (n=5). Table 2 describes the main study characteristics and findings.
Classification of intervention
Overall, the results were mixed. Most studies (n= 7) failed to identify a significant improvement in hospital readmission attributable to digital interventions, as shown in Table 3 below.
In the remaining sections, we discuss study findings with respect to intervention type (Table 4).
Web- and mobile-based interventions (n=4)
Of the four studies that examined a web or mobile-based intervention, only 1 study found positive results. However, 3 out of 4 found significantly positive effects in reducing hospital readmission or dimensions of self-management of COPD, such as adherence to medicine.
Turning to the main positive findings, the RCT by Piette et al. (2019) [21] aimed to assess the effects of an accessible health technology and caregiver support program on 30-day readmission risk in patients with common medical diagnoses, including COPD, coronary artery disease, pneumonia, and diabetes in the USA. While the intervention did not show a significant difference in the 30-day readmission rate for all patients, among patients with pulmonary diagnoses, the intervention group demonstrated a significantly reduced 30-day risk of rehospitalization relative to controls (HR: 0.31; 0.11, 0.87; p=.026).
No significant difference in hospitalization rate was found for the remaining three studies examining a web or mobile-based intervention. These studies, undertaken in Sweden, Spain, and the US, examined. While Ritchie et al. (2016) [19] have reduced the number of days in hospital for patients with COPD , none were found to affect 30-day readmissions. (0.5 vs. 1.6, p = 0.03)
Ritchie et al. (2016) [21] trial randomized 511 patients hospitalized with congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) in the USA to an E-Coach technology-assisted care transition system. The E-Coach intervention integrates a remote monitoring device with IVR (interactive voice response), which takes the patient’s vital signs input (Oxygen saturation, heart rate, and repository rate) using the touchpad daily. This information gets pulled on the web-based dashboard for detailed monitoring of a patient daily. E-coach did not significantly affect 30-day rehospitalization rates (0.5 vs. 1.6, p = 0.03).
Garcia-Aymerich et al. 2007 [29] evaluated the effects of integrated care intervention on risk factors for COPD readmissions in Spain, having 113 exacerbated patients (14% female, mean (SD)age 73 [17]). This study used an individually tailored care plan post-discharge shared with the primary care team and access to a specialized case manager nurse through a web-based call center as the intervention. The integrated care intervention improved patient knowledge, adherence to treatment, and self-management items related to COPD. However, no differences were observed in lung function, quality of life scores, lifestyle factors, medical treatment, or risk of hospital readmission between the intervention and control groups.
Fors et al. 2018 [20] trial evaluated the effects of person-centered telephone support in patients with COPD and/or chronic heart failure in Sweden. This trial randomized 221 patients with a mean age of 77.6 years, and 54.3% were women. All the patients in the intervention group received a telephone call one to four weeks after discharge in addition to usual care. The results did not show a significant difference in a composite score comprising general self-efficacy, rehospitalization, and death between the intervention and control groups at six months of follow-up. However, the intervention did reduce the risk of decreased self-efficacy in patients.
Impact of telehealth/telemonitoring (n= 8)
Of the eight studies examining telehealth and telemonitoring intervention, only three found positive results in hospital readmission related to COPD exacerbations.
Of these three studies, most found positive results and examined various telemonitoring devices, including pulse oximeters, thermometers, and electronic diaries, to continuously monitor patients’ symptoms and vital signs. Patients in these studies were trained to report their symptoms and health data regularly, either daily or periodically, and patients were allowed to communicate with trained operation or medical nurses at specific hours.
Specifically, Zanaboni et al. (2023) [23] randomized controlled trial compared long-term telerehabilitation or unsupervised training at home with standard care in patients with COPD from Norway, Australia, and Denmark. Both telerehabilitation and unsupervised training groups experienced significantly fewer acute exacerbations of COPD hospitalizations during the intervention period than the control group. Additionally, participants in the intervention groups showed better health status for one year. Long-term telerehabilitation and unsupervised training were favorable alternate COPD patient maintenance and rehospitalization.
The incidence rate of hospitalizations and emergency department presentations was lower in telerehabilitation (1.18 events per person-year; 95% confidence interval [CI], 0.94-1.46) and unsupervised training group (1.14; 95% CI, 0.92-1.41) than in the control group (1.88; 95% CI, 1.58-2.21; P < 0.001 compared with intervention groups)
Te-Wei Ho et al. (2016) [27] trial investigated the effectiveness of a telemonitoring program in reducing COPD-related re-admissions in Taiwan. A total of 106 patients were randomly distributed between telemonitoring and usual care of (n=53), each with the age group of 20 years or more, and 76% of patients were men. The telemonitoring patient group was trained to use a pulse oximeter, thermometer, and sphygmomanometer as a digital intervention before discharge, and patients had to report their symptoms daily till two months of discharge using the electronic diary, which consisted of standard questions related to disease symptoms, vital signs, weights.
Telemonitoring significantly increased the time to first re-admission for COPD exacerbation than in the usual care group (p = 0.026) and reduced the number of all-cause re-admissions (0.23 vs. 0.68/patient; p = 0.002) and emergency room visits (0.36 vs. 0.91/patient; p = 0.006) compared to the control group. Countries with small territories and high accessibility of medical services have better outcomes for patients with COPD, which was one of the findings of this RCT.
In a randomized controlled trial, Vianello et al. (2016) [28] investigated the effectiveness of home telemonitoring for advanced-stage patients with COPD in Italy. This study randomized 334 patients in the age group of 18 years or more into two groups of (n=230) with telemonitoring and (n=104) as the control group for one year. Patients in the intervention group were provided a TM system consisting of a finger pulse-oximeter and a gateway device for data transmission over a telephone line to a central data management unit located at the Veneto Regional e-Health Centre.
Results have shown evidence of a lower readmission rate for AECOPD for the telemonitoring group in comparison with another group [IRR = 0.43 (95% CI 0.19–0.98); p = 0.01 and 0.46 (95% CI 0.24–0.89); p = 0.01, respectively] but there was no clear evidence on prevention of hospitalization for patients with COPD using telemonitoring intervention.
Four studies however, found no significant difference in hospitalization and/or rehospitalization rate for a telehealth/telemonitoring intervention. These studies examined the impact of telemedicine and telemonitoring on patients with chronic obstructive pulmonary disease (COPD). They collectively revealed that telehealth interventions involving real-time video conferencing or telemonitoring of patients with COPD did not reduce the hospitalization rate.
For example, Sorknaes et al. (2013) [22] trial investigated the effect of real-time teleconsultations between hospital-based nurses and patients with severe COPD discharged after an exacerbation in Denmark. A total of 266 patients with a minimum age of 40 years and mean age of 72 years were randomized telemonitoring intervention (n=132) and control group (n=134). The telemonitoring intervention group used a built-in computer, including a web camera, microphone, and measurement equipment, and this randomized trial was carried out in two sites (Hospital One and Hospital 2). The results showed no significant difference between the intervention and control groups’ total number of hospital readmissions after 26 weeks. Total number of hospital readmissions after 26 weeks: mean 1.4 (SD 2.1) in the intervention group and 1.6 (SD 2.4) in the control group.
Additionally, no significant differences were observed in mortality, time to readmission, total hospital readmission days, or readmission days with AECOPD between the groups using real-time video consultations between patients discharged after hospitalization and hospital-based nurses. Hospital 2 showed a weak reduction in the readmission rate for patients with COPD, but these differences were insignificant. Extensive experience in teleconsultation and technologically mediated care for two hospital nurses is a potential factor for differences in results.
Andersen et al. (2023) [24] trial investigated the effect of telemonitoring on hospitalization rates for acute exacerbations of COPD in Denmark. There were 222 patients above 40 and a median age of 70. The telemonitoring group (n=110) and the control group (n=112) were randomized. The telemonitoring intervention consisted of home measurement of oxygen saturation, heart rate, peak expiratory flow, body weight, and completion of a standardized questionnaire with yes or no questions focusing on dyspnea, cough, sputum volume, and color, and alerts were triggered if these measurements reach the threshold. The monitoring was carried out using Tunstall Healthcare’s TM equipment for all weekdays of the first month and then three times a week for the next five months.
Telemonitoring significantly reduced the number of acute exacerbations of COPD hospitalizations during the intervention period compared to the control group. However, this reduction did not persist after the intervention period. This study also found that patients with repeated hospitalization have positive outcomes using telemonitoring as an intervention.
Køpfli et al. (2023) [25] aimed to assess the effect of telemonitoring on hospitalization reduction and readmission in patients with moderate to severe COPD in Denmark. One hundred ninety-eight patients with age group 40 or more were randomized between Telemonitoring(n=101) and standard care group [n=97] for six months of telemonitoring services in addition to standard care of COPD. The telemonitoring group received the equipment from Tunstall HealthCare for six months, and the respiratory nurse trained all the participants on handling the equipment within two days of discharge from the hospital. Telemonitoring equipment focused on measuring oxygen saturation, heart rate, lung function, body weight, and symptoms—assessment using standard questionnaires specific to dyspnea, cough, sputum volume, and color-related information.
However, the addition of telemonitoring to best practice management did not improve patient reported QoL and hospitalization in the short-term and long-term follow-up.
The last study which did not find a significant result tested the effectiveness of telemonitoring integrated into existing clinical services for patients with COPD in Lothian, Scotland (Reader et al. 2013) [26]. Here, a total of 256 patients were randomized between the telemonitoring group (n=128) and usual care (n=128). The telemonitoring group was provided equipment with a touch screen to record the data related to treatment and oxygen saturation, and this information was transferred to the clinical team using the secured broadband link.
The results showed that telemonitoring did not significantly benefit time to hospital admission duration when both the groups had access to the same level of clinical service. The mean number of COPD admissions was similar in both groups (telemonitoring 1.2 admissions per person (standard deviation 1.9) v control 1.1 (1.6); P=0.59). The mean duration of COPD admissions over one year was also similar between groups (9.5 days per person (standard deviation 19.1) v 8.8 days (15.9); P=0.88).
Finally, one study did not find evidence of non-inferiority Specifically, Jakobsen et al. (2015) [18] trial compared the effect of home-based telehealth hospitalization against standard hospitalization for patients with COPD in Denmark. A total of 57 patients with the age group of 45 years and more were randomized in the telehealth group (n=29) and the control group (n=28) for 30, 60, and 90 days after discharge. Studies have used home-based telehealth hospitalization equipment provided to patients for 24/7 virtual medical support by exchanging patient data. Telehealth equipment consists of a touch screen with a Webcam, pulse oximeter, spirometer, thermometer, nebulizer for aerosolized inhalation medication, oxygen compressor, and a medicine box containing antibiotics, prednisone, sedative, beta2 agonists, and anticholinergics.
This study did not find evidence of non-inferiority of home-based telehealth hospitalization to standard hospitalization regarding rehospitalization rates within 30 days after discharge (lower 95% confidence limit [CL], -24.8%; p=0.35).
Discussion
This systematic review aimed to provide a detailed analysis of existing available literature on the effectiveness of digital intervention to reduce hospital readmission for patients with chronic obstructive pulmonary disease (COPD). Overall, we found that there are positive impacts on patients with COPD’ outcomes of mobile-based, telehealth, and telemonitoring digital intervention. Specifically, many proximal drivers of COPD, such as adherence to treatment and self-management efficacy, were significantly improved, particularly by web and mobile-based interventions. However, results have not shown a consistent pattern of effectiveness of examined digital interventions.
Based on the included studies, telemonitoring, patient education, regular data reporting, and focusing on high-risk patients are standard features for studies with both positive and negative results. This suggests that the differences in outcome may be influenced by additional factors, such as the duration of follow-up, the specific components of telemonitoring interventions, or the tailoring of the intervention as per patient population, which needs further investigation.
The early introduction of remote monitoring is an efficient way to control the progression of COPD. However, the outcome is influenced by usability, user-centric design, and adaptability of digital devices by patients. Usability and user-centric design ensure that digital intervention devices are user-friendly and easy to navigate for patients with varying digital literacy and physical capabilities. Effective self-management is essential for patients with COPD, especially patients over 65 years who might have several chronic diseases concurrently, and self-management skills can be further improved by having personalized patient-provider bonding. Caregivers provide care to patients with special needs. Based on the latest report published by AARP, the National Alliance of Caregiving, out of 53 million caregivers in the USA, 47 million caregivers were family members [30], and it is critical to select and design a digital intervention that can be simpler to adopt and use by patients and caregivers. (Fernández et al. 2023).
Additionally, lack of knowledge about device features, insufficient training, and technical challenges are some of the barriers that influence the effectiveness of the outcome especially when patients need feedback on large amounts of data transmitted to address the psychosocial challenges and might feel anxious about the low reading of devices [31].
In addition to usability, technology acceptance and adoption play a critical role in the effectiveness of digital interventions, and it is directly proportional to patients’ actual engagement and use of technology. Technology acceptance refers to the willingness and ability of individuals to adopt and use technologies that are influenced by several key factors, such as user-centric design, ease of use, user’s attitude toward technology, social influence, and perceived usefulness. It has been found that digital interventions perceived as useful, easy for patients and caregivers, and supported by social norms are more likely to be accepted by users. [32,33,34] Therefore, understanding the end-user needs and addressing these factors are essential for the successful implementation and maximum efficiency and effectiveness of digital interventions to reduce hospitalization and readmission among patients with chronic obstructive pulmonary disease.
Our study has important implications for research and practice. For research, outcome data disaggregated by COPD severity (mild to severe) patient groups would provide more information on whom might benefit most from digital interventions. Personalized experience of clinicians rendering services and patients with COPD could also provide additional information on the effectiveness of specific digital interventions with potential areas of improvement. It is also unclear the role which could be played by training patients, clinicians, and caregivers to facilitate the uptake and effective use of established digital technologies.
This systematic review has highlighted the following areas of further research and investigation to enhance the understanding of results. First, future research should consider additional factors that impact the effectiveness of digital intervention, including variation in follow-up duration and customized digital interventions for specific patient populations. Second, Prioritize access to data on various COPD severity levels and age ranges and a larger sample size for robust results. Comparison of the effectiveness of synchronous telehealth, i.e., data transferred in real time over asynchronous where patients transmit data, for patients with COPD.
Finally, in practice, clinicians need sufficient training on using digital devices within patient populations and concerning data interpretation.
Limitations
Our systematic review included a multi-component package as digital intervention where self-management and manual intervention of health professionals were some of the contributing factors influencing the overall outcome.
We do not have the data on adherence to intervention to justify the reason for not working on specific digital interventions. We could not conclude the effectiveness of digital intervention for specific COPD severity (mild to severe) and patient age range (from 20 to 80 years), benefited from the specific digital intervention due to lack of disaggregated data part of included studies. Currently, some researchers have included smaller patient sample sizes, which might impact the overall effectiveness of the hospital readmission rate.
Due to the limited number of studies that met the inclusion criteria, our analysis did not demonstrate which specific digital intervention and specific subgroup with patient with COPD will benefit more than standard care. However, this demonstrates the essential gap in the literature. This systematic review has included published randomized control trials (RCTs) only, and no cluster-randomized or protocol trial design is included in the review, and results might have varied based on additional data. This has included all digital interventions related to short message service (SMS) (for reminders), mobile phones, personal digital assistants, web or internet-based interventions, telehealth, and telemonitoring.
Despite these limitations, this review had several strengths. First, our search timeframe included studies undertaken during the COVID-19 pandemic when the use of digital instruments in mobile, web, and telemonitoring has improved drastically.
Findings with respect to previous work
Our findings align with other systematic reviews on the effectiveness of devices used as part of digital intervention, and studies have also shown heterogeneous outcomes with a limited number of studies included. All the included RCTs having a digital intervention with or without self-management support to usual care.
For example, review (Janjua et al., 2021) [3], (Janjua et al., 2018) [11], and (McCabe et al., 2017) [12] is primarily focused on digital intervention in the overall management of chronic obstructive pulmonary disease in terms of health behavior, quality of life, and patient engagement, whereas this study is focusing on 30-day hospitalization or readmission
Conclusions
Overall, this systematic review provides insight into the impact of digital intervention on hospital readmission among patients with COPD. While some studies showed positive results, the evidence is mixed, and further research is needed to determine the pattern and consistency of these positive outcomes. COVID-19 has accelerated the use of digital intervention and created the opportunity for comprehensive research and investigation with more updated information and further impact on readmission.
There needs to be clear evidence on the constituency of positive results for these interventions, and future research is needed to determine if digital interventions have consistent positive results for patients with COPD.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- Digital Health:
-
Digital health comprises a broad range of technologies to deliver virtual medical or educational services.
- Web-based:
-
This includes using a web-based platform accessible via the internet using the standard web browser on a desktop, laptop, tablet, or smartphone without the need to stall additional software or applications.
- Mobile-based:
-
This includes using mobile communication devices such as smartphones, tablets, and wearable devices to exchange messages between patients and physicians via health alerts, vital sign changes, and tracking.
- Telehealth:
-
its synchronous two-way digital communication between patients and providers using telecommunication technologies such as video conferencing and telecommunication devices.
- Telemonitoring:
-
is the remote collection, transmission, and analysis of patient's health data using digital devices and electronic communication technologies, which helps providers monitor patients' health status, vital signs, and symptoms remotely outside of traditional clinical settings—for example, home oxygen saturation, heart rate, peak expiratory flow, and Body Weight measurements.
References
World Health Organization. Chronic obstructive pulmonary disease (COPD). World Health Organization: WHO. 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
Portillo EC, Wilcox A, Seckel E, Margolis A, Montgomery J, Balasubramanian P, et al. Reducing COPD readmission rates: Using a COPD care service during care transitions. Fed Pract. 2018;35(11):30–6.
Janjua S, Banchoff E, Threapleton CJD, Prigmore S, Fletcher J, Disler RT. Digital interventions for the management of chronic obstructive pulmonary disease. Cochrane Libr [Internet]. 2021;2021(4). Available from: https://doi.org/10.1002/14651858.cd013246.pub2
Elixhauser A, Au DH, Podulka J. Readmissions for Chronic Obstructive Pulmonary Disease, 2008. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs Agency for Healthcare Research and Quality. US 2008.
Press VG, Konetzka RT, White SR. Insights about the economic impact of chronic obstructive pulmonary disease readmissions post implementation of the hospital readmission reduction program. Current Opinion in Pulmonary Medicine. 2018 Mar [cited 2020 Feb 4];24(2):138–46. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5810972/
Mclean S, Nurmatov U, Liu JL, Pagliari C, Car J, Sheikh A. Telehealthcare for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. 2011; Available from: https://doi.org/10.1002/14651858.CD007718
Darzi A. National Health Service. London, England: Crown Publishing; 2008.
McLean S, Sheikh A. Does telehealthcare offer a patient-centred way forward for the community-based management of long-term respiratory disease? Prim Care Respir J. 2009;18(3):125–6. Available from: https://doi.org/10.3132/pcrj.2009.00006
Williams V, Price J, Hardinge M, Tarassenko L, Farmer A. Using a mobile health application to support self-management in COPD: a qualitative study. Br J Gen Pract. 2014;64(624):e392-400. Available from: https://doi.org/10.3399/bjgp14X680473
Seemungal TAR, Wedzicha JA. Acute exacerbations of COPD: The Challenge is Early Treatment. COPD. 2009;6(2):79–81. Available from: https://doi.org/10.1080/15412550902806011
Janjua S, Threapleton CJD, Prigmore S, Disler RT. Telehealthcare for remote monitoring and consultations for people with chronic obstructive pulmonary disease (COPD). Cochrane Libr. 2018; Available from: https://doi.org/10.1002/14651858.cd013196
McCabe C, McCann M, Brady AM. Computer and mobile technology interventions for self-management in chronic obstructive pulmonary disease. Cochrane Libr. 2017;2020(2). Available from: https://doi.org/10.1002/14651858.cd011425.pub2
Rosano A, Loha CA, Falvo R, van der Zee J, Ricciardi W, Guasticchi G, et al. The relationship between avoidable hospitalization and accessibility to primary care: a systematic review. Eur J Public Health. 2013;23(3):356–60. Available from: https://doi.org/10.1093/eurpub/cks053
Dalla Zuanna T, Spadea T, Milana M, Petrelli A, Cacciani L, Simonato L, et al. Avoidable hospitalization among migrants and ethnic minority groups: a systematic review. Eur J Public Health. 2017;27(5):861–8. Available from: https://doi.org/10.1093/eurpub/ckx113
van Loenen T, van den Berg MJ, Westert GP, Faber MJ. Organizational aspects of primary care related to avoidable hospitalization: a systematic review. Fam Pract. 2014;31(5):502–16. Available from: https://doi.org/10.1093/fampra/cmu053
Zhou L, Parmanto B. Reaching people with disabilities in underserved areas through digital interventions: Systematic review. J Med Internet Res. 2019;21(10):e12981. Available from: https://doi.org/10.2196/12981
Alkhaldi G, Hamilton FL, Lau R, Webster R, Michie S, Murray E. The effectiveness of prompts to promote engagement with digital interventions: A systematic review. J Med Internet Res. 2016;18(1):e6. Available from: https://doi.org/10.2196/jmir.4790
Jakobsen AS, Laursen LC, Rydahl-Hansen S, Østergaard B, Gerds TA, Emme C, et al. Home-based telehealth hospitalization for exacerbation of chronic obstructive pulmonary disease: Findings from “the virtual hospital” trial. Telemed J E Health. 2015;21(5):364–73. Available from: https://doi.org/10.1089/tmj.2014.0098
Ritchie CS, Houston TK, Richman JS, Sobko HJ, Berner ES, Taylor BB, et al. The E-Coach technology-assisted care transition system: a pragmatic randomized trial. Transl Behav Med. 2016;6(3):428–37. Available from: https://doi.org/10.1007/s13142-016-0422-8
Fors A, Blanck E, Ali L, Ekberg-Jansson A, Fu M, Lindström Kjellberg I, et al. Effects of a person-centred telephone-support in patients with chronic obstructive pulmonary disease and/or chronic heart failure – A randomized controlled trial. PLoS One. 2018;13(8):e0203031. Available from: https://doi.org/10.1371/journal.pone.0203031
Piette JD, Striplin D, Fisher L, Aikens JE, Lee A, Marinec N, et al. Effects of accessible health technology and caregiver support posthospitalization on 30-day readmission risk: A randomized trial. Jt Comm J Qual Patient Saf. 2020;46(2):109–17. Available from: https://doi.org/10.1016/j.jcjq.2019.10.009.
Sorknaes AD, Bech M, Madsen H, Titlestad IL, Hounsgaard L, Hansen-Nord M, et al. The effect of real-time teleconsultations between hospital-based nurses and patients with severe COPD discharged after an exacerbation. J Telemed Telecare. 2013;19(8):466–74. Available from: https://doi.org/10.1177/1357633x13512067
Zanaboni P, Dinesen B, Hoaas H, Wootton R, Burge AT, Philp R, et al. Long-term telerehabilitation or unsupervised training at home for patients with chronic obstructive pulmonary disease: A randomized controlled trial. Am J Respir Crit Care Med. 2023;207(7):865–75. Available from: https://doi.org/10.1164/rccm.202204-0643oc
Andersen FD, Trolle C, Pedersen AR, Køpfli ML, Børgesen S, Jensen MS, et al. Effect of telemonitoring on readmissions for acute exacerbation of chronic obstructive pulmonary disease: A randomized clinical trial. J Telemed Telecare. 2023;1357633X221150279. Available from: https://doi.org/10.1177/1357633X221150279
Køpfli ML, Børgesen S, Jensen MS, Hyldgaard C, Bell C, Andersen FD. Effect of telemonitoring on quality of life for patients with chronic obstructive pulmonary disease-A randomized controlled trial. Chron Respir Dis. 2023;20:147997312311577. Available from: https://doi.org/10.1177/14799731231157771
Pinnock H, Hanley J, McCloughan L, Todd A, Krishan A, Lewis S, et al. Effectiveness of telemonitoring integrated into existing clinical services on hospital admission for exacerbation of chronic obstructive pulmonary disease: researcher blind, multicentre, randomised controlled trial. BMJ. 2013 [cited 2024 Feb 29];347(oct17 3):f6070–f6070. Available from: https://www.bmj.com/content/347/bmj.f6070.
Ho T-W, Huang C-T, Chiu H-C, Ruan S-Y, Tsai Y-J, Yu C-J, et al. Effectiveness of telemonitoring in patients with chronic obstructive pulmonary disease in Taiwan-A randomized controlled trial. Sci Rep. 2016;6(1). Available from: https://doi.org/10.1038/srep23797.
Vianello A, Fusello M, Gubian L, Rinaldo C, Dario C, Concas A, et al. Home telemonitoring for patients with acute exacerbation of chronic obstructive pulmonary disease: a randomized controlled trial. BMC Pulm Med. 2016;16(1). Available from: https://doi.org/10.1186/s12890-016-0321-2
Garcia-Aymerich J, Hernandez C, Alonso A, Casas A, Rodriguez-Roisin R, Anto JM, et al. Effects of an integrated care intervention on risk factors of COPD readmission. Respir Med. 2007;101(7):1462–9. Available from: https://doi.org/10.1016/j.rmed.2007.01.012
AARP, for A. Caregiving in the United States 2020. AARP. AARP; 2020. Available from: https://www.aarp.org/pri/topics/ltss/family-caregiving/caregiving-in-the-united-states.html.
Althobiani MA, Shuttleworth R, Conway J, Dainton J, Duckworth A, Jorge A, et al. Supporting self-management for patients with Interstitial Lung Diseases: Utility and acceptability of digital devices. PLOS digital health. 2024;3(1):e0000318-8.
Kalun Calvin, et al. Human Factors Engineering and User-Centered Design for Mobile Health Technology: Enhancing Effectiveness, Efficiency, and Satisfaction. Human-Automation Interaction. 2022;12(15):97–118. https://doi.org/10.1007/978-3-031-10788-7_6.
Yan M, Or C. Factors in the 4-week acceptance of a computer-based, chronic disease self-monitoring system in patients with type 2 diabetes mellitus and/or hypertension. Telemed J E-Health. 2018;24(2):121–9.
Yan M, Or C. A 12-week pilot study of acceptance of a computer-based chronic disease self-monitoring system among patients with type 2 diabetes mellitus and/or hypertension. Health Informatics J. 2019;25(3):828–43.
Acknowledgements
Not applicable.
Funding
This study has not received any funding.
Author information
Authors and Affiliations
Contributions
V.M. and D.S. designed the framework and topic. Three review authors (V.M., D.S., and CM) finalized the search strategy and screening criteria to flag the articles as eligible, potentially eligible, or unclear. V.M. retrieved full-text study reports of all potentially eligible studies, which are further reviewed by D.S. and C.M. for inclusion, listing reasons for exclusions on ineligible studies and all disagreements resolved through multiple discussions. V.M. and D.S. worked together on the data extraction strategy. V.M. extracted the outcome data from a mutually agreed strategy among three review authors (V.M., D.S., and CM). D.S. and C.M. have further reviewed extracted data independently to check the consistency of the result.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mishra, V., Stuckler, D. & McNamara, C.L. Digital Interventions to reduce hospitalization and hospital readmission for chronic obstructive pulmonary disease (COPD) patient: systematic review. BMC Digit Health 2, 46 (2024). https://doi.org/10.1186/s44247-024-00103-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44247-024-00103-x