Abstract
Background
The growing popularity and affordability of immersive virtual reality (VR), as adjunctive non-pharmacological interventions (NPIs) for chronic pain, has resulted in increasing research, with mixed results of its effectiveness reported. This randomized controlled superiority trial explored the effects of a home-based adjunctive 3D VR NPI for chronic pain in cancer patients, compared to the same NPI experienced through a two-dimensional (2D) medium.
Methods
The NPI used four different applications experienced for 30 min for six days a week at home for four weeks using established cognitive distraction and mindfulness meditation techniques. Participants were randomly assigned (N = 110) into two arms: a VR group (n = 57) where the NPI was delivered through a VR system, and a control group (n = 53) which used a computer screen for delivery. Participants were blinded to which arm of the study they were in, and sequence of the NPI applications experienced was randomized. Primary outcomes of daily pre/post/during exposure, and weekly average pain scores were assessed via the Visual Analog Scale (VAS) and the Short Form McGill Pain Questionnaire (SF-MPQ), and secondary outcomes of weekly Quality of Life (SF-12), and sleep quality (Pittsburgh Sleep Quality Index) were measured.
Results
Findings indicate VR applications were not significantly superior to the 2D group, but both VR and control NPIs provided clinically important pain reduction for participants when experiencing significant daily pain of a VAS ≥ 4. No significant adverse effects were encountered, although many of the participants in the VR group reported some cybersickness in certain applications (VR group n = 46 vs 2D group n = 28).
Conclusions
Overall, VR did not provide superiority as an NPI for pain relief compared to 2D computer-based applications. For those experiencing significant pain, cognitive distractive applications appeared superior for VR-based pain reduction during exposure, whilst meditative applications supplied better pain relief post-exposure. Findings from this trial support some clinical efficacy of home-based VR immersive experiences as NPIs for chronic cancer-related pain but in this context the 2D computer-based applications demonstrated similar value.
Trial registration
Clinicaltrials.gov, identifier NCT02995434, registered 2017–07-31.
Similar content being viewed by others
Introduction
Background
Cancer survivorship has increased over the last two decades, and with advances in treatment this population is expected to grow further worldwide [1, 2]. Chronic pain remains the most common long-term effect, caused by cancer or its associated treatments [3, 4], and can be mild to severe [5]. Ongoing pain related to cancer, or its treatment is often difficult to manage and causes substantial suffering and disability. Patients often exhibit and endure persistent pain which affects physical and psycho-social health, impacting energy levels, cognitive and social functioning, and sleep [6,7,8,9]. Despite existing pain treatments, 40% of cancer survivors continue to experience chronic pain [5, 10].
Non-pharmacological interventions (NPIs) as adjunctive methods of pain control are of increasing interest and relevance for clinical practice and research, especially with ongoing opioid crises worldwide [11]. NPIs show promise for reducing cancer-related pain with few adverse effects [12,13,14]. More recently, as a more immersive medium, the use of immersive virtual reality (VR) as an NPI has become an area of high impact research [15,16,17,18]. A number of successes have been reported in the use of VR for the treatment of acute pain, whilst evidence of the value of its use for chronic cancer-related pain and other forms of chronic pain continues to develop [19,20,21,22,23,24,25,26,27].
Virtual reality is theorized to be more immersive than conventional 2D computer-based multimedia due to several factors. Firstly, VR headsets typically offer a wide field of view and stereoscopic vision, which enhances depth perception and spatial awareness within the virtual environment. This allows users to perceive distances, sizes, and spatial relationships more accurately, contributing to a greater sense of immersion [17, 18].
Secondly, VR provides a more comprehensive sensory experience compared to 2D media in by supporting multisensory engagement. As users can see their virtual hands and actually manipulate materials in the VR world (through VR hardware such as headsets and motion controllers) this creates a more immersive and realistic environment for users. In this way VR technologies and the shutting out of any other visual stimulation create a sense of "presence" for users, where they feel as if they are physically present, of being there, within the virtual environment [18, 20].
Overall, this combination sensory engagement, spatial awareness and the resulting sense of presence are theorized to make VR a more immersive medium than traditional 2D screen-based digital media.
The concept of pain distraction therapy has proven interest in VR pain applications, particularly for acute pain. Distraction therapy involves interventions that shift a person's attention away from the pain they are experiencing, to experiences that require greater information processing [28, 29]. This can be a powerful moderator of the pain experience, and active distractions, such as playing a game or solving a puzzle, or passive distractions such as listening to music appear effective [29, 30]. The more engaging the activity, the more likely it will distract attention from the pain experience, relegating pain to a less salient “background” of attention [31, 32]. VR technology offers a powerful distraction from pain by immersing participants in computer-generated three-dimensional (3D) environments that offer strong sensory and perceptual engagement. Such environments cognitively engage participants through activities such as exploration of richly detailed and complex spaces, film-like narratives or solving 3D puzzles, thereby drawing attention away from pain signals and sensations and thus actively reducing pain perception [33,34,35].
Similarly, mindfulness-based meditation for pain control has been used to refocus neurological activity by greater activation of cortical and other regions, altering the appraisal of nociceptor and other sensory stimuli and increasing interoceptive awareness [36,37,38,39,40]. However, despite over 40 years of scientific research, the nature, mechanisms, and value of mindfulness techniques remains controversial, and there is currently no universally accepted technical definition of ‘mindfulness’ [41,42,43]. For the purpose of this work, VR-guided mindfulness meditation can be seen as a parallel NPI to VR distraction, in that both are used to neurologically mediate some of the negative effects of pain by altering its perception. As mindfulness is frequently promoted as a pain reduction technique in chronic pain and has been advocated in several VR pain studies, [36,37,38,39, 44,45,46] it was selected as a key technique for use here.
With the theorized advantages of immersive VR and its growing exploration as a NPI in pain management, a number of studies comparing the effects of VR immersion to other media in various clinical chronic pain settings have occurred [20,21,22, 24, 25, 27], and also for chronic cancer-related pain, but with some mixed findings [44,45,46].
Objectives
The primary aim of this RCT was to explore to what extent VR computer-based applications were advantageous for daily home-based chronic cancer-related pain management, compared to equivalent applications experienced on two-dimensional (2D) computer screens. An in-vivo experiment using a series of four different immersive experiences each using a different computer-based application for a week for 30 min a day was devised, and the following primary null hypotheses were tested:
-
1.
There is no difference between the reported daily pain experiences of participants during or after exposure to VR immersive environments, overall and within four different VR immersive environments, compared to the equivalent applications experienced on a 2D computer screen.
-
2.
There is no difference in self-reported weekly pain, quality of life and sleep experiences of participants exposed to different VR immersive environments over the period of the study, compared to participants exposed to the equivalent applications experienced on a 2D computer screen.
Secondly, the researchers also sought to explore if any potential improvements beyond the immediate suppression of pain, such as improvements in quality of life, function or sleep were reported with the use of these NPIs.
Methods
Design
The study was a parallel two-arm (VR vs. non-VR control) exploratory participant-blinded prospective RCT with 1:1 allocation (clinicaltrials.gov, TRN: NCT02995434, registered 2017–07-31). It was primarily conducted with rolling recruitment in British Columbia as well as Alberta, Ontario, and Quebec between August 2017 and December 2022.
Sample size
Sample size was determined by a power analysis to test group differences in VAS pain intensity between two arms. Due to limited recruitment feasibility, a third no intervention arm was impractical, and the two arms were considered sufficient to establish the impact of VR as a discrete pain therapy. As reliable estimates of expected effect size were unknown, and a standardized approach to estimating power in mixed effects modelling studies has yet to emerge, the study was practically powered to detect a medium effect (0.5 SD change). This was considered a reasonable clinically meaningful impact to obtain 80% power based on a repeated measures analysis of variance (RM ANOVA) with 2-tailed alpha of 0.05 model [47]. Power calculated using the G*Power application suggested a minimum sample size of 100 participants (50 in each group) [48, 49].
Participants
Community-dwelling adults with cancer-related chronic pain were recruited through postings in cancer clinics, pain clinics, hospitals, support groups, support networks (PainBC, People in Pain Network), physician networks, social media, and the REACH BC research volunteer website. Initial recruitment focused on BC. Recruitment was expanded to Alberta in 2020 and Canada-wide in 2022. The inclusion criteria were:
-
Aged > 18, with a past or current diagnosis of cancer
-
Past or current treatment with standard cancer therapies
-
Experiencing chronic pain (defined as ongoing daily pain ≥ 3 months, with a self-reported daily pain Numeric Rating Scale score ≥ 4 out of 10)
-
Able to understand the English language (read and write)
-
Normal stereoscopic vision
-
Readily able to move head up, down, left, and right, and able to wear a headset
-
Have fine motor control in one hand sufficient to use a game controller
-
Have space at home for a computer and monitor
People who self-reported having significant cognitive issues, non-cancer-related pain, a history of seizures, claustrophobia, or high susceptibility to motion-sickness were excluded. All participants were paid a $400 honorarium upon completion of the study to compensate them for their time.
Blinding
The study was single blinded as control and VR participants were recruited in the same way, and the term "immersive multimedia" was used in all recruitment and study materials rather than “VR” to blind participants about the type of intervention they would receive. Participants in the control arm were unaware of the VR arm and vice versa. The research coordinator and statistician analyzing the data were also blind to allocation. Due to the nature of the intervention, the research assistants responsible for setting up equipment, training participants, and conducting technical support were not blinded.
Intervention
The adjunctive NPI tested four separate computer-based immersive applications using two established approaches to chronic pain management using VR: cognitive distraction, and introspective mindfulness relaxation [20, 23, 36, 50, 51]. These independent interactive experiences were selected so as to prevent boredom through repetition and expose participants to four different forms of VR experience, rather than designed as a specific sequenced program of therapy. They were delivered through either a computer-based VR system, or a laptop in the 2D (control) group. The VR equipment consisted of an HTC Vive (HTC, Taiwan) head mounted display (HMD) with a resolution of 1080 × 1200 pixels per eye, and 110° field of view at a 90 Hz refresh rate. Audio was delivered through the Vive Deluxe Audio Strap high-fidelity stereo headphones, and two hand controllers were used for application interaction, movement and navigation in the VR environment. Two infrared tracking modules enable 6-degrees-of-freedom spatial motion tracking of the HMD and controllers. The desktop computer running the VR system included hardware sufficient to run all activities at the highest graphical settings available for the applications. The non-immersive control group participants received a 17″ laptop with a mouse, an XBOX game controller, and stereo headphones.
Two commercially available applications were used for cognitive distraction interventions. Obduction (OB: Cyan Ventures, Mead, USA) is a first-person adventure game that involved exploring a strange new environment, solving puzzles, and uncovering mysteries.
The other was Cape Lucem—Seize the Light (CL: Application Systems, Heidelberg, Germany), a VR puzzle game that involved manipulating and redirecting light beams in 3D space with different pieces to unlock objects. Participants used hand controllers to move puzzle pieces. CL was unavailable in a suitable format for laptop use, so another geometric puzzle solving application was used as a substitute for the control group, The Witness (WN: Thekla, San Francisco, USA) which requires participants to solve various maze-based puzzles. These applications were not specifically designed for pain relief, but selected as powerfully engaging experiences that provide immersive cognitive distraction.
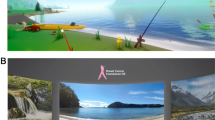
Two mindfulness focused applications targeted at introspective pain management were also used: the Virtual Meditative Walk (VMW), and Wildflowers (WF; Mobio Interactive).
The VMW involved moving along a forested path while listening to a guided meditation for pain with accompanying relaxing music [17, 38]. There were 3 meditations in sequence, and participants were able to freely look around as the participant was slowly moving along a fixed curved path through the forest.
The WF application involved controlling a butterfly from a third-person perspective to explore a peaceful island. The participant could freely look around and control the butterfly's flight path three dimensionally using the controller. The application included locations for ten guided meditations, location-specific relaxing soundscapes, and interactive musical sculptures. Both applications were adapted by the developers for use in this project.
Outcomes
Data collection strategy
The data collection strategy was primarily designed to account for individual pre/during/post exposure changes in pain with the Visual Analogue Scale (VAS: public domain) [52] and any weekly trend from the initial baseline using the Short Form McGill Pain Questionnaire (SF-MPQ: public domain) [53]. The secondary goal was to explore in the Health Survey Short Form (SF-12: Licensed from the Rand Corporation) [54] and Pittsburgh Sleep Quality Index (PSQI: public domain) [55] over the four weeks to identify any cumulative trends in these quality-of-life indicators from the initial baseline.
Primary outcomes
Daily pre, during and post intervention exposure pain was assessed using the VAS. The VAS is a single item linear self-reported pain scale from no pain (0 mm) to worst pain imaginable (100 mm). It was selected as a well-established and validated subjective measure for acute and chronic pain [52]. The measure has demonstrated moderate-high correlation with the numeric pain fidelity scale (correlation coefficient from 0.62–0.91) [56] and high reliability (intraclass correlation coefficient = 0.97 [57]. The clinically meaningful change for the VAS has been shown to be between 9 and 12 mm; this study adopted the convention of 10 mm as the minimum clinically important difference (MCID) [58,59,60].
The SF-MPQ was used to assess for any pain trend from the initial baseline at the end of each week. The measure includes 15 items (rated not applicable, mild, moderate, severe) assessing sensory pain (11 items) and affective pain (4 items), as well as a weekly VAS component scored out of 10 (VAS indicated at the time of the survey). Higher scores mean greater pain. This instrument is also well-validated and established in clinical use [53] and has demonstrated good sensitivity to change over time in chronic cancer pain [61]. A MCID has not been established for the SF-MPQ, although a clinically important change (CIC) has been identified as a mean total score of > 5 out of the total of 55 [62,63,64]. Its use here was designed to examine trends over the 4-week period of the RCT. A brief end of trial RCT descriptive survey was also completed by participants asking if they found any ongoing pain relief after NPI use (and if so, and for how long), if they reduced their pain medication requirements, or if they were helped in other ways not captured.
Secondary outcomes
The SF-12 was used as a self-reported outcome measure assessing health-related quality of life at the end of each week, and any trends from initial baseline. It includes 12 items with binary response items and 3–6-point Likert items. The SF-12 is scored using proprietary software to generate a physical composite (PCS) and mental composite (MCS) health scores ranged 0–100, with scores above or below 50 indicating greater or poorer health than normative mean, respectively. The measure has demonstrated validity (internal consistency αPCS12 = 0.89; αMCS12 = 0.88) and reliability (Interclass correlation: ICCPCS12 = 0.82; ICCMCS12 = 0.73) in a sample of 420 adult cancer patients [54]. MCID is smaller in patients with longer pain duration and better baseline quality of life, and so based on prior medical studies a MCID > 3.77 in the MCS and > 3.29 in PCS were adopted as clinically relevant for this study [65, 66].
Similarly, the Pittsburgh Sleep Quality Index (PSQI) was used as a self-reported outcome measure assessing sleep quality at the end of each week [55, 67]. The measure includes 19 items asking about sleep schedule, duration, disruption frequency (4-point Likert scale), and quality (4-point Likert scale). Scores range from 0–21, with higher scores indicating worse sleep quality. The PSQI has demonstrated validity in cancer patients with Cronbach’s alpha ranging from 0.77–0.81 [68]. Estimates for the MCID for the PSQI index score range from 1.3 to 4.4 [69].
Potential moderator and exploratory outcomes
As no suitable tool was available when the RCT commenced including both audio-visual fidelity immersion and presence as characteristics, a simple 28-item immersion and presence survey instrument was developed based upon prior work exploring immersive fidelity (quality of audio-visual representation on sense of immersion in the environment) and presence (sense of dislocation from the real world and being present in a virtual world) [70,71,72,73,74]. Items used 5-point Likert scales, with two global items assessing immersion and presence on 10-point Likert scales. This survey incorporated the previously validated Immersion Experience Questionnaire (IEQ) [75] and was administered at the end of each week of the trial. Potential moderator demographic variables were also collected including age, gender and type of cancer. Any reported cybersickness (VR-induced motion sickness) was also recorded at this time by participants weekly on a 5-point Likert scale, with an option to add comments [76,77,78].
Randomization
Applicants were screened for eligibility and assigned a participant ID by the research coordinator. The research assistant responsible for equipment setup would then determine the participant’s group from the assignment sheet. Participants were randomly assigned to either the VR or control group in blocks of 12 using a Latin Square design assignment sheet prepared by a professional statistician. Each block of 12 included six unique permutations for order of the NPI applications used to effectively randomize allocation and avoid sequencing effects (Fig. 1).
Procedure
During the trial, each participant engaged in a daily 30-min immersive media therapy session in their own homes, either as a VR activity or a screen-based laptop activity for the control group. In associated literature using VR or hypnosis for chronic pain it has been demonstrated that studies utilizing interventions comprised of 6–12 sessions can result in significant improvements in pain control and outcomes [24, 79, 80]. It is reasonable to compare hypnosis as a similar NPI with regard to its effect on pain, as it appears to alter the central processing and appraisal of pain in a similar manner. Additionally, studies that described positive results of hypnotherapy, guided imagery meditation, mindfulness and VR for pain frequently report 8–12 sessions of exposure between 30–40 min [79, 80]. Given this, an exposure to 24 therapeutic sessions of 30 min duration was considered adequate to establish if any clinical effects of VR in chronic pain reduction were evident [24, 79,80,81,82]. Additionally prior pilot work and manufacturers guidelines for length of exposure suggest 30 min exposure duration was suitable [23].
The NPI was used six days per week for one month, using one of four different applications (one per week) in sequence, with a one-day rest period at the end of the week before changeover to the next application (providing 12 h of total NPI exposure over the month). Equipment was initially set up in the participant’s own home at the start of the month with orientation and training involving a detailed overview of the study, instruction and provision of a data collection binder with daily and weekly measures, as well as familiarization with equipment and applications. The binder was sectioned into each week, with daily sheets including instructions to record the time spent each day, and their pre, during, and post exposure VAS pain scores. To avoid the effects of interrupting the immersive activity, participants completed their “during” VAS pain score immediately after their daily session by “thinking back to somewhere in the middle of your session and recalling your pain at that time.” This approach had been demonstrated as a practical solution to this issue in a pilot study [23]. Participants were supplied a timer they were asked to set for 30-min. Data collection was self-reported. At the end of each week, participants also completed the SF-MPQ, SF-12, PSI, and the Immersion/Presence survey, including cybersickness fidelity and any deviations from the procedures. The end-of-study questionnaire included the option to add comments on how useful they found the NPI overall and any other thoughts they wished to record about the therapy.
Practical support was provided through simple instructional materials and walkthroughs for the four different applications. A help service by phone, email or teleconferencing (with remote desktop computer access) was also provided for participants to contact a research assistant for technical support or any other issues they met during the trial. Participants were encouraged to contact them if anything seemed problematic or if they felt stuck.
Statistical analysis
A first exploration of all outcomes across all participants was undertaken, using an intention to treat analysis (where all participants were included in the statistical analysis and analyzed according to the group they were assigned, regardless of individual changes in protocol). For the primary outcomes of interest, a minimum clinically important difference (MCID) of 10 mm on the VAS scale was adopted.
Linear mixed effects modelling was used to establish whether there were differences in the outcomes of interest between the VR and control groups. Patient-level random intercepts were considered to account for the repeated outcome measures. Interaction terms of participant exposure (VR or non-VR) and time (before, during and after for daily outcomes and by week for weekly outcomes) were included in each model and used to ascertain whether changes in the outcomes of interest from baseline—before each activity for the daily and before exposure to NPI for the weekly outcomes and at specific time points – during and after each activity for the daily and at day six for the weekly outcome measures – were different between the VR and non-VR groups. Baseline demographic characteristics and duration of exposure to each environment for the daily outcomes were considered for adjustment in the full models. Terms were sequentially removed from the full models if their exclusion did not affect model fit. Reduced models were compared to full models using the Akaike Information Criteria (AIC) and those with the lower values were identified as the final models for each outcome. The AIC criterion, unlike other criteria, favours reduced models as it penalizes complex models with more parameters, thereby discouraging model overfitting. Using the final models, adjusted values of each outcome per group were estimated and presented as mean summaries with standard errors as a measure of dispersion. The 95% confidence interval (CI) of the fixed effects were estimated using the bootstrapping method and graphical plots of residuals and fitted values were used to determine whether normality and constant variance assumptions were met. To explore potential correlations between video and audio fidelity, and cyber sickness between applications in the immersion survey a two-sample t-test was also used. All analyses were conducted using R statistical software in which the lme4 package [83] was used to fit the mixed effects models, emmeans package [84] was used to calculate the adjusted outcome values and the pbkrtest package [85] to calculate the 95%CI.
COVID-19 pandemic study modifications
Due to the global COVID-19 pandemic, the study was paused completely at three separate times between March 2020 to February 2022 due to the need to follow ongoing public health and safety requirements. The study was initially restarted with modified protocols to minimize physical contact and ensure safety according to public health and REB guidelines. However, in January 2022, to maintain falling recruitment, the set-up protocol was modified to be completely remote, which also allowed participants form outside of BC to take part, and so recruitment was expanded to include cancer support centres across Canada. Participants were shipped all study equipment and were asked to view a brief tutorial video on how to set it up beforehand. Once the participants received their equipment, a research assistant helped them conduct the set-up and orientation via teleconference.
Results
Participant characteristics
A total of 110 participants were recruited for this study: 100 from BC, 2 from Alberta, 7 from Ontario, and 1 from Quebec. A total of 10 participants discontinued participation within the first week due to time commitment (n = 5), changes in medication (n = 2), change in interest (n = 2), and cybersickness (n = 1). Figure 2 depicts the patient flow through the study, and Table 1 shows the overall participant characteristics.
Of the 100 participants from whom baseline data were collected, one chose not to disclose sex and gender, while the remaining participants were all cisgender with the majority being female (69%) overall and in both groups. Participants in the VR group were similar in age to those in the control group (Table 1). Many participants (n = 69) had prior computer-gaming experience with more in the VR group reporting slightly more gaming experience than the control group. Table 1 shows the most common cancer type was breast cancer, followed by lymphoma in both groups, while other types represented by < 5 participants per group included cancers such as kidney cancer, melanoma, among others. The majority (n = 85) of participants overall and in both groups also reported other conditions besides cancer and its treatment that contributed to their pain history, and most were using pain medication, especially prescription medications. Nearly all participants engaged in other NPI activities for pain management (Table 1).
Effects of VR interventions on participants with chronic cancer-related pain
VAS daily pain outcomes
The data exploration demonstrated highly varied pain experiences by many participants throughout the trial, with many beginning their daily activity with pain below a 40 mm VAS score, or even with zero pain on some days. As assessment of an NPI for pain on days when participants reported none is problematic, a sub-group analysis was also undertaken excluding data from participants whose pre-exposure VAS score was less than 40 mm on that day, to compare effects of the VR NPI on participants who were experiencing more substantial pain at the time.
Across all activities, for all participants the mean change in VAS from pre to during NPI exposure was -7.3 ± 9.5 mm in the control group and –8.8 ± 7.4 mm in the VR group; these changes ranged from a mean weekly decrease of -43.5 mm to a mean weekly increase of + 13.3 mm in the control group and -30.9 to + 4.2 mm in the VR group. The mean VAS changes from pre to post was -8.0 ± 12.4 mm (range -43.9 mm to + 18.5 mm) and -7.4 ± 9.2 mm (range -33.7 mm to + 12.0 mm) in the control and VR groups respectively Typically, there was a split between participants finding the VR or control NPIs effective or ineffective in all applications (Fig. 3).
In total, 43 VR participants and 37 control participants reported clinically meaningful pain reduction (VAS decrease ≥ 10 mm) on average for at least 1 week, either during or immediately after NPI exposure. We grouped participants according to whether they experienced meaningful pain reduction during only meditative activities (for either one or both meditative activities), only cognitive activities (one or both), a mixture (at least one meditative and one cognitive), all four activities, or for none of the activities (Table 2). The control group had nearly double the number of participants who did not experience clinically meaningful pain reduction (n = 13 vs n = 7). While both groups showed similar numbers of participants who responded to meditative only, or both meditative and cognitive, the VR group had more participants respond only to cognitive activities compared to control (n = 19 vs n = 7).
VAS daily pain scores during and post exposure
Only during exposure, reductions in pain for the cognitive applications (OB, CL) amongst participants in the VR group were clinically meaningful (-13.16 mm, 1.08SE and -12.37 mm, 1.14SE: Table 3). The VR group post-exposure mean scores overall, and for these cognitive applications, showed a reduction from during exposure mean scores, whilst the meditative applications (VMW and WF) demonstrated the opposite trend in the VR group where post exposure mean VAS scores were higher than during exposure (Table 3).
There were no clinically meaningful improvements overall or for any applications in the control group, although they approached clinical significance during exposure mean scores for the cognitive applications WN and OB (Table 3). In the control group, during exposure pain reduction was also somewhat better for the cognitive applications than the meditative applications (Table 3). Notably, in the control group, the post-exposure reductions in mean pain scores were higher than during exposure in the meditative applications, approaching clinical significance for the VMW (-9.51, 1.03SE).
The VR group showed a moderately superior performance in pain reduction compared to the control group for the cognitive applications (> 10 mm vs < 10 mm reduction), but overall, there was no evidence of statistically significant differences between the VR and control group performance, as mean score differentials were marginal.
The sub-group analysis of those with a VAS baseline of ≥ 40 mm (substantial pain on the day) revealed more nuanced results (Table 4). The reductions in mean pain scores during exposure sessions among participants in the VR group were also clinically meaningful overall and for all activities (from -10.13, 1.33SE to 14.55 mm, 1.35S) except the VMW. The post exposure VR group data showed that overall, and in the cognitive OB and WF application mean scores, clinically meaningful pain reduction was evident (from -10.42 mm, 0.72SE to –11.11 mm, 1.35SE). Also, that the meditative VMW and WN applications approached clinical significance. Similar to the complete sample analysis, the post exposure scores in the VR group were lower than that achieved during exposure for the cognitive applications, whilst the meditative applications showed the opposite.
In the control group, the pain reduction amongst participants during exposure, and post-exposure overall and for all applications also showed clinically meaningful improvements (from -10.99 mm, 1.25SE to –15.46 mm, 1.63SE), except for the WF application during exposure (which approached clinical significance: mean -8.81, SE 1.42). The post exposure mean scores were also superior to during exposure overall and for all applications except for WN in the control group. The cognitive applications OB and CL/WN provided the greater reported pain reduction in both groups, and the highest mean pain reduction recorded in the RCT for the cognitive WN application in the control group (mean -15.46, SE 1.63). As previously, between groups, the group differences were not significant with overlapping 95% CIs in this sub-group (Table 4).
Post-exposure pain severity and interference
In the final trial completion descriptive survey, 49% of the participants indicated that pain relief persisted for some time after NPI exposure (Fig. 4). This occurred similarly across both arms, with 32% of the control arm and 25% of the VR arm participants reporting persisting effects. Some (19%) indicated no post exposure effects, and the length of post exposure pain relief reported by others was highly varied, although most (29%) indicated it was an hour or less. The only observable difference noted between arms, was for pain relief lasting 1–2 h, where 11% of the control arm compared to 3% of VR participants identified effects of this length. A few participants (12%) reported an impact over two hours, and 6% over four hours.
In terms of impact on medication use, 25% of participants indicated some reduction, with 15% of the VR arm indicating they used less analgesics, compared to 10% of the control arm on days when they used the NPIs.
SF-MPQ pain questionnaire
End of week pain scores across sensory, affective, and VAS pain components were all decreased compared to baseline in both groups (Fig. 5). However, the only clinically meaningful baseline decrease observed was the week 4 total score in the control group (-5.44, 1.03SE). Comparing weekly baseline differentials between groups, the only point where the VR group showed a greater decrease than control group was for the VAS component in week 3 (Group difference = -0.59 cm 95%CI: -1.48, 0.18); in all other instances, control group showed greater decreases from baseline. However, none of the SF-MPQ between group differences were statistically significant. The complete results can be found in the supplemental materials (Supplemental Table 1).
Quality of Life (SF12)
For all participants overall, the SF12 scores in both groups did not appear to change significantly over the period of the trial (Figs. 6 and Table 5). The mean physical and mental health quality of life component score at baseline for participants in the VR arm were slightly lower as compared to those participants in the control arm. The changes in weekly mean physical quality of life component scores were significantly better for participants at week 3 in the VR arm (3.40, 0.92SE) compared to the baseline before any NPI (week 0), and in the VR arm compared to the control arm at week 3, at which point the difference was clinically meaningful (3.79, 95%CI: 1.02—6.08) between groups. For the mental health quality of life component however, the changes in the mean weekly scores from baseline showed clinically meaningful improvement for participants in weeks 2 and 4, (4.27, 1.20SE, and 5.22, 1.20SE respectively). Also, the control arm participants performed better in the mental health component during week 2 where the difference between groups was clinically meaningful (-3.90, 95%CI: -7.35—-0.48: 5). All significant changes were marginal in terms of clinical importance.
Pittsburgh sleep quality index
In all participants both PSQI groups did not meet the MCID over the period of the trial, except for a significant PSQI reduction (improvement) in control arm participants by the end of week 4 (-1.26, 0.41SE: Fig. 7 and Table 6). Although no progressive trend was evident, the mean PSQI among VR participants was higher compared to that of control arm participants at baseline and at all weeks, but not significantly so. Although not statistically significant, the mean weekly change in the sleep quality index from the baseline index was better for participants in the control arm compared to the VR arm in all weeks except week three where participants in the VR arm had a better PSQI change (Table 6).
Immersion and presence survey
In the immersion and presence survey piloted there was a > 90% completion rate for the questionnaire across all applications. Participants reported exposure to the NPIs on 23.1 days (SD = 2.0) on average out of the expected 24 days. There were no notable differences between groups (23.4, SD = 1.5, and 22.8, SD = 2.5 for the control and VR group, respectively). Overall, participants did not distinguish any statistically significant differences between the video and audio fidelity scores across the applications, except for the VMW application control arm where participants reported significantly higher visual fidelity scores compared to the VR participants (Control mean 3.9, SD 0.6 vs VR mean 3.6, SD 0.7). The complete results can be found in the supplemental materials (Supplemental Table 2).
Acceptability and adverse events
The VR interventions proved very acceptable to most participants. The majority of participants navigated through the experiences independently, although 31% required technical support by e-mail, phone or remote access during the study. This included help with software and hardware issues and gameplay assistance, suggesting that these technologies, though maturing, are not yet universally suitable for independent use.
Approximately 5% of participants deviated from using the assigned VR experiences in the allocated sequence. Some due to feeling ill on the day or other external factors, but some reported this was due to frustration with the ability to complete some of the cognitive activities (OB and CL-WN particularly), or navigating through the VR experiences (OB, CL-WN & WF). However, these were only reported issues in about 2% of all weekly activity and were reported in both the VR and control arms.
The most significant adverse effect of the VR intervention proved to be cybersickness [76, 77]. The majority of the participants reported some cybersickness occurring in the weekly surveys over the trial (n = 74), with 115 reported incidents in the VR group (66%: n = 46), versus 60 in the control group (34%: n = 28). The VR participants using the VMW, and WF applications demonstrated significantly higher cybersickness scores than the control (VMW Control mean 0.3, SD 0.6 vs VMW VR mean 1.0, SD 1.3; WF Control mean 0.4, SD 0.7 vs WF VR mean 2.3, SD 1.5) compared to the control participants (p < 0.001: Supplemental Table 3 and Fig. 8). Those VR participants using the OB application also had somewhat higher cybersickness scores than the control group (OB Control mean 0.9, SD 1.3 vs OB VR mean 1.4, SD 1.3), that approached statistical significance (p = 0.061). In the majority participants indicated this was mild and transitory, although two reported incidents using VR the sickness was severe enough to require rest afterwards and in one case use of an anti-emetic. One VR participant commented: “I was very, very motion sick the first day (and I never get car sick), I remained motion sick for the better part of the afternoon as well. I had eaten breakfast about 30 min [sic] before doing the VR.”
Six participants also noted the weight of the VR HMDs and associated neck ache was a factor in length of time they were able to use the applications. E.g., “I did not notice pain until the headset began causing pain for my head and neck from its weight. Just noticed the head & neck pain immediately afterwards.” Whilst one participant also reported mild eyestrain with use of the HMD.
Discussion
This exploratory study examined the extent to which home-based VR NPIs may reduce pain compared to a traditional 2D computer screen in people with chronic cancer-related pain. Participants included more females than males, possibly due to the proportion (69%) of breast cancer participants. This was the most common form of cancer represented by the sample (46%), followed by lymphoma at 23%. Although lung cancer is higher in the general population, lung cancer has a high mortality rate [86]. Hence the sample likely represents the range of cancer survivors with notable chronic pain issues. Most participants (69%) had some prior videogaming experience, and this may reflect a degree of self-selection into the study. However, this reflects a similar proportion to that found in the general population at around 63% [87]. Most (63%) were using prescription medications including analgesics such as opioids, usually in combination with over-the-counter medications and other NPIs to manage pain. This is consistent with chronic cancer pain sufferers, and clearly indicates the perceived value of adjunctive NPIs in chronic pain management [88,89,90].
The effectiveness of the NPIs varied markedly and were split between those finding the NPIs ineffective, and those finding them beneficial with some outliers at both ends of the continuum (Fig. 3). This would seem to reflect the highly personal, varied and idiosyncratic nature of chronic pain and highly variable inter-subject response to NPIs, and results being very dependent on the individual response to the applications used [17, 24, 91,92,93].
Despite the more immersive nature of the VR experiences, we found no statistically significant difference between the arms in daily VAS pre/during/post exposure pain score reduction. However, more participants had changes in pain scores exceeding the MCID (Table 2), and only during exposure pain reduction in the cognitive applications in the VR arm exceeded the MCID. The effects of cognitive applications in the control arm approached clinical significance (MCID) in the total sample. Whilst some recent studies have reported positive results in RCTs exploring VR as a NPI for chronic pain [21, 22, 26], reviews have also noted significant confounding factors such as underpowered sample size, dissimilar control treatments, lack of blinding, or significant risk of bias and some, as here, have also found inconclusive results [20, 25, 27, 44]. Additionally, although overall results in this study were negative, more focused specific pain VR applications could have different results. For example, tailored approaches that address changes in body perception and body representation in specific chronic pain situations might have more potential value. Custom-designed VR applications targeting specific psycho-biological factors in chronic pain scenarios such as phantom-limb pain have showed significant promise in this area [94, 95].
Intriguingly, the sub-group analysis of those with greater pre-exposure pain showed greater pain reductions (Table 4). Here, both control and VR arms demonstrated clinically meaningful pain reduction in most applications, and the cognitive applications provided greater pain reduction than the meditative counterparts within each arm during the therapy. However, in both full sample and sub-group analysis the immediate post-exposure mean scores for the meditative applications were better than those during exposure. In all but one instance (the OB application in the control sub-group analysis), a trend of the cognitive applications providing greater pain reduction during the experience, and meditative applications a greater post exposure pain reduction was evident. These findings suggest cognitive distractive VR applications may offer better pain reduction during the experience, and meditative experiences a slightly greater post-exposure effect. This supports the differences in the way these applications are theorized to act on the brain, in that cognitive applications provide distraction through focused engagement in problem solving, whilst mindfulness meditative applications stimulate activation of cortical and other regions offering a temporary altered state of mind [36, 40]. A related sub-group exploratory study of EEG changes during VR guided mindfulness meditation revealed some distinctive EEG characteristics, which would support this contention [37].
VR and control NPIs provided pain reduction effects post-exposure (Fig. 4), mostly for up to an hour afterwards, but for several hours for some. Both VR and control applications demonstrated this effect, however, it was unclear if meditative or cognitive applications offered superior effects, although the better post-exposure effects of the meditative applications might suggest they would perform better in this respect (Tables 3 and 4). A quarter of participants indicated they used less medication, which is of clinical interest, as all analgesics have adverse side-effects and reductions in analgesic use are associated with improvements in function [96]. Again, no significant difference was observed between groups, suggesting that VR NPIs may not offer an advantage in this respect.
In terms of any ongoing and cumulative effects, only the SF-MPQ and SF12 demonstrated any clinically meaningful changes and differences between groups from baseline (week 0 in Figs. 5 and 6). The SF-MPQ identified a clinically important change for the control group in the total score in Week 4 (also one approaching clinical significance in Week 2). In both the VR and control groups a reducing trend in total pain was evident (Fig. 5) and the control group decrease just surpassed the CIC threshold of > 5 at 5.44, SE1.03. The SF-12 did identify some between group effects in the PCS in Week 3 and the MCS in Week 2, but these demonstrated opposite effects with the VR being better in the PCS in week 3 and control for the MCS in week 2.
Overall, no distinct trends were apparent, as scores varied by week, and it is unlikely these findings reflect clinically meaningful changes due to NPI use during the trial. More likely, these reflect other changes in chronicity and pain of participants [97]. Overall, the SF-MPQ demonstrated a slight pain reduction in both arms over the period of the trial, whilst the SF-12 quality of life scores remained variable throughout the study. Although a significant difference in self-reported weekly pain and quality of life was seen between the VR and control group over the period of the study, this was inconclusive and in the case of the SF-MPQ, favoured the control. Definitive evidence for any progressive improvement in pain control, quality of life, or sleep over the trial was largely absent in either group.
In the immersion and presence survey, audio and video fidelity items were generally similarly scored, and there were no significant differences between audio, video fidelity, and presence scores between VR and control groups, except for the VMW, where the screen-based control version scored significantly better than the VR for visual fidelity. As a pilot version of the survey, these findings should be treated with caution. However, possibly, this may have been due to VR participants finding the trees and grass less realistic when looking peripherally, with those using the screen-based version looking around less. This may help explain why between-arm differences were generally not observed. The VR HMD displays offered stereoscopic views allowing the user to turn and look around, just as in the physical world with a resolution of 1080 × 1200 pixels per eye (2160 × 1200), compared to 1366 × 768 pixels of the computer screen. However, the pixels span a larger field of view in the HMD than the computer screen, providing approximately 11 pixels per degree, compared to 45 pixels per degree on the laptop. Low resolution can cause the pixels to become visible to the human eyes in VR HMDs because the user's eyes are positioned close to the display. For truly immersive Virtual Reality, 4 K resolution (3840 × 2160 pixels) or even 8 K resolution (7680 × 4320 pixels) per eye has been suggested as required by some VR developers [98]. Additionally, VR HMDs suffer from screen-door effect (a visual grid overlay artifact caused by viewing a screen close up where the spaces between pixels become visible) [99]. Both issues detract from perceptions of visual fidelity for VR applications.
In terms of acceptability, safety, and adverse events, VR appeared a safe and suitable NPI for home use, and transient cybersickness was the only significant adverse effect encountered across all the applications, and as might be expected was more evident in VR. In both VR meditative and cognitive applications participants reported more cybersickness as compared to the control participants (Supplemental Table 3). This was most evident in the applications that involved floating or flying along a path (WF and VMW) which are known to promote cybersickness in VR applications [76, 78]. Some VR applications, therefore, may not be suitable for those susceptible to motion sickness, and developers should be mindful of this when developing clinical applications. However, cancer patients are often prone to nausea, so other populations might tolerate this better. The only other adverse effects, reported were minor discomfort with using glasses in the HMD, or neck ache and/or eye ache after wearing the HMD for 30 min. These issues may be resolved with lighter HMDs in the future, although eye-ache with prolonged use may be more difficult to resolve with existing HMD screen technologies.
A significant complicating factor in this field is that the nature of chronic pain in cancer is widely heterogenous. In some cancer patients it may represent a form of chronic primary pain with significant emotional distress or functional disability in the absence of an acute medical condition, whilst other patients could be suffering from pain with ongoing active peripheral nociceptive stimulation as a result of tissue damage from cancer or its treatment.
Findings suggest that VR interventions may have a role to play in the management of chronic pain, together with demonstrating that cognitive distraction can provide significant pain reduction benefits for some. However, the hypothesis that VR applications offer superior pain-relief to equivalent less immersive screen-based media was not validated, and evidence for any progressive benefits weak. Largely, it would appear VR, provides some distractive pain relief, and offers an immersive way to engage in mindfulness meditation. Responses were not large and varied, and computer-based interactive multimedia applications seemed to provide similar (often superior) results to VR ones. Although VR cognitive NPIs demonstrated superior efficacy in pain reduction in some cognitive applications, their use might be more appropriately targeted in settings where short-term powerful distraction is more valuable. At this stage of the technology’s development, laptop-based interactive multimedia cognitive and meditative NPIs may also be sufficient for chronic pain applications in this domain and offer more cost-effective solutions and practicality for home use.
Limitations
There were a number of imitations in this in-vivo study. The external validity may be limited as the types of cancer patients participating and pain types were heterogenous, and participant self-selection may mean they were not representative of the larger population. The study may have been statistically underpowered because of the effect size selected, NPI exposure time, and multiple VR applications used as dependent variables. Additionally, all data was self-reported, and as it was not possible to use instruments during the VR experience without breaking the immersion, the during VR VAS pain scores were determined retrospectively immediately post-experience. Also, as many participants were using pain medication and/or other NPIs these may also have influenced the weekly trends. However, randomization should have helped mitigate such effects. The immersion tool used was in a pilot phase, as it has yet to be validated as a reliable instrument. Another limitation was that as a close-knit community, blinding may have been compromised by some VR and control arm participants comparing notes. However, as the work was largely explorative in nature, focused on comparing VR to screen-based media, and the fact that this population is very difficult to access for longitudinal studies, these limitations are considered acceptable. Finally, participants were randomized per treatment arm, and the study used a larger sample than many VR studies, multiple instruments and data collection points, and used blinding to enhance the robustness of the experimental design. This is argued a strength as the NPI physical intervention literature (and particularly VR work) has reported that chronic pain behavioural research is particularly vulnerable to bias in many of these respects [25, 100,101,102,103].
Future directions
The findings suggest several intriguing avenues for future research. The study needs to be replicated with more homogenous chronic pain populations, ideally with more patients and fewer dependent variables. Improved research methods to capture pain experiences during VR experiences are also needed. Exploration of creative designs for cognitive and meditative applications targeting chronic pain should also be undertaken to maximize their impact. Furthermore, the exploration of post-exposure effects of cognitive vs meditative applications would also be appropriate, as well as studies with lighter more comfortable HMDs with higher resolutions.
Conclusion
The use of VR-based chronic pain NPIs achieved some pain reduction effects beyond the MCID and CIC, but not dissimilar effects from their use on a typical 2D computer screen. No significant differences were identified between the reported pain experiences of participants during, or after daily exposure to VR immersive environments, overall and within four different VR immersive environments, compared to participants exposed to the equivalent applications experienced on 2D computer screens. Similarly, there were no statistically significant trends in weekly pain, quality of life, and sleep experiences reported by the VR participants compared to the screen-based control participants.
Cognitive VR applications appeared to offer some better during-exposure pain relief whilst meditative applications had superior post-exposure effects. Reported positive effects usually lasted less than an hour, but a small number of participants reported effects lasting 4 h or more. Transient cybersickness was the only significant adverse effect encountered.
Pain reduction responses with VR NPIs were varied, and at this stage of VR technological development, laptop-based interactive multimedia cognitive distractive and meditative NPIs may offer equivalent solutions that are practical for home use in chronic cancer-related pain settings.
Availability of data and materials
The deidentified data from this study is openly available from the Borealis data repository at: https://borealisdata.ca/dataset.xhtml?persistentId=doi:https://doi.org/10.5683/SP3/9MSN4Y.
Abbreviations
- 2D:
-
Two dimensional
- 3D:
-
Three dimensional
- CI:
-
Confidence interval
- CIC:
-
Clinically important change
- CL:
-
Carpe Lucem multimedia application
- ICC:
-
Interclass correlation
- IEQ:
-
Immersion Experience Questionnaire
- HMD:
-
Head mounted display
- MCS:
-
Mental component score—SF12
- MCID:
-
Minimum clinically important difference
- NPI:
-
Non-pharmacological intervention
- OB:
-
Obduction multimedia application
- PCS:
-
Physical component score—SF12
- PSQI:
-
Pittsburgh sleep quality index instrument
- RCT:
-
Randomized controlled trial
- SF-12:
-
Short form 12 instrument
- SF-MPQ:
-
Short form McGill pain quality instrument
- VR:
-
Virtual reality
- VAS:
-
Visual analogue scale instrument
- WF:
-
Wildflowers multimedia application
- VMW:
-
Virtual meditative multimedia application
References
Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “Silver Tsunami”: Prevalence Trajectories and Co-Morbidity Burden among Older Cancer Survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016;25:1029–36.
Miller KD, Nogueira L, Devasia T, Mariotto AB, Yabroff KR, Jemal A, et al. Cancer treatment and survivorship statistics, 2022. CA Cancer J Clin. 2022;72:409–36.
Gallaway MS. Pain Among Cancer Survivors. Prev Chronic Dis. 2020;17.
Levy MH, Chwistek M, Mehta RS. Management of chronic pain in cancer survivors. Cancer J Sudbury Mass. 2008;14:401–9.
Everdingen MHJ van den B, Hochstenbach LMJ, Joosten EAJ, Tjan-Heijnen VCG, Janssen DJA. Update on Prevalence of Pain in Patients With Cancer: Systematic Review and Meta-Analysis. J Pain Symptom Manage. 2016;51:1070–1090.e9.
Green CR, Hart-Johnson T, Loeffler DR. Cancer-related chronic pain: examining quality of life in diverse cancer survivors. Cancer. 2011;117:1994–2003.
Pachman DR, Barton DL, Swetz KM, Loprinzi CL. Troublesome symptoms in cancer survivors: fatigue, insomnia, neuropathy, and pain. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30:3687–96.
Shirvalkar P, Prosky J, Chin G, Ahmadipour P, Sani OG, Desai M, et al. First-in-human prediction of chronic pain state using intracranial neural biomarkers. Nat Neurosci. 2023;:1–10.
Zucca AC, Boyes AW, Linden W, Girgis A. All’s well that ends well? Quality of life and physical symptom clusters in long-term cancer survivors across cancer types. J Pain Symptom Manage. 2012;43:720–31.
Valeberg BT, Rustøen T, Bjordal K, Hanestad BR, Paul S, Miaskowski C. Self-reported prevalence, etiology, and characteristics of pain in oncology outpatients. Eur J Pain Lond Engl. 2008;12:582–90.
Bushnell MC, Frangos E, Madian N. Non-pharmacological Treatment of Pain: Grand Challenge and Future Opportunities. Front Pain Res. 2021;2.
Becker WC, Dorflinger L, Edmond SN, Islam L, Heapy AA, Fraenkel L. Barriers and facilitators to use of non-pharmacological treatments in chronic pain. BMC Fam Pract. 2017;18:41.
Hökkä M, Kaakinen P, Pölkki T. A systematic review: non-pharmacological interventions in treating pain in patients with advanced cancer. J Adv Nurs. 2014;70:1954–69.
Turk DC, McCarberg B. Non-Pharmacological Treatments for Chronic Pain. Dis Manag Health Outcomes. 2005;13:19–30.
Chau B, Ta P, Humbert S, Hata J, Tran D, Phelan I. Immersive virtual reality therapy with myoelectric control for treatment-resistant phantom limb pain: Case report. j. 2017;14.
Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M. A Rapid Evidence Assessment of Immersive Virtual Reality as an Adjunct Therapy in Acute Pain Management in Clinical Practice. Clin J Pain. 2014;30:1–26.
Gromala D, Song M, Yim J-D, Fox T, Barnes SJ, Nazemi M, et al. Immersive VR : A Non-pharmacological Analgesic for Chronic Pain ? Proc Annu Conf Hum Factors Comput Syst CHI. 2011;11:1171–6.
Hoffman HG, Chambers GT, Meyer WJ 3rd, Arceneaux LL, Russell WJ, Seibel EJ, et al. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Ann Behav Med Publ Soc Behav Med. 2011;41:183–91.
Ahmadpour N, Randall H, Choksi H, Gao A, Vaughan C, Poronnik P. Virtual Reality interventions for acute and chronic pain management. Int J Biochem Cell Biol. 2019;114:105568.
Chuan A, Zhou JJ, Hou RM, Stevens CJ, Bogdanovych A. Virtual reality for acute and chronic pain management in adult patients: a narrative review. Anaesthesia. 2021;76:695–704.
Darnall BD, Krishnamurthy P, Tsuei J, Minor JD. Self-Administered Skills-Based Virtual Reality Intervention for Chronic Pain: Randomized Controlled Pilot Study. JMIR Form Res. 2020;4:e17293.
Garcia LM, Birckhead BJ, Krishnamurthy P, Sackman J, Mackey IG, Louis RG, et al. An 8-Week Self-Administered At-Home Behavioral Skills-Based Virtual Reality Program for Chronic Low Back Pain: Double-Blind, Randomized, Placebo-Controlled Trial Conducted During COVID-19. J Med Internet Res. 2021;23:e26292.
Garrett B, Taverner T, McDade P. Virtual Reality as an Adjunct Home Therapy in Chronic Pain Management: An Exploratory Study. JMIR Med Inform. 2017;5:e11.
Goudman L, Jansen J, Billot M, Vets N, Smedt AD, Roulaud M, et al. Virtual Reality Applications in Chronic Pain Management: Systematic Review and Meta-analysis. JMIR Serious Games. 2022;10:e34402.
Grassini S. Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis. Int J Environ Res Public Health. 2022;19:4071.
Maddox T, Sparks C, Oldstone L, Maddox R, Ffrench K, Garcia H, et al. Durable chronic low back pain reductions up to 24 months after treatment for an accessible, 8-week, in-home behavioral skills–based virtual reality program: a randomized controlled trial. Pain Med. 2023;24:1200–3.
Wong KP, Tse MMY, Qin J. Effectiveness of Virtual Reality-Based Interventions for Managing Chronic Pain on Pain Reduction, Anxiety, Depression and Mood: A Systematic Review. Healthcare. 2022;10:2047.
Dahlquist LM, McKenna KD, Jones KK, Dillinger L, Weiss KE, Ackerman CS. Active and passive distraction using a head-mounted display helmet: Effects on cold pressor pain in children. Health Psychol. 2007;26:794–801.
Johnson MH. How does distraction work in the management of pain? Curr Pain Headache Rep. 2005;9:90–5.
Eccleston C. Chronic pain and distraction: an experimental investigation into the role of sustained and shifting attention in the processing of chronic persistent pain. Behav Res Ther. 1995;33:391–405.
Furman E, Jasinevicius TR, Nabil F, Victoroff KZ, Skillicorn R, Buchner M, et al. Virtual Reality Distraction for Pain Control During Periodontal Scaling and Root Planing Procedures. J Am Dent Assoc. 2013;140 JADA 2009;140(12):1508-1516:1508–16.
Schreiber KL, Campbell C, Martel MO, Greenbaum S, Wasan AD, Borsook D, et al. Distraction Analgesia in Chronic Pain Patients: The Impact of Catastrophizing. Anesthesiology. 2014;121:1292–301.
Garrett B, Taverner T, Gromala D, Tao G, Cordingley E, Sun C. Virtual Reality Clinical Research : Promises and Challenges. JIMR Serious Games. 2018;6:e10839.
Sharifpour S, Manshaee GR, Sajjadian I. Effects of virtual reality therapy on perceived pain intensity, anxiety, catastrophising and self-efficacy among adolescents with cancer. Couns Psychother Res. 2021;21:218–26.
Wickens CD. Multiple resources and mental workload. Hum Factors. 2008;50:449–55.
Day MA, Jensen MP, Ehde DM, Thorn BE. Toward a Theoretical Model for Mindfulness-Based Pain Management. J Pain. 2014;15:691–703.
Fu H, Garrett B, Tao G, Cordingley E, Ofoghi Z, Taverner T, et al. Virtual Reality Guided Meditation for Chronic Pain in Cancer Patients: An Exploratory Analysis of EEG Activity (Preprint). JMIR Biomed Eng. 2021;6:e26332.
Gromala D, Tong X, Choo A, Karamnejad M, Shaw CD. The Virtual Meditative Walk: Virtual Reality Therapy for Chronic Pain Management. Proc ACM CHI15 Conf Hum Factors Comput Syst. 2015;1.
Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KMG. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther. 2016;45:5–31.
Zeidan F, Baumgartner JN, Coghill RC. The neural mechanisms of mindfulness-based pain relief: a functional magnetic resonance imaging-based review and primer. PAIN Rep. 2019;4:e759.
Farias M, Wikholm C. Has the science of mindfulness lost its mind? BJPsych Bull. 2016;40:329–32.
Stetka B. Where’s the Proof That Mindfulness Meditation Works? Scientific American. https://www.scientificamerican.com/article/wheres-the-proof-that-mindfulness-meditation-works1/. Accessed 21 Mar 2023.
Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, et al. Mind the Hype: A Critical Evaluation and Prescriptive Agenda for Research on Mindfulness and Meditation. Perspect Psychol Sci. 2018;13:36–61.
Pittara M, Matsangidou M, Stylianides K, Petkov N, Pattichis CS. Virtual Reality for Pain Management in Cancer: A Comprehensive Review. IEEE Access. 2020;8:225475–89.
Violanti D, Mete M, Morris A, Groninger H. Virtual Reality for Pain Management in Inpatients with Cancer: A Randomized Controlled Trial (Sci259). J Pain Symptom Manage. 2023;65:e672.
Zeng Y, Zhang JE, Cheng ASK, Cheng H, Wefel JS. Meta-Analysis of the Efficacy of Virtual Reality–Based Interventions in Cancer-Related Symptom Management. Integr Cancer Ther. 2019;18.
Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the Clinical Importance of Treatment Outcomes in Chronic Pain Clinical Trials: IMMPACT Recommendations. J Pain. 2008;9:105–21.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009; 41:1149–1160.
Shahrbanian S, Ma X, Korner-Bitensky N, Simmonds MJ. Scientific evidence for the effectiveness of virtual reality for pain reduction in adults with acute or chronic pain. Stud Health Technol Inform. 2009;144:40–3.
Wiederhold BK. VR and Interactive Simulation for Pain Distraction: An Overview. Cybertherapy Rehabil. 2010;:12.
Delgado DA, Lambert BS, Boutris N, McCulloch PC, Robbins AB, Moreno MR, et al. Validation of Digital Visual Analog Scale Pain Scoring with a Traditional Paper-based Visual Analog Scale in Adults. J Am Acad Orthop Surg Glob Res Rev. 2018;2:e088.
Kremer E, Hampton AJ. Pain measurement: Construct validity of the affective dimension of the McGill Pain Questionnaire with chronic benign pain patients. Pain. 1981;11:93–100.
Bhandari NR, Kathe N, Hayes C, Payakachat N. Reliability and Validity of SF-12v2 Among Adults with Self-Reported Cancer. Res Soc Adm Pharm RSAP. 2018;14:1080–4.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37:378–81.
Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med Off J Soc Acad Emerg Med. 2001;8:1153–7.
Bird SB, Dickson EW. Clinically significant changes in pain along the visual analog scale. Ann Emerg Med. 2001;38:639–43.
Kelly A. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J EMJ. 2001;18:205–7.
Lee JS, Hobden E, Stiell IG, Wells GA. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med Off J Soc Acad Emerg Med. 2003;10:1128–30.
Dudgeon D, Raubertas RF, Rosenthal SN. The short-form McGill Pain Questionnaire in chronic cancer pain. J Pain Symptom Manage. 1993;8:191–5.
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011;63(Suppl 11):S240-252.
Huysmans E. Short-form McGill Pain Questionnaire. Physiopedia. 2022. https://www.physio-pedia.com/Short-form_McGill_Pain_Questionnaire. Accessed 6 Apr 2023.
Strand LI, Ljunggren AE, Bogen B, Ask T, Johnsen TB. The Short-Form McGill Pain Questionnaire as an outcome measure: test-retest reliability and responsiveness to change. Eur J Pain Lond Engl. 2008;12:917–25.
Clement ND, Weir D, Holland J, Gerrand C, Deehan DJ. Meaningful changes in the Short Form 12 physical and mental summary scores after total knee arthroplasty. Knee. 2019;26:861–8.
Díaz-Arribas MJ, Fernández-Serrano M, Royuela A, Kovacs FM, Gallego-Izquierdo T, Ramos-Sánchez M, et al. Minimal Clinically Important Difference in Quality of Life for Patients With Low Back Pain. Spine. 2017;42:1908–16.
Zhang C, Zhang H, Zhao M, Li Z, Cook CE, Buysse DJ, et al. Reliability, Validity, and Factor Structure of Pittsburgh Sleep Quality Index in Community-Based Centenarians. Front Psychiatry. 2020;11.
Beck SL, Schwartz AL, Towsley G, Dudley W, Barsevick A. Psychometric evaluation of the Pittsburgh Sleep Quality Index in cancer patients. J Pain Symptom Manage. 2004;27:140–8.
Longo UG, Berton A, De Salvatore S, Piergentili I, Casciani E, Faldetta A, et al. Minimal Clinically Important Difference and Patient Acceptable Symptom State for the Pittsburgh Sleep Quality Index in Patients Who Underwent Rotator Cuff Tear Repair. Int J Environ Res Public Health. 2021;18:8666.
Jacobs C, Rigby M. Developing measures of immersion and motivation for learning technologies in healthcare simulation: a pilot study. J Adv Med Educ Prof. 2022;10:163–71.
Jennett C, Cox AL, Cairns P, Dhoparee S, Epps A, Tijs T, et al. Measuring and defining the experience of immersion in games. Int J Hum-Comput Stud. 2008;66:641–61.
Skarbez R, Brooks, Jr. FP, Whitton MC. A Survey of Presence and Related Concepts. ACM Comput Surv. 2017;50:96:1–96:39.
Slater M, Lotto B, Arnold MM, Sanchez-vives MV. How we experience immersive virtual environments : the concept of presence and its measurement *. 2009;40:193–210.
Slater M, Wilbur S. A framework for immersive virtual environments (FIVE)... Presence Teleoperators Virtual Environ. 1997;6:603.
Rigby JM, Brumby DP, Gould SJJ, Cox AL. Development of a Questionnaire to Measure Immersion in Video Media: The Film IEQ. In: Proceedings of the 2019 ACM International Conference on Interactive Experiences for TV and Online Video. Salford (Manchester) United Kingdom: ACM; 2019. p. 35–46.
Bonato F, Bubka A, Palmisano S. Combined pitch and roll and cybersickness in a virtual environment. Aviat Space Environ Med. 2009;80:941–5.
Helin Kaj, D’Cruz Mirabelle, Valtion teknillinen tutkimuskeskus. HT, Qu C, Heynderickx I. Cybersickness and anxiety in virtual environments. In: VTT Symposium (Valtion Teknillinen Tutkimuskeskus). VTT; 2011. p. 115.
LaViola JJ. A discussion of cybersickness in virtual environments. ACM SIGCHI Bull. 2000;32:47–56.
Elkins G, Johnson A, Fisher W. Cognitive Hypnotherapy for Pain Management. Am J Clin Hypn. 2012;54:294–310.
Oneal BJ, Patterson DR, Soltani M, Teeley A, Jensen MP. Virtual Reality Hypnosis In The Treatment Of Chronic Neuropathic Pain: A Case Report. Int J Clin Exp Hypn. 2008;56:451–62.
Cole L. The Impact of Guided Imagery on Pain and Anxiety in Hospitalized Adults. Pain Manag Nurs. 2021;22:465–9.
Hussain N, Said ASA. Mindfulness-Based Meditation Versus Progressive Relaxation Meditation: Impact on Chronic Pain in Older Female Patients With Diabetic Neuropathy. J Evid-Based Integr Med. 2019;24:2515690X19876599.
Bates D, Mächler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using Lme4. J Stat Softw. 2015;17:1–48.
Searle SR, Speed FM, Milliken GA. Population Marginal Means in the Linear Model: An Alternative to Least Squares Means. Am Stat. 1980;34(4):216–21.
Halekoh U, UHøjsgaard S. A Kenward-Roger Approximation and Parametric Bootstrap Methods for Tests in Linear Mixed Models – The R Package pbkrtest. Journal of Statistical Software. 2014; 59(9): 1–32.
Public Health Agency of Canada. Canadian Cancer Statistics. 2022. https://www.canada.ca/en/public-health/services/chronic-diseases/cancer/canadian-cancer-statistics.html. Accessed 21 Apr 2023.
Juniper Research. Video Games: Industry Trends, Monetisation Strategies & Market Size 2020–2025. 2022.
Asthana R, Goodall S, Lau J, Zimmermann C, Diaz PL, Wan AB, et al. Framing of the opioid problem in cancer pain management in Canada. Curr Oncol. 2019;26:e410–3.
Schopflocher D, Taenzer P, Jovey R. The prevalence of chronic pain in Canada. Pain Res Manag. 2011;16:445–50.
Zajacova A, Lee J, Grol-Prokopczyk H. The Geography of Pain in the United States and Canada. J Pain. 2022;23:2155–66.
Crofford LJ. Chronic Pain: Where the Body Meets the Brain. Trans Am Clin Climatol Assoc. 2015;126:167–83.
Pitcher MH, Von Korff M, Bushnell MC, Porter L. Prevalence and Profile of High-Impact Chronic Pain in the United States. J Pain. 2019;20:146–60.
Svenaeus F. The phenomenology of chronic pain: embodiment and alienation. Cont Philos Rev. 2015;48:107–22.
Gupta A, Scott K, Dukewich M. Innovative Technology Using Virtual Reality in the Treatment of Pain: Does It Reduce Pain via Distraction, or Is There More to It? Pain Med. 2018;19:151–9.
Matamala-Gomez M, Donegan T, Bottiroli S, Sandrini G, Sanchez-Vives MV, Tassorelli C. Immersive Virtual Reality and Virtual Embodiment for Pain Relief. Frontiers in Human Neuroscience. 2019;13.
Guildford BJ, Daly-Eichenhardt A, Hill B, Sanderson K, McCracken LM. Analgesic reduction during an interdisciplinary pain management programme: treatment effects and processes of change. Br J Pain. 2018;12:72–86.
Jayasinghe UW, Proudfoot J, Barton CA, Amoroso C, Holton C, Davies GP, et al. Quality of life of Australian chronically-ill adults: patient and practice characteristics matter. Health Qual Life Outcomes. 2009;7:50.
Orland K. Virtual Perfection: Why 8K resolution per eye isn’t enough for perfect VR. Ars Technica. 2013. https://arstechnica.com/gaming/2013/09/virtual-perfection-why-8k-resolution-per-eye-isnt-enough-for-perfect-vr/. Accessed 20 Apr 2023.
Cho J, Kim Y, Jung SH, Shin H, Kim T. 78–4: Screen Door Effect Mitigation and Its Quantitative Evaluation in VR Display. SID Symp Dig Tech Pap. 2017;48:1154–6.
Deyo RA, Walsh NE, Schoenfeld LS, Ramamurthy S. Can trials of physical treatments be blinded? The example of transcutaneous electrical nerve stimulation for chronic pain. Am J Phys Med Rehabil. 1990;69:6–10.
Mallari B, Spaeth E, Goh H, Boyd B. Virtual reality as an analgesic for acute and chronic pain in adults: A systematic review and meta-analysis. j. 2019;12.
McQuay HJ, Moore RA, Eccleston C, Morley S, Williams AC. Systematic review of outpatient services for chronic pain control. Health Technol Assess Winch Engl. 1997;1:i–iv, 1–135.
Smith LA, Oldman AD, McQuay HJ, Moore RA. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain. 2000;86(1-2):119–32. https://doi.org/10.1016/s0304-3959(00)00234-7.
Acknowledgements
The authors acknowledge the supporting free use of the following commercial VR applications in this study: Mobio Interactive—Qualia Wildflowers (WF), Cyan Worlds—Obduction (OB), and Hammer Labs for Carpe Lucem (CL). These companies had no input into the design, recruitment, data collection analysis, or resulting publications from the study.
We acknowledge Dr. Diane Gromala, Dr. Christopher Shaw, and their graduate students at the Pain Studies Lab at Simon Fraser University for the development of Virtual Meditative Walk, one of the environments used in the study, and their continued support and collaboration throughout the project. We also acknowledge the support of Dr. Bechara Saab, at Mobio Interactive for the development and use of Qualia Wildflowers (WF), Cyan Worlds for Obduction (OB), and Hammer Labs for Carpe Lucem (CL) by supporting free use of their VR applications in the study. We thank Dr. Pippa Hawley and Dr. Gil Kimel for their support with participant recruitment at BC Cancer centres and at St John Hospice. Lastly, we want to thank all the participants in this research study for their time and effort, without whose participation this work would not have been possible.
Funding
The study was funded by a research grant from the Lotte and John Hecht Memorial Foundation (Grant ID: 4110). The funding source has no authority in the study design or execution or in this manuscript's preparation.
Author information
Authors and Affiliations
Contributions
B.G.: formulated the overarching research goals and aims, developed the methodology, analyzed study data, wrote the main manuscript text and provided overall oversight and leadership responsibility for the research activity planning and execution. G.T.: performed the experiments, collected the data, analyzed study data and wrote the main manuscript text. R.M.: analyzed study data, presented the published work, specifically visualization/ data presentation and wrote the main manuscript text. C.Sun.: performed the experiments, collected the data, coordinated research activity planning and execution, and wrote the main manuscript text. E.C.: performed the experiments, collected the data and wrote the main manuscript text. T.T.: formulated the overarching research goals and aims, developed the methodology and wrote the main manuscript text. C.Shaw.: formulated the overarching research goals and aims, developed the methodology and wrote the main manuscript text. D.G.: formulated the overarching research goals and aims, developed the methodology and wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial was approved by the University of British Columbia Clinical Research Ethics Board (Approval #: H16-01510), and all participants provided informed written consent. All procedures were followed in accordance with the relevant guidelines and regulations (E.g., Declaration of Helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper reports the results of a randomized controlled superiority trial examining the effects of a home-based adjunctive virtual reality (VR) non-pharmacological intervention (NPI) for chronic pain in cancer patients. This randomized controlled superiority trial explored the effects of a home-based adjunctive 3D VR NPI for chronic pain in cancer patients, compared to the same NPI experienced through a two-dimensional (2D) medium. N=110.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garrett, B., Tao, G., Taverner, T. et al. An exploratory randomized controlled trial of virtual reality as a non-pharmacological adjunctive intervention for adults with chronic cancer-related pain. BMC Digit Health 2, 28 (2024). https://doi.org/10.1186/s44247-024-00084-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44247-024-00084-x