Abstract
Background
Due to a multitude of factors, the onset of the COVID-19 pandemic resulted in a significant increase in mental health issues within society, including depression and anxiety. Due to the increased trend of mental health disorders in society, digital mental health therapies are more useful than ever. With the emergence of programs utilizing Internet Cognitive Behavioral Therapy (iCBT), mental health resources are easily accessible and can be widely implemented to those in need.
The aim of this study was to identify predictors for interest to participate in SilverCloud digital mental health therapy among individuals with mild to severe anxiety and/or depression based on preliminary findings from the COVIDsmart study.
Methods
COVIDSmart participants who had moderate to severe anxiety and/or depression based on the PHQ-9 and GAD-7 scores, and who consented to be contacted for future studies, were invited to complete a needs assessment survey via Research Electronic Data Capture (REDCap). This assessment used self-reported measures including medical diagnoses, mental health services received, reasons for anxiety and/or depression, the use of coping strategies, suicidal ideology using the Ask Suicide Questions tool, and whether they would be interested in receiving free digital mental therapy. Descriptive statistics were used to report participants’ demographics and a logistic regression was used to find predictors for interest in participation in SilverCloud. SAS 9.4 was used and p values < 0.05 were considered significant.
Results
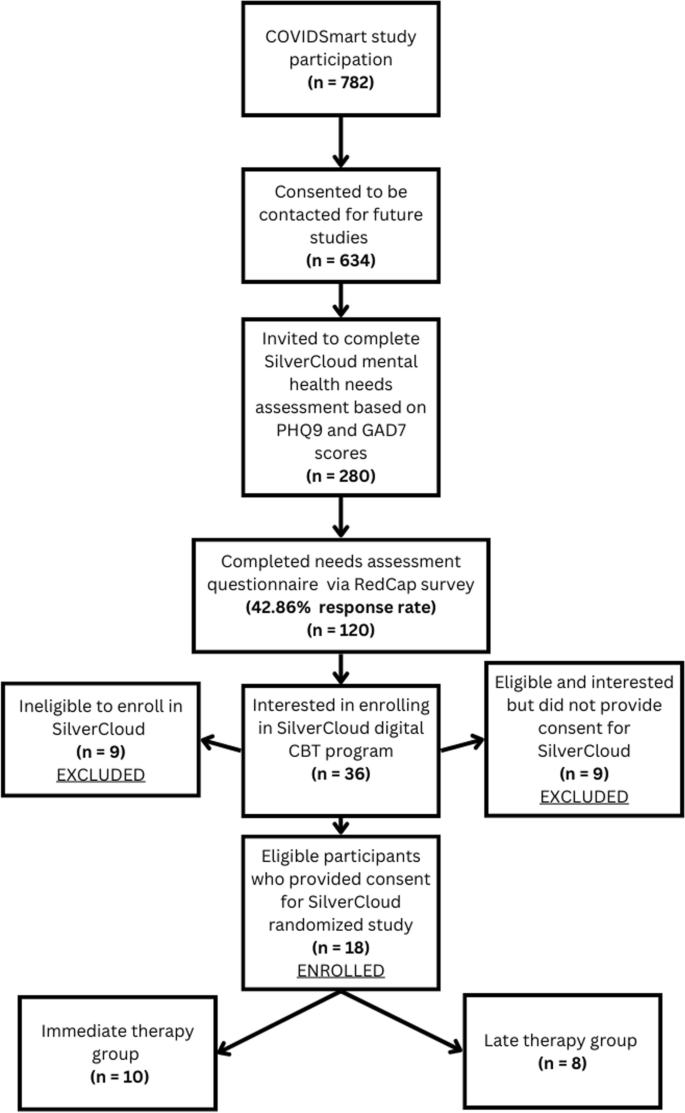
Out of the original 782 COVIDsmart participants, 634 consented to be contacted for future studies, 280 were subsequently invited to complete the SilverCloud needs assessment, and 120 individuals completed it. The largest demographic among these participants were females (70.83%) who identified as White (80.83%). The mean age was 48.74 years (SD = 14.66). Results revealed that having a mental health comorbidity significantly predicted the likelihood of interest in participating in the SilverCloud digital mental health program (p = 0.027).
Conclusions
In this study, mental illness comorbidities predicted the interest to participate in digital mental therapy. Fragmented healthcare and perceptions of unmet care needs are likely contributor factors. Further research with a diverse sample of participants is necessary for generalizability. Findings may have important implications for healthcare best practices.
Similar content being viewed by others
Introduction
Repeatedly, it has been evident that periods of widespread human catastrophe or disaster often result in large-scale detrimental impacts on mental health. During the COVID-19 pandemic, there were not only new cases of mental health disorders but also an exacerbation of existing mental health conditions [1]. According to a briefing released by the World Health Organization in March 2022, during the first year of the COVID-19 pandemic, the prevalence of major depressive disorders and anxiety disorders had increased significantly [2]. There were multiple factors leading to a significant spike in mental health disorders. Common stressors were social isolationism, perpetual fear of COVID-19 infection, loss of employment, death of a loved one or friend and uncertainty about the future [3]. Despite many of the COVID-19 restrictions and lockdowns being relaxed since March of 2020, the damaging adverse mental health effects of the pandemic seem to have persisted throughout the United States (U.S). According to a CDC report, the prevalence of anxiety and depressive disorders has been three and four times higher, respectively, compared to pre-pandemic levels within the U.S.[4]. In 2021, mental health screenings were taken by over 5.4 million people, indicating a near 500% increase since 2019 and a 103% increase since 2020 [5].
In the state of Virginia, the COVIDsmart study was initiated to assess the effects of COVID-19 on health, behavioral and economic status of individuals in Virginia. The study gathered data from March 2021 to November 2021 through longitudinal surveys. The surveys comprised the Patient Health Questionnaire-9 (PHQ-9), Generalized Anxiety Disorder-7 (GAD-7), a condensed version of the UCLA Loneliness Scale, and a condensed version of the Social Network Index [6]. 782 Virginia residents, spanning from 18 to 87 years, registered in the COVIDsmart study. The COVIDsmart sample consisted of mostly White (81.5%), middle aged (mean age 51), middle income (51% with income of $100,000 or higher), college educated (62.6%) females (78.6%) [6, 7]. The COVIDsmart preliminary results revealed that 21% of participants had moderate to severe anxiety and 25% had moderate to severe depression [7]. It was evident that there was a significant presence of mental disorders among Virginia residents after the COVID-19 pandemic. This prompted us to believe that there was a considerable number of individuals that required mental health services, but simply did not receive adequate counseling or therapy, leading to unmet health needs.
Based on these preliminary findings, a significant percentage of the participants of the COVIDsmart study had experienced some level of depression or anxiety, therefore the SilverCloud study was conceived and was funded by Eastern Virginia Medical School (EVMS) to alleviate the high rates of anxiety and depression among Virginians. Designed to alleviate depression and anxiety, SilverCloud is a digital mental health program that uses Internet Cognitive Behavioral Therapy (iCBT). CBT has been a highly effective form of psychological therapy for over 50 years. As patient requirements have increased, mental healthcare delivery has evolved significantly in the past decade with the introduction of new tools. Psychological interventions, specifically CBT, have become easier to implement in the form of iCBT [8]. The benefits of iCBT include cost effectiveness and global use [9]. Additionally, patients can utilize iCBT programs from the comfort of their homes, without the need for any in-person interaction. This can be particularly useful for those who have busy schedules or reside in more remote locations.
Although the mental health digital landscape is full of CBT-based apps and other digital interventions, meta-analyses and systematic reviews suggest that iCBT targeting anxiety and depression is not always effective. For example, a 2020 study by Etzelmueller et al., provided evidence for efficacy of iCBT interventions via randomized clinical trials [10] while Liu et al., 2022, suggested some iCBT-based modules are effective in treating anxiety and depression but other modules are not. Implementation science highlighting specialized needs, resources, and training to operate digital services is necessary for the success of digital therapeutics in healthcare [11]. SilverCloud Health has achieved global reach by using implementation science strategies and is the global leader in developing and delivering evidence-based mental health interventions across healthcare systems, payors such as insurance companies and government plans, providers, employer organizations, and charity/advocacy agencies [12]. SilverCloud delivers a vast array of personalized interventions to meet the specific mental health needs of individuals. Compared to other traditional digital platforms, SilverCloud offers self-guided programs, digital coaching, progress tracking tools and mobile accessibility in a secure environment. SilverCloud programs for anxiety and depression are recommended based on PHQ-9 and GAD-7 scores. These programs encourage the development of awareness and understanding of emotions, while increasing daily enjoyable activities and motivation. CBT is used to teach healthy thinking, feelings, behaviors, and to make positive changes to overcome anxiety and/or depression. SilverCloud programs include 10 modules: Getting Started, Understanding Depression and Anxiety, Noticing Feelings, Boosting Behavior, Spotting Thoughts, Challenging Thoughts, Managing Worry, Core Beliefs (unlockable by Coach), Facing Your Fears (unlockable by coach), and Bringing It All Together. SilverCloud coaches are licensed mental health professionals who provide weekly support to motivate users to engage in the SilverCloud programs, provide daily and weekly goals, and help users apply their learnings into everyday life [13]. The preliminary randomized controlled trials, which utilized SilverCloud, indicate that this therapy is effective as a stand-alone treatment for mild to moderate anxiety and depression [14].
The objective of this study was to determine the factors that can predict interest in participating in the SilverCloud program by COVIDsmart participants. Additionally, a secondary objective was to recognize the particular traits that enhance the probability of people seeking digital mental health care. This data could have significant clinical implications as it would enable healthcare professionals to gain better insights into the mental health needs of Virginians. With a greater understanding of the characteristics of these individuals in local communities, clinicians can customize digital interventions that cater to specific groups. This approach could enhance the rates of mental health screening and treatment accessibility among vulnerable populations, leading to better patient outcomes. Additionally, utilizing this information may enable digital mental health professionals to provide tailored and suitable treatment to their patients in the future. The implementation of these strategies could potentially have a notable effect in alleviating the continuous mental health emergency at a local, national, and conceivably worldwide scale.
Methods
Study design and recruitment
In order to conduct the SilverCloud study, the participants were recruited from the original COVIDSmart study. There were several recruitment strategies implemented in the COVIDSmart study, particularly to increase the likelihood of including ethnic minorities, individuals from rural areas, and individuals from lower socioeconomic backgrounds. The strategies implemented included online articles, employer e-newsletters, purchased email lists, social media posts, television, radio, paper flyers, and digital flyers. As an incentive, electronic gift cards were used to garner participation in the study. The data collection was conducted via an online HIPAA compliant platform designed by Vibrent Health Inc. The study was a joint effort with EVMS-Sentara Healthcare Analytics and Delivery Science Institute (HADSI), George Mason University, and Vibrent Health. 782 residents of Virginia enrolled in the COVIDSmart registry from March to May 2021.
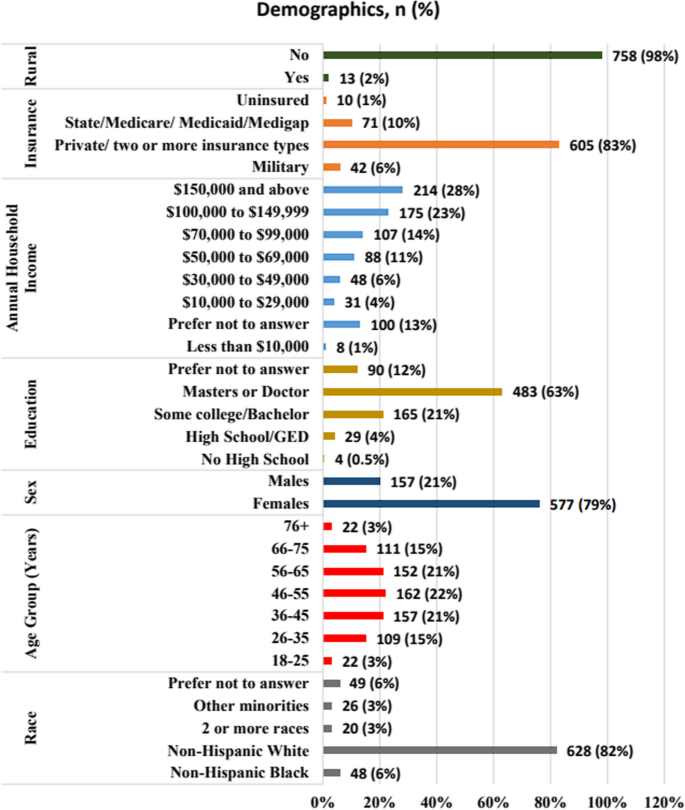
The SilverCloud study was created to address the COVIDSmart study’s preliminary results showing 21% of participants had moderate to severe anxiety and 25% had moderate to severe depression [15]. Figure 1 shows the demographics for COVIDSmart participants.
Out of the 782 original COVIDsmart participants, 634 of them consented to be contacted for future studies. 280 of the COVIDSmart participants who had moderate to severe anxiety and/or depression based on the PHQ-9 and GAD-7 scores, and who consented to be contacted for future studies, were invited to complete a needs assessment questionnaire to further determine eligibility to the SilverCloud study. 120 individuals completed the SilverCloud needs assessment. The needs assessment (Appendix 1) evaluated self-reported measures such as medical diagnoses, mental health services received, reasons for anxiety and/or depression, the use of coping strategies, suicidal ideology (using the Ask Suicide Questions (ASQ) survey), and whether they would be interested in receiving free digital mental therapy.
Thus, the purpose of this survey was twofold: to determine their eligibility for the 8-week SilverCloud study and to assess the factors contributing to their elevated levels of anxiety and/or depression during the COVID-19 pandemic (Fig. 2).
COVIDsmart participants who had an acute suicide screening based on the ASQ survey or self-reported substance abuse and dependence were not eligible to participate in SilverCloud. However, they were provided with a list of resources they could reach for immediate assistance (Appendix 2). This study was approved by the Eastern Virginia Medical School Institutional Review Board (IRB# 21–07-FB-0185).
Data collection
The SilverCloud needs assessment survey was created using Research Electronic Data Capture (REDCap). REDCap is a secure web-based application used to create forms and manage databases in order to support data capture and surveys for research. REDCap data is stored securely at EVMS on private, protected servers, and meets requirements for the Health Insurance Portability and Accountability Act for collection of personal health information. The needs assessment was sent via REDcap to identified potential participants.
Statistical analysis
Descriptive statistics were used to analyze the demographics of participants. To find predictors for interest to participate in SilverCloud, we used a logistic regression including the independent variables: receiving mental health care (yes or no), having coping strategies (yes or no), severity categories for GAD-7 and PHQ-9 (moderate to severe), mental illness comorbidity (yes or no), current medications for anxiety and/or depression (yes or no), race, sex, and age. The dependent variable was interest to enroll in SilverCloud (yes or no). We conducted the analysis using SAS 9.4, and p values < 0.05 were considered significant.
Results
A total of 120 participants who were part of the COVIDsmart program completed a needs assessment for SilverCloud. Table 1 shows that the majority of SilverCloud participants were female (70.83%) and White (80.83%). The mean age of participants was 48.74 years (SD = 14.66, Table 2).
The study found that having a co-existing mental health condition was a significant predictor of the likelihood of showing interest in participating in the digital mental health SilverCloud program (p = 0.027). Among participants with moderate to severe anxiety and/or depression who were enrolled in COVIDsmart, those with a comorbidity of mental illness were 378% more inclined to be interested in SilverCloud as compared to those without a mental illness comorbidity. The mental health comorbidities reported by SilverCloud participants had a wide range, but the most common comorbidity was Posttraumatic Stress Disorder (PTSD) (28.6%), followed by eating disorder (21.4%) and Attention Deficit Hyperactivity Disorder (ADHD) (14.3%), as presented in Table 3. These reported comorbidities were based off of self-reported survey data, and were not verified diagnoses.
However, factors such as race, gender, age, taking medication for anxiety or depression, anxiety severity, depression severity, use of coping strategies, and receiving mental health services did not have any predictive value in terms of interest in participating in SilverCloud (p ≥ 0.05), as shown in Table 4.
Discussion
Principle results
This study showed that the only significant factor that led COVIDsmart participants to be interested in participating in SilverCloud for depression and anxiety treatment was a mental illness comorbidity. The most common comorbidities reported included PTSD, eating disorders, and ADHD. Individuals with comorbid mental illnesses experience a cumulative medical burden, often requiring multiple physical and mental health services [15, 16]. These individuals are more likely to experience unintegrated and uncoordinated healthcare delivery [17, 18]. Furthermore, individuals with multiple mental health comorbidities are more likely to have perceived unmet needs for care [19, 20]. Thus, we hypothesize that individuals who experience fragmented healthcare and perceived unmet care needs may be more willing to accept mental health treatment for new conditions.
In addition, participants who had high levels of anxiety and/or depression, but no prior experience with mental health counseling, may be more apprehensive to receive treatment due to societal stigma about treatment for mental disorders. Participants with mental disorders with high levels of experienced stigma have lower rates of recovery since they are less likely to receive mental health services for their condition [21]. In this study, it seemed as if participants with multiple mental conditions were more likely to accept digital mental health treatment. The digital therapeutic setting may remove the stigma barrier for individuals with comorbid mental illnesses.
The PHQ-9 and GAD-7 scores did not have a significant predictive value for participating in mental health therapy. Unfortunately, it is unclear as to why this is. We hypothesize that since PHQ-9 and GAD-7 scores are only indicators for depression and anxiety alone, respectively, it is possible that despite a high level of depression and/or anxiety, the mental burden on these participants may not be as taxing as it is for participants with multiple mental health comorbidities, therefore, these participants were less likely to enroll in digital mental health therapy compared to participants with multiple comorbid mental illness. The individuals who chose to enroll in digital mental therapy may require integrated healthcare approaches to address their physical/mental multi-comorbidity healthcare needs. Additionally, participants who were already receiving mental health care services as well as those who were using coping strategies such as exercising and drinking less alcohol, were not likely to be interested in digital mental therapy.
The majority of participants in the COVIDsmart study were Non-Hispanic Whites and females, which explains why a similar demographic makeup was observed in the SilverCloud study. However, the SilverCloud study had a slightly higher percentage of female and Non-Hispanic White participants compared to the COVIDsmart study. Additionally, the greatest percentage of COVIDsmart participants fell into the 46–55 age range (Fig. 1). This corresponds accordingly with the mean age of SilverCloud participants being 48.74 years old (Table 2). Despite this, neither race nor gender nor age were significant predictors of participation in digital mental health therapy. It is not clear why these particular demographics were more likely to participate in both studies. Non-Hispanic Whites are known to have higher rates of mental disorders compared to people of color, although this may be due to various factors such as discriminatory medical practices, negative cultural attitudes towards mental illness, lack of insurance, and language barriers that minorities face [22, 23].
Future directions
Our findings suggest healthcare workers should especially turn their attention towards individuals who are already suffering from coexisting mental conditions. It is very possible that the introduction of future large-scale stressors can result in new cases or the exacerbation of milder forms of depression and anxiety in these patients. Mental health counselors, psychiatrists, and therapists should regularly screen patients with existing mental health conditions with the PHQ-9 and GAD-7 for any new developments regarding depression and anxiety. Moreover, future research is needed to further evaluate the role of healthcare fragmentation and perceptions of unmet medical care needs in the enrollment of digital mental therapies. Findings could have important implications for healthcare best practices.
Future research should expand the scope and demographics of this study. While the cause of the increase in the percentage of highly-educated female and Non-Hispanic White participants in the SilverCloud study remains unknown, it is important to consider this metric on a global scale. Large nationally representative US surveys have found that mental health of Black, Hispanic, and Asian respondents worsened relative to White respondents during the pandemic, including significant increases in depression and anxiety among racialized minorities compared to White people [24]. These surveys also showed that White respondents were the most likely to receive professional mental health care before and during the pandemic, while minority respondents demonstrated higher levels of unmet mental health care needs during the pandemic than White respondents [24]. The findings of our study showed a similar trend, wherein there was an increase in the number of White participants seeking mental health care. Although our study was limited in size compared to a nationwide study, the outcomes are comparable. Securing a diverse socio-economic and racial participation is important for generalizability of future studies.
Limitations
The study has several limitations. Firstly, it only included participants from the COVIDsmart study, which means that the sample was restricted to residents of Virginia. Secondly, research fatigue from the six-month longitudinal COVIDsmart study could have deterred some participants from taking part in the SilverCloud study, thus resulting in a smaller sample size. Thirdly, the socioeconomic and racial diversity of the SilverCloud study participants did not accurately reflect the Virginia population, as there was an overrepresentation of highly educated White females and an underrepresentation of minority groups, including those living in rural areas. The lack of participant diversity and limited scope of this study may significantly hamper its generalizability to broader populations.
Fourthly, because the SilverCloud program was only accessible online, participants without internet access in Virginia may have been less likely to participate. In the future, alternative treatment options such as traditional in-person face-to-face therapy could be considered, although this would require additional resources and higher costs. Fifth, the mental illness comorbidity was self-reported. We included the variable comorbidity (yes or no) in the logistic regression model to determine whether having a mental illness comorbidity would influence the outcome: interest to participate in SilverCloud. Sixth, high risk respondents to the needs assessment could only be provided with available resources to receive help, rather than being provided with an on demand consultation with an available clinician.
Conclusions
Individuals with mental illness comorbidities may have a higher tendency to seek and participate in digital mental health programs amid the COVID-19 pandemic. Digital CBT-based programs can potentially improve the accessibility of care for this group. However, programs should prepare to address the needs of patients with mental illness comorbidities as they may require multidisciplinary healthcare services. Mental health professionals and researchers need to gain a deeper understanding of the unique needs of this population.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- ADHD:
-
Attention Deficit Hyperactive Disorder
- EVMS:
-
Eastern Virginia Medical School
- iCBT:
-
Internet cognitive behavioral therapy
- PTSD:
-
Posttraumatic Stress Disorder
- REDCap:
-
Research Electronic Data Capture
References
Jones EAK, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. 2021;18(5):2470. https://doi.org/10.3390/ijerph18052470. PMID: 33802278; PMCID: PMC7967607.
World Health Organization. Covid-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization. 2022. Retrieved February 1, 2023, from https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
Panchal N, Kamal R, Cox C, & Garfield R. The implications of COVID-19 for mental health and substance use. KFF. 2021. Retrieved February 3, 2023, from https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–57. https://doi.org/10.15585/mmwr.mm6932a1.
Mental health and covid-19: Two years after the pandemic, mental health concerns continue to increase. Mental Health America. (n.d.). Retrieved February 3, 2023, from https://mhanational.org/mental-health-and-covid-19-two-years-after-pandemic
Bartholmae MM, Roess AA, Renshaw KD, Levy BL, Karpov MV, Sill JM, Dodani S. Evaluation of recruitment strategies on inclusiveness of populations at risk for health disparities in the statewide remote online COVID smart registry. Virginia J Publ Health. 2022;7(1):11–45 (https://commons.lib.jmu.edu/vjph/vol7/iss1/5/).
Schilling J, Klein D, Bartholmae MM, et al. COVID smart: A digital health initiative for remote data collection and study of COVID’s impact on the state of Virginia. J Med Internet Res. 2023. https://doi.org/10.2196/37550.
Karyotaki E, et al. Internet-based cognitive behavioral therapy for depression: a systematic review and individual patient data network meta-analysis. JAMA Psychiat. 2021;78(4):361–71. https://doi.org/10.1001/jamapsychiatry.2020.4364. PMID: 33471111; PMCID: PMC8027916.
Kumar V, Sattar Y, Bseiso A, Khan S, Rutkofsky IH. The effectiveness of internet-based cognitive behavioral therapy in treatment of psychiatric disorders. Cureus. 2017;9(8):e1626. https://doi.org/10.7759/cureus.1626. PMID: 29098136; PMCID: PMC5659300.
Etzelmueller A, Vis C, Karyotaki E, Baumeister H, Titov N, Berking M, Cuijpers P, Riper H, & Ebert DD. Effects of internet-based cognitive behavioral therapy in routine care for adults in treatment for depression and anxiety: Systematic review and meta-analysis. Med Inter Res 2020;22(8). https://doi.org/10.2196/18100
Liu T, Xu J, Cheng H, Zhang Y, Wang S, Lin L, Tian L. Effects of internet-based cognitive behavioral therapy on anxiety and depression symptoms in cancer patients: a meta-analysis. Gen Hosp Psychiatry. 2022;79:135–45. https://doi.org/10.1016/j.genhosppsych.2022.09.003.
Richards D, Enrique A, Palacios J, et al. SilverCloud health: online mental health and wellbeing platform. In: Sverdlov O, van Dam J, eds. Digital Therapeutics Strategic, Scientific, Developmental, and Regulatory Aspects. 1st ed. CRS Press. 2022; 307–329. https://doi.org/10.1201/9781003017288-15
SilverCloud Program Guide. Anxiety depression, and co-morbid anxiety & depression. (n. d.). Retrieved June 22, 2023, from https://www.silvercloudhealth.com/programs/mental-health-wellbeing
Richards D, Enrique A, Eilert N, Franklin M, Palacios J, Duffy D, Earley C, Chapman J, Jell G, Sollesse S, Timulak L. Author correction: A pragmatic randomized waitlist-controlled effectiveness and cost-effectiveness trial of digital interventions for depression and anxiety. Npj Digit Med 2020;3(1). https://doi.org/10.1038/s41746-020-0298-3
Bartholmae MM, Karpov Sill JM, Karpov MV, Sunita D. The association between depression, anxiety, and COVID-19 symptoms. J Mental Health Clin Psychol. 2023;7(2):1–8. https://doi.org/10.29245/2578-2959/2023/2.1277.
Doherty AM, Gaughran F. The interface of physical and mental health. Soc Psychiatry Psychiatr Epidemiol. 2014;49(5):673–82. https://doi.org/10.1007/s00127-014-0847-7.
Pizzol D, Trott M, Butler L, et al. Relationship between severe mental illness and physical multimorbidity: a meta-analysis and call for action. BMJ Ment Health. 2023;26:e300870. Retrieved from: https://mentalhealth.bmj.com/content/26/1/e300870.
Walker ER, Druss BG. Cumulative burden of comorbid mental disorders, substance use disorders, chronic medical conditions, and poverty on health among adults in the USA. Psychol Health Med. 2017;22(6):727–35. https://doi.org/10.1080/13548506.2016.1227855 Epub 2016 Sep 3. PMID: 27593083; PMCID: PMC5564203. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5564203/.
Forman-Hoffman VL, Batts KR, Hedden SL, Spagnola K, Bose J. Comorbid mental disorders among adults in the mental health surveillance survey. Ann Epidemiol. 2018;28(7):468–74. Retrieved from: https://www.sciencedirect.com/science/article/pii/S104727971730889X.
Chen L-Y, Crum RM, Martins SS, Kaufmann CN, Strain EC, Mojtabai R. Service use and barriers to mental health care among adults with major depression and comorbid substance dependence. Psychiatric Services. 2013;64(9):863–70. Retrieved fromhttps://ps.psychiatryonline.org/doi/10.1176/appi.ps.201200289.
Oexle N, Müller M, Kawohl W, Xu Z, Viering S, Wyss C, Vetter S, Rüsch N. Self-stigma as a barrier to recovery: A longitudinal study. Eur Arch Psychiatry Clin Neurosci. 2017;268(2):209–12. https://doi.org/10.1007/s00406-017-0773-2.
Panchal N, Saunders H, & Ndugga N. Five key findings on Mental Health and Substance Use Disorders by race/ethnicity. KFF. 2022. Retrieved March 5, 2023, from https://www.kff.org/racial-equity-and-health-policy/issue-brief/five-key-findings-on-mental-health-and-substance-use-disorders-by-race-ethnicity/#:~:text=Overall%20rates%20of%20mental%20illness,to%20accessing%20mental%20health%20care.
Racial disparities in mental health treatment. SC-UMT. 2021. Retrieved March 5, 2023, from https://online.simmons.edu/blog/racial-disparities-in-mental-health-treatment/
Thomeer MB, Moody MD, Yahirun J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J Racial Ethn Health Disparities. 2022:1–16. https://doi.org/10.1007/s40615-022-01284-9. Epub ahead of print. PMID: 35318615; PMCID: PMC8939391.
Acknowledgements
We thank all of the participants who took part in the SilverCloud study. A preprint version of this manuscript has been published in JMIR Publications and is provided as #15 in the list of references.
Funding
SilverCloud did not provide any funding for this project. All funding was provided internally by Eastern Virginia Medical School.
Author information
Authors and Affiliations
Contributions
MB, MK, and SD contributed to the study design, data collection, and data analysis. TG, RD, KA, AR, MK, MB, MK, and SD wrote and revised the main manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the ethical principles laid out in the Declaration of Helsinki. The participants gave informed consent to participate in the study. The study protocol was approved by the Eastern Virginia Medical School institutional review board (IRB# 21–07-FB-0185) and was conducted in compliance with all applicable laws and regulations.
Consent for publication
Not applicable.
Competing interests
None declared.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gunawardena, T., Bartholmae, M.M., Karpov, M.V. et al. Predictors for interest to participate in digital mental health therapy: a cross-sectional survey of individuals with anxiety and depression. BMC Digit Health 2, 21 (2024). https://doi.org/10.1186/s44247-024-00080-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44247-024-00080-1