Abstract
Background
Since 2020, physicians in Germany have the possibility of prescribing approved digital health applications (DHAs) with the costs covered by the health system – a step that was unique in the world at that time and still is. So far, there have been hardly any studies that shed light on the possible applications of DHAs in the context of primary care and take stock of the benefits and potential for optimization. In 2022, a quantitative survey was carried out. The aim was to determine what attitudes, experiences and expectations GPs have with regard to the use of DHAs, under what conditions they are willing to integrate them into health care, and what experience they have already gained.
Methods
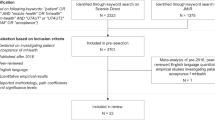
The focus was on a large-scale survey of GPs. Between spring and summer 2022, all 18,914 GPs in the federal states of Baden-Württemberg, Hesse, Lower Saxony, Rhineland-Palatinate and Saarland were invited to an online survey. 5,868 questionnaires were included in the evaluation (response rate: 31%). A t-test on independent samples was used to determine significant differences between two groups.
Results
68% of those surveyed are positive about DHAs and consider them to be reliable (69%) and safe (63%) applications that can generate efficiency benefits for the doctor-patient relationship. 24% trust themselves to competently advise patients on DHAs. 14% have already prescribed DHAs, 13% plan to do so. 85% of doctors with DHA experience rate the prescribed applications as (very) useful. Observed health care effects relate primarily to the improvement in compliance (94%), mobility (93%), and education (93%), as well as weight reduction (83%). Among other things, a further optimization of usability (59%), systematic further training of doctors on DHAs (53%) and the expansion of gamification elements (49%) are suggested. GPs lack well-founded information with regard to DHAs (52%).
Conclusion
For GPs, DHAs can be effective tools to encourage patients in their personal responsibility, compliance and motivation to behave in a health-conscious manner and to strengthen prevention in the primary care setting. Where DHAs have been used in a practical context so far, widespread positive health care effects are noticeable. Most respondents do not dare to give patients competent advice on available applications. Comprehensive training courses that provide information about the framework conditions, strategies and advantages of using DHAs appear to be important. There is also a need for more well-founded sources of information and research for doctors to select suitable applications in a targeted manner. GPs see significant added value in DHAs compared to conventional health apps. In order for DHAs to be effectively implemented in primary care, it is important to better inform GPs about the legal basis and possible applications as well as to address their concerns.
Similar content being viewed by others
Background
Germany has seen high-quality approved digital health applications (DHAs) integrated into standard care since 2020 by law (Digitalization and Innovation Act, DVG) – a step that was unique in the world at that time and still is [1]. Doctors have been able to prescribe DHAs to patients with statutory health insurance ever since. DHAs are apps covered by the country’s statutory health insurance and aimed at helping detect diseases more effectively, manage treatment and/or contribute to prevention [2,3,4,5]. Like conventional, freely available health apps, the purpose of DHAs is to reinforce empowerment, motivation, and compliance while also keeping patients informed and encouraging a healthy lifestyle [6, 7]. Unlike conventional health apps, DHAs are classified and certified as low-risk medical devices [8].
A health app needs to be listed in the DHA directory maintained by the Federal Institute for Drugs and Medical Devices (BfArM) to be classified as a DHA covered by statutory health insurance [9]. This requires DHA manufacturers to submit an application for approval and fulfil various requirements in a methodical evaluation process. Apart from CE certification as a medical product, DHAs also need to comply with standards on data privacy and information security, medical content quality, user-friendliness, robustness, and patient safety. The application’s benefits and added value (clinical benefit) need to be documented [10]. DHA directory listing and prescription are possible once all these criteria have been met. Apps that only meet general requirements initially may be granted temporary inclusion in what is referred to as a fast-track procedure. In these cases, manufacturers are given a period of grace to document the app’s clinical benefits in a one-year testing phase [2, 3, 8]. Various categories apply to clinical benefits such as pain reduction, increased awareness, and disease management. DHAs should be designed to be used by patients on their own or together with their doctors [2, 3, 7].
Favorably evaluated apps are now available for increasing numbers of clinical conditions including migraine, tinnitus, obesity, diabetes, sleep disorders, and mental illnesses. Lifestyle-associated applications are relatively well-represented in the forty-five DHAs currently listed by BfArM. Studies have shown that health apps can have positive effects on diseases such as obesity and type 2 diabetes mellitus by encouraging changes in patient behavior towards regulating everyday activities such as diet and exercise [11,12,13,14,15].
Like health apps, DHAs are mainly associated with their potential for assisting patients in empowerment, intrinsic motivation, and compliance in coping with disease. Patient information improves with educational content, and reminder features help towards health-promoting behavior [2, 3, 7, 8]. Ideally, apps will make it easier to identify disease risk earlier, document medical issues and symptoms, and increase effectiveness in doctor-patient relationships [16].
General practitioners will play a key role as primary care providers (PCPs) in successfully establishing DHAs in the healthcare system [17, 18]. This raises the possibility of general practitioners using DHAs specifically to promote health such as in cardiovascular risk prevention, support the process of application, and collect health data from patients on a regular basis [19,20,21,22,23]. Expert reports have highlighted the benefits of health apps towards optimizing differential diagnosis, disease management, and adherence to treatment [2, 8, 11, 12, 24].
Surveys have shown reticence among primary care physicians in recommending health apps and integrating them into their care, although PCPs have identified their potential benefit including reinforcing personal responsibility, education, and doctor-patient networking [17, 21, 25, 26]. This reticence corresponds to a distinct uncertainty regarding reliability and security – data privacy, practical readiness, suitability for certain patient groups, lack of legal certainty in app use on doctor’s instructions, and integration into everyday care [21, 23, 27]. The DHA concept covers these concerns. Most doctors express a poor level of information and difficulties in selecting suitable health apps given the plethora of packages available on the market [28].
There has also been a lack of reliable studies to elucidate possible applications for DHAs in primary care. This study provides an interim assessment from a general medical perspective since the establishment of these mHealth tools in the German healthcare system back in 2020. This includes factors such as level of knowledge, attitudes (acceptance, opportunities and risks, application potential by area), expectations, willingness to use, and previous experience among PCPs using DHAs. The study also set out to determine the extent to which GPs see added value in DHAs compared to classic health apps. The aim is to draw conclusions from the results as to the conditions that would favor harnessing the potential of DHAs in healthcare, especially primary care.
Materials and methods
This exploratory study collected detailed opinions and experiential accounts from GPs with a view to addressing the subject of this research project. We performed a full survey of GPs in five German states between spring and summer 2022. This was designed as an online survey with a written cover letter sent in the regular mail.
The quantitative large-scale survey of GPs mainly served as a central starting point for a qualitative interview study, which was carried out a few months later and focused exclusively on GPs with DHA experience (96 interviewees). The results of this qualitative study have already been published [29].
Questionnaire
The questionnaire was designed for this study. Individual questions were developed with the help several quantitative and qualitative preliminary studies by the authors, which examined various areas of focus on possible uses of health apps in primary care and specialist settings [21, 23, 28, 29]. In addition, a general literature research [such as 7, 11, 12, 16, 19, 25–31] ensured that—beyond the previous knowledge mentioned—no essential aspects in the topic context were ignored.
The final questionnaire (see Appendix 1) consisted of twenty-seven questions with five main areas of focus:
-
Awareness and general assessment of the DHA concept: This includes questions 1–4. The aim was to record the extent to which the respondents were familiar with the DHA concept, on which the Digitalization and Innovation Act is based. It is also determined how the respondents generally feel about the concept, without their attitudes being asked in detail. These questions have been newly developed. The information base on which the questions are based comes, among other things, from dealing with the official information sources and reports of the Federal Joint Committee and scientific articles on the possibilities of using DHA in the healthcare system [1, 2, 7, 9,10,11, 16, 30].
-
Attitudes and perceived potential use of DHAs in healthcare: This includes questions 5–8. The initial aim was to record the potential uses of DHAs and their benefits from the perspective of the respondents. Among other things, a differentiation was made according to general areas of application and various positive and negative statements were asked. In question 6, the classification scheme was used from a previous meta-study by Albrecht et al. [12]. The item list in question 7 was the result of an independent qualitative preliminary study [23].
-
Prerequisites and requirements for a (stronger) DHA application in practice operations: This includes questions 15, 16, 18–27. On the one hand, this section was about recording the conditions under which there is a willingness to use DHAs in practice or, after certain improvements, to use them more often than before. On the other hand, the status quo and the circumstances in everyday practice were determined. This made it possible to obtain information about the extent to which there is potential for DHA use in general practice settings (e.g. when interacting with patients). These questions have been newly developed.
-
Willingness and experience in using DHAs: This includes questions 9–17. This section was specifically about the use of DHAs in patient care (e.g. by recommending or prescribing certain applications to patients), experiences made so far and observed effects, differentiated according to general areas of application. The item battery in question 14 (positive effects on health) was developed with the help of other studies that have compiled possible effects of DHAs [4, 12, 16]. The findings from our own preliminary study were also included, which specifically looked at effects from the perspective of diabetological doctors [28].
The survey included several open questions (13, 15, 18, and 24) in addition to the standardized questions.
Ordinal scales came into wide use to achieve a good compromise between data quality and intuitive answerability in the survey for GPs as a target group with limited time to spare. Most of these ordinal scales had four options; some exceptions (questions 6, 12, and 17) combined the two negative answer options as this seemed reasonable. We deliberately avoided using a neutral middle category in the classification to make trends in attitudes and assessments regarding DHAs as clear as possible, so avoiding ticking middle categories as a non-response seemed to be the most beneficial way of ensuring this clarity. On the other hand, we used additional answer options for various knowledge and assessment questions such that respondents had the option of checking a box expressing difficulty in making an assessment.
The sociodemographic characteristics recorded were gender, age, practice setting, type of practice, and patients per quarter. We performed a pretest before field use; this involved presenting the questionnaire to fifty randomly selected GPs. The pretest showed answer categories to be easy to understand, well structured, and complete. Two item batteries had smaller item additions added (questions 7 and 14).
Recruitment and implementation
All 18,914 GPs practicing in Baden-Württemberg (6,664), Hesse (3,839), Lower Saxony (5,001), Rhineland-Palatinate (2,667), and Saarland (743) were sent written postal invitations to take part in an anonymized survey; the invitation period lasted between March and June 2022. This was a one-off mailshot where potential respondents were informed of password-protected access to the online survey (no incentives), inter alia.
The analysis included 5,868 completed questionnaires among the 5,903 processed (return rate: 31%).
Data analysis
We used SPSS 23.0 for data analysis. Student’s t-test for independent samples was used to determine significant differences between two groups. The practice setting was one of the parameters used for group comparison, distinguishing between the large and medium-sized city and small town and rural area categories. A distinction was also drawn between respondents above and below average age.
We also performed a factor analysis (Varimax rotation). Factor analysis serves to combine a larger number of variables into factors based on internal correlations. The aim of this is to reveal common underlying factors. The Varimax method that we selected is the most common method for arriving at interpretable factor solutions. We selected a 0.4/-0.4 limit value for factor loadings [31]. The Bartlett sphericity test was performed to test for the requirements of factor analysis. This tests the hypothesis that all correlation coefficients in the population have a zero value. A significant result allows the interpretation that at least some variables correlate within the population; the null hypothesis can be rejected.
We evaluated the open questions using post-coding for qualitative content analysis. This involved creating a basic category system for answers in free text to each open question [32]. STROBE was used as the reporting statement.
Results
Sample overview
Table 1 compares the sample from the quantitative survey and representative data from the German National Association of Statutory Health Insurance Physicians (Kassenärztliche Bundesvereinigung) on general practice distribution in Germany. The sample approximates to the representative distribution in major parameters, as the figures show.
A) Awareness and general assessment of the DHA concept
At the time of the survey, 88% of those surveyed were aware of the option to prescribe digital health applications. Ninety-six percent of doctors based in large and medium-sized cities had been informed about DHAs compared to 70% in small towns and rural communities (p < 0.001). Sixty-eight percent of respondents were generally positive about DHAs compared to 15% being more skeptical; 17% were undecided. Doctors in urban settings expressed a substantially more favorable view of apps compared to their colleagues in rural areas (92% vs. 29%, p < 0.001). Similarly, respondents below average age rated these applications more favorably than those above by a clear margin (86% vs. 48%, p < 0.001).
Of those surveyed, 69% expressed general trust in the BfArM evaluation process for approving DHAs and expected applications listed as DHAs to be reliable. A far higher percentage of urban doctors expressed confidence in the DHA directory than did rural doctors at 92% vs. 30% (p < 0.001). Just under a third of all respondents at 63% saw sufficient legal certainty, such as in issues of risks and liability, for doctors prescribing DHAs and their use in the practice.
Just over a quarter of those surveyed at 28% expected DHAs to make a very or moderately large contribution to health promotion, while 62% considered a contribution to exist but rather small; 10% saw no contribution at all. A higher percentage of urban doctors expected a large contribution from DHAs compared to rural doctors at 38% vs. 9% (p < 0.001). Of all the respondents, 58% expected DHAs to advance healthcare and medical practice digitalization in a positive and meaningful way; 16% did not expect such an effect and 26% found it difficult to say.
B) Attitudes and benefit potential in using DHAs
Perceived benefits of DHAs varied depending on field of application. Most at 88% thought it made sense if the apps helped manage medications or medical appointments. Just over three-quarters at 77% took a favorable view of the support they provided in self-monitoring for risk factors such as weight, blood pressure, and blood sugar, or weight data for parameters such as steps taken, water intake and similar. Just under three-quarters at 74% spoke in favor of using DHAs in physical exercise regimes followed by features to help patients keep to a healthy lifestyle such as diet and quitting smoking at 72%. A little over half at 54% saw DHAs as well suited for monitoring and treatment support.
More than half of the respondents at 56% saw no issues in physicians relying on data from DHAs in planning treatment for patients, whereas 29% rejected the idea and 15% found it difficult to say. Nearly three-quarters at 71% of the respondents who had no issues with doctors using DHA data in planning treatment also saw these applications as beneficial in supporting disease management and treatment.
Respondents associated DHAs with opportunities and risks (see Table 2). Increases in motivation and compliance were considered to be a significant benefit. The empowerment reinforcement component was also considered important. However, some of the respondents also expressed concerns about lack of data privacy and fear of undesirable consequences such as measurement errors due to lack of suitability for certain patient groups.
Factor analysis combining variables into factors based on underlying relationships as correlations [25]. revealed three distinct clusters of GPs. The correlating variables in the first group were perceived benefits of DHAs in health promotion, compliance, and motivation. The second group mainly focused on effectiveness and efficiency as benefits in the doctor-patient networking. The respondents also expressed awareness of the dangers in overusing and applying incorrect treatment as a result of using the app. The third cluster correlated on negative attitudes towards data privacy and adverse consequences for the doctor-patient relationship.
C) Prerequisites and additional factors for DHA use
DHAs have become widespread in everyday life for patients, as further results from the quantitative survey show. Forty percent of respondents estimated the share of their patients using DHAs and/or other digital tools for health prevention or disease management at between 10 and 15%; another 40% ballparked the figure at 15% to 20%. On average, doctors thought the use of DHAs would be or could be of interest to 16% of their own patients. This figure rose to 24% among doctors with practices in city settings.
Twenty percent of respondents reported being asked about DHAs by their own patients occasionally, 40% sporadically, and the remaining 40% reported never being asked. Doctors that had already been asked about DHAs mostly had their practices in towns and cities; those in small towns and rural communities were asked far less often (89% vs. 23%, p < 0.001).
There are various information sources on digital health available for GPs. However, only one in three respondents reported using these sources often at 5% or occasionally at 28%, and 32% used them rarely. Thirty-five percent stated that they had never looked for information about DHAs and similar tools. This proportion was particularly high among rural doctors at 62%. Most of the respondents found information on DHAs in specialist magazines (26%), association newspapers (23%), exchanges with colleagues (23%), and researching on the internet (21%).
Only a small proportion at 25% felt confident enough to distinguish between trustworthy and bad health apps, and only 22% felt they had a general picture as to the range of applications available. Just under a quarter at 24% expressed confidence in their ability to give patients capable advice on DHAs, health apps, and other digital tools. This included 42% among doctors in city settings but only 9% among rural respondents p < 0.001).
D) Willingness to use and prescribing DHAs in practice
We first asked participating doctors what basic requirements a digital health application should include for them to prescribe it, regardless of whether or not they had already used DHAs. Analysis of this open question showed that it was particularly important to respondents for DHAs to be clear and easy to understand (67%) and simple and intuitive to use (62%). It should ensure data privacy in the best possible way (59%), provide customizability options for 57% of respondents, and motivate patients to become more health-conscious in everyday life in a playful way such as by using gamification features for 56%. A sizable part of the sample emphasized that doctors must have reputable, reliable sources of information on the application concerned as a further requirement (49%). Some respondents at 32% cited permanent inclusion in the DHA register as an absolute requirement for prescription.
In everyday practice, 31% of those surveyed often or occasionally mentioned the possibility of using mHealth tools such as DHAs and health apps to support patients in disease prevention or management; 29% rarely mentioned this possibility. Eighteen percent had frequently or occasionally recommended specific apps for prevention, lifestyle changes and/or therapy in the past, and 21% reported that this happened rarely.
Specifically related to DHAs, 14% of all respondents had already prescribed such applications. This group had prescribed DHAs for prevention and self-monitoring (78%), lifestyle (73%), and fitness (60%). Respondents also increasingly mentioned applications for lifestyle change in type 2 diabetes mellitus, severe obesity, and prevention through exercise, and for dealing with depressive episodes, sleep disorders, and tinnitus. A breakdown showed that 21% of doctors in city practices had so far prescribed DHAs compared to 5% of doctors in rural practices (p < 0.001). Beyond that, 13% of doctors in the total sample stated that they planned to prescribe DHAs in the near future; this also targeted the areas already mentioned. Just over half at 51% were generally willing to prescribe DHAs compared to 22% stating that prescription was absolutely out of the question.
E) Experience with using DHAs
Of those doctors with general experience in DHAs, 85% reported the prescribed applications to have proven very useful at 34% or somewhat useful at 51%. Many reported positive effects related to health care and/or recovery. This especially applied to improved compliance and self-management in chronic disease, increased mobility, and measurable weight reduction (see Table 3). The greatest added value from DHAs was attributed to prevention and self-monitoring, health-oriented lifestyle, and exercise promotion.
F) Perceived optimization potential
In response to an open question, doctors with DHA experience outlined different priorities towards making DHAs more accessible and therefore more attractive for use in (primary) healthcare (see Table 4). These respondents saw potential for further improvement in user navigation and usability as well as structured further training for doctors as well as extension on interactivity and gamification elements, although they did express a relatively high level of satisfaction with DHAs that they had already used. Some also addressed the issues of remuneration, information, data privacy, and legal certainty. Many doctors felt a need for reliable and well-founded information on DHAs. The DHA directory was often criticized for not having detailed enough information, and information given sometimes too closely matching the manufacturer’s information. This was also linked to a fundamental criticism questioning the justification of the fast-track procedure in some cases. Some respondents suggested the German National Health Portal (www.gesund.bund.de) as a possible information platform focused on DHAs, potentially including an area specifically intended for doctors. Many GPs expressed a wish for statutory health insurance organizations to provide more advice and support to patients on using a DHA. Patients can already install some DHAs directly from their statutory health insurance organization if indicated without an explicit doctor's prescription [32].
More than three-quarters of doctors surveyed at 78% were generally willing to use DHAs significantly more (20%) or slightly more (58%) often than before if the improvements they looked for were to be implemented. However, 22% said they would not.
Discussion
Main findings
Previous studies have shown that many GPs associate health apps with positive potential, but they have so far been reluctant to integrate mHealth tools into healthcare due to major reservations on safety, reliability, and ease of use [23, 26, 27]. There was also a high degree of uncertainty in selecting suitable applications for patients from a large and dynamic app market [33, 34]. The DVG Act aims to create a basis for implementing DHAs in healthcare using clear-cut quality standards [1, 8]. So far, Germany is the only European country where the statutory health insurance covers state-approved health apps under certain conditions. It can be assumed that other countries might use the implementation of DHAs in Germany as a basis or role model for their own decisions [1, 7, 14].
The results of the present survey revealed a noticeably more favorable image, significance and increased acceptance of DHAs among GPs than in the case of ordinary health apps compared to previous surveys [21, 23, 28]. In this respect, the results are consistent with the qualitative interview study mentioned above, which was carried out with GPs experienced in DHA [29]. The qualitative interviews showed that the GPs interviewed rated DHAs favourably in terms of healthcare potential and as safer and more reliable compared to conventional health apps. GPs generally showed greater confidence in DHAs as being trustworthy, comparatively safe, and potentially effective due to the compulsory testing for a listing in the DHA directory and the legal framework.
The number of doctors with prescribing experience is still relatively low, but many of those surveyed saw the use of DHAs as worth considering or were already in the process of adopting them.
DHAs are considered especially useful in supporting prevention, self-monitoring and lifestyle changes as are high-quality health apps. Here, too, there are clear parallels in the general survey conducted by the Stiftung Gesundheit health foundation [35]. The largest cluster among respondents in a factor analysis included the perceived benefits of DHAs for health promotion, compliance, and motivation; respondents in another cluster mainly included effectiveness and efficiency in doctor-patient networking. This favorable assessment applies in a similar fashion to practical experiences with DHAs, with a clear majority of respondents reporting clinical benefits after having already prescribed these applications. This also applies to the results of the qualitative study: Almost all doctors interviewed reported a benefit from the applications they had prescribed. The positive effects observed especially referred to improved compliance and self-management in chronic disease [29]. Younger GPs and GPs with practices in urban areas are significantly and noticeably more open-minded and motivated towards using DHAs. This is a very common finding in the topical context under consideration and agrees with the observation that younger doctors are less reluctant to embrace new digital technologies [36]. The general situation and accompanying factors are often more favorable for this in urban settings, where doctors are already younger on average than in rural settings and benefit from advantages such as connectivity to digital infrastructure, division of labor, and digitally literate physician’s associations.
Willingness to use digital health applications in healthcare widely and on a consistent basis is currently still limited despite generally favorable assessment of DHAs and their potential use [19,20,21, 23, 35]. Most respondents currently lack confidence in their capability to introduce patients to DHAs and support their use due to lack of previous experience with mHealth programs [37, 38]. A lack of reliable sources of information has also left GPs with a major need for neutral research sources focused on health apps. The DHA directory is seen as needing improvement to make a qualified overview and selection of suitable applications possible.
Some respondents suggested the German National Health Portal (www.gesund.bund.de) as a possible information platform focused on this topic, potentially including an area specifically intended for doctors. A survey on GPs conducted by the authors on this portal has produced similar results [39]. Specialist associations and their management could provide support with their own information services and discuss clinical results from using DHAs. Respondents expressed a need to see a wide range of CME-certified, professional training courses to give GPs an understanding of the opportunities and conditions applicable to integrating DHAs into healthcare [33, 40, 41]. The results also reflected the lack of familiarity among GPs with the basics of the DVG Act, that is, data privacy, fees, and the legal situation. Respondents also saw importance in statutory health insurance organizations consistently and proactively advising patients on DHA rather than leaving their doctors to handle this responsibility on their own. The qualitative study, which preceded the present investigation, shows that physician’s associations could play an especially important role in providing information and supporting a dialog on mHealth topics [29]. Respondents expressed criticism at the lack of proof of effectiveness in the fast-track procedure as well as liability issues, especially in diagnostic and therapeutic DHAs, regardless of application potential. Many GPs saw a problem specifically in the DHA fast-track procedure.
Doctors with DHA experience focus on reinforcing motivational user-friendliness with uncomplicated usability ensured for mentally handicapped patients or patients unfamiliar with digital technology to use these apps easily [31, 42].
Comparison with prior work
GPs’ perception that DHAs are safe and reliable tools is reflected in the results of a Barmer survey [43]. Moreover, a survey among 569 outpatient doctors and psychotherapists showed that the majority trusted medical apps used on prescription despite the fundamental heterogeneity in the responding target groups [35].
Surveys specifically of GPs on the topic of potential uses of DHAs are, so far, almost completely missing. Nevertheless, the results of our study are compatible with several other surveys conducted in Germany that dealt with DHAs. These studies did not have an exclusive focus on general and family medicine and also had significantly smaller sample sizes with regard to individual specialist groups. For the trend study “Doctors in the future health market 2022 (Ärztinnen und Ärzte im Zukunftsmarkt Gesundheit 2022)”, 2,238 doctors from all specialist groups were surveyed in a representative manner [44]. It turned out that one in three of the doctors surveyed already had prescribing experience with DHAs, although in most cases only with a few applications. The doctors who already prescribe DHAs are mostly specialists. This also explains why the proportion of physicians who use DHAs is lower in our survey, since GPs, as primary care providers, have a different challenge in taking up digital applications in everyday care [12, 29]. The health market study also provided information about what is increasing the acceptance of DHAs among physicians: evidence of clinical evidence, changing patient needs towards digital solutions, familiarity with digital diagnostics and therapeutics, and support from medical societies and committees [44]. As the further results showed, doctors support the use of DHAs, especially in somatic and psychosocial areas (e.g. diary applications or apps that record vital parameters). The present work also found that lifestyle, prevention-related and psychosocial applications were clearly supported by GPs. Despite the obviously increasing acceptance, the results of the Stiftung Gesundheit study also provide evidence of hurdles that still exist, which lead many doctors to be skeptical about DHAs. The participants mentioned data protection concerns, doubts about the (empirically proven) effectiveness, excessive costs and doubts about the motivation of patients.
Another broad survey of practicing and clinical doctors in Germany is the “e-Health Monitor” [45]. Doctors from all specialist groups were asked about digital developments, including the possible uses of DHAs. The results indicate that many practicing doctors are fundamentally ambivalent about the increasing digitalization of the healthcare system. However, more than 60% of those who had experience with DHAs observed a positive supply effect. In this regard, there is something in common with the present survey.
A study conducted shortly after the introduction of DHAs among practicing physicians and psychotherapists found a high level of openness to such tools [16]. A total of 62% of respondents supported the opportunity to prescribe DHAs. Improved adherence, health literacy, and disease management were most frequently seen as benefits of DHAs.
Further investigations looked at specific groups of specialists and correspondingly small samples:
-
In 2021, a survey of 250 pain doctors and other health professionals showed that, although they perceive a benefit from DHAs, they have high requirements and expectations with regard to the quality of such applications. What is particularly important to health professionals is that DHAs do not require a lot of time and resources [46].
-
A survey of psychotherapists from 2021 revealed that 87% of respondents can imagine integrating DHAs into their treatment or were already doing so at the time of the survey. Potentials for using DHAs are seen especially in the quality improvement of therapy, in the increase of the sustainability of the therapy and in promotion of patients' health literacy. The therapists stated barriers in the lack of technical infrastructure and in the patients’ insufficient digital health literacy [47].
-
A survey of 75 rheumatologists in 2021/2022 found that respondents would like to be informed about DHAs via continuing education events, trade press, and manufacturers. 7% have already prescribed a DHA, while 46% planned to do so. 86% believed that using medical apps would at least partially be feasible and understandable to their patients. 83% thought that data collected by the patients using DHAs or other digital solutions could at least partially influence health care positively [48].
-
With regard to the management of depression, a qualitative study among GPs showed that they view digital interventions using DHA ambivalently. Advantages are, for example, the chance to offer patients a low-threshold, readily available treatment option with diverse language options. Interviewees criticized the costs and evidence basis of DHAs. Overall, there is a consensus that the prescription of digital interventions needs to be embedded in a personal provision of medical care. Physicians describe a lack of knowledge with regard to medical apps [49].
The criticism that the GPs surveyed in our study expressed with regard to the available information about digital tools is also reflected in the results of other studies. Several previous investigations have shown that GPs do not consider the information sources currently available to be sufficient in terms of transparency and reliability for patient support with DHAs or health apps [17, 21,22,23, 25,26,27,28, 43]. Besides, experts share GPs’ desire for greater usability and gamification. Krisam and Preis have explicitly recommended expanding on playful potential in (further) DHA development [31, 42, 50, 51]. These gamification elements combined with an intuitive user experience could stimulate behavioral changes in a low-threshold and sustainable manner.
Similar to the doctors surveyed, criticism of the DHA fast track procedure is also repeatedly expressed in expert reports and scoping reviews [52]. An application may be included in the DHA directory temporarily even if there is no evidence of any clinical benefit although other requirements are met. Statutory health insurance organizations would then be forced to cover the costs from then on even without any documented clinical benefit. The advisory council [53]. stated that the test procedure should focus on careful evaluation of the effectiveness and benefits of a DHA in its report on digitalization in healthcare. However, short DHA development cycles pose a challenge compared to the prolonged periods applicable to established study designs. The system for benefit assessment and insurance cover should therefore be designed in such a way that the safest possible apps with high quality and proven benefit are supplied to the healthcare system while also providing suppliers with an incentive to invest in developing these applications.
Expert reports on digitalization in healthcare encourage a wide range of professional and comprehensive training programs to familiarize GPs with the opportunities and conditions involved in integrating DHAs into patient care [16, 40, 41, 54]. Versluis et al. have provided a practical worksheet to effectively target expected or experienced barriers towards helping healthcare professionals in the process of implementing an eHealth intervention [33]. Houwink et al. have recommended incorporation of eHealth education into vocational training and CPD activities [54]. It would also be of importance for statutory health insurance organizations to advise patients consistently and proactively on the use of DHAs rather than leaving this to the physicians alone [7, 11, 22].
The inclusion of DHAs and their evidence-based use in medical guidelines can be an important contribution to systematically introducing practicing physicians to digital applications for the management of chronic diseases [40, 41]. In this context, medical societies can play an important role. Besides, better IT training in medical can be a valuable instrument to make doctors understand DHAs better.
Various authors explicitly advised expanding on gamification in DHAs: Prioritizing motivation such as by integrating gamification in an intuitive user experience could make more of a success at initiating lifestyle changes and keeping them in the long term [42, 51].
Take-Aways
Against the background of the comprehensive study results and the use of available literature, we would like to conclude by deriving a number of basic take-aways in a condensed form. Figure 1 brings together what we consider to be crucial starting points where improvements would make sense so that DHAs can be established as broadly as possible in primary care. The points presented can be assigned to four categories. Firstly, it is important to create differentiated incentive and remuneration structures for doctors (point 1). Secondly, physicians need reliable information and overview platforms as well as basic knowledge of DHAs and their use (points 2–4). Thirdly, it is important to optimize the formal and content-related framework conditions of DHAs (points 5–7). Fourthly, GPs should be involved in the development, testing and evaluation process of DHAs so that a primary care conformity of corresponding applications can be ensured in the long term (point 8).
In conclusion, all of the points mentioned would motivate GPs and provide additional support to prescribe DHAs in everyday care and to further support patients who use such applications. If GPs observe positive effects in patient care due to the use of DHAs and also have the opportunity to incorporate their feedback in order to optimize DHAs for outpatient care, this would promote positive momentum in the long term.
Strengths and limitations
The quantitative survey was specifically tailored to GPs and was based on several preliminary studies. It combined closed questions with several open questions for non-standardized information to be collected as well. The survey also achieved a comparatively high response rate, so the sample obtained was broadly spread for major characteristics and attitudes towards DHAs and their application potential.
Even so, the study cannot claim to be representative in the strict sense due to the limited number of cases and regional recruitment strategy, at most approximating to a representative study due to comparison with health insurance data. The survey regions included five federal states in Western Germany. For example, the largest federal states with the most inhabitants, such as North Rhine-Westphalia or Bavaria, are not included. The same applies for large city states such as Hamburg and Berlin. Apart from that, the risk of bias towards doctors with a specific interest in digitalization and health apps taking part cannot be excluded. The relatively high proportion of GPs with existing DHA experience compared to other studies among other factors supports this [36]. Even so, the sample obtained shows the respondents to be broadly spread across important factors and attitudes towards DHAs and their potential use.
The scaling method used in the questionnaire is another point of criticism. This was not always consistent, such as in the scale levels used or additional categories included such as “undecided” or “difficult to say.” This was due to the authors’ efforts to ensure that the survey was as easy to complete as possible given the time constraints applicable to the target group. Furthermore, it can be criticized that different scales alternate in the questionnaire. Theoretically, this can lead to an increased occurrence of incorrect response behavior. However, given the very practical development of the survey instrument and a detailed pretest, the authors did not find any problems with the survey target group answering the questions. In addition, the respondents are experts who are interviewed much more often on various topics and, therefore, are more familiar with scientific surveys than, for example, the general population. Nevertheless, it can be critically objected that when developing the study, attention could have been paid to greater similarity of the scales. Internal consistency could also have been examined during the development of the questionnaire.
Conclusions
This article presented the results of a survey of 5,868 general practitioners in five federal states of the Federal Republic of Germany. According to these results general practitioners have a favorable general view of DHAs regarding their care potential, and DHAs are seen as safer and more reliable than conventional health apps. Many of the doctors with experience of using DHAs report clinical benefits from DHA intervention. Many GPs also see the use of DHAs as worth considering going forward. This provides favorable conditions for implementation in primary care. However, the potential for digital health applications has not yet been exhausted.
Certain optimization approaches can be derived from the results. Integrating DHAs into primary care across the board will require educating general practitioners on the basics of the DVG Act and specifically addressing their desires and concerns towards increasing their acceptance by GPs in the medium and long term. Comprehensive training courses providing information on GPs as well as benefits and limitations of DHA use and strategies on how digital tools might be integrated consistently would seem to play a key role. There is also a need for increased orientation and overview for GPs to be able to assess which DHAs are useful for which area of application safely and what they need to take into account while using them.
Availability of data and materials
All major data generated or analysed during this study are included in this published article. Additional information can be provided on request made to the corresponding author.
Abbreviations
- DHA(s):
-
Digital Health Application(s)
- DVG:
-
Digitalization and Innovation Act
- GP(s):
-
General Practitioner(s)
References
Bundesgesetzblatt (2020): Gesetz für eine bessere Versorgung durch Digitalisierung und Innovation (Digitale-Versorgung-Gesetz – DVG) [Law for better care through digitalization and innovation (Improving Healthcare by Digitalisation and Innovation Act – DVG)]. https://www.bgbl.de/xaver/bgbl/start. xav?startbk=Bundesanzeiger_BGBl&jumpTo=bgbl119s2562.pdf#__bgbl__%2F%2F* %5B%40attr_id%3D%27bgbl119s2562.pdf %27%5D__1601186193941 [Accessed November 9, 2023].
Brönneke JB, Debatin JF, Hagen J, Kircher P, Matthies H: DiGA Vademecum. Was man zu Digitalen Gesundheitsanwendungen wissen muss [DiGA Vademecum. What you need to know about digital health applications]. Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft. 2020. German.
Stern AD, Brönneke J, Debatin JF, et al. Advancing digital health applications: priorities for innovation in real-world evidence generation. Lancet Digit Health. 2022;4(3):e200–6. https://doi.org/10.1016/S2589-7500(21)00292-2.
König IR, Mittermaier M, Sina C, et al. Evidence of positive care effects by digital health apps—methodological challenges and approaches. Inn Med. 2022;63(12):1298–306. https://doi.org/10.1007/s00108-022-01429-2.
Richter JG, Nannen C, Chehab G, et al. Mobile App-based documentation of patient-reported outcomes – 3-months results from a proof-of-concept study on modern rheumatology patient management. Arthritis Res Ther. 2021;23:121. https://doi.org/10.1186/s13075-021-02500-3.
Shaw T, McGregor D, Brunner M, et al. What is eHealth? Development of a conceptual model for eHealth: qualitative study with key informants. J Med Internet Res. 2017;19(10): e324. https://doi.org/10.2196/jmir.8106.
Kuhn E, Rogge A, Schreyer K, et al. Apps on Prescription in the Medical Office, but how? A Case-based Problem Outline of Medical-ethical Implications of DHA Usage. Gesundheitswesen. 2022;84(08/09):696–700. https://doi.org/10.1055/a-1473-5655.
Mäder M, Timpel P, Schönfelder T, et al. Evidence requirements of permanently listed digital health applications (DiGA) and their implementation in the German DiGA directory: an analysis. MC Health Serv Res. 2023;23(1):369. https://doi.org/10.1186/s12913-023-09287-w.
Bundesgesetzblatt (2020): Verordnung über das Verfahren und die Anforderungen zur Prüfung der Erstattungsfähigkeit digitaler Gesundheitsanwendungen in der gesetzlichen Krankenversicherung (Digitale-Gesundheitsanwendungen-Verordnung, DiGAV) [Ordinance on the procedure and requirements for examining the reimbursement of digital health applications in statutory health insurance (Digital Health Applications Ordinance, DiGAV)]. https://www.bgbl.de/xaver/bgbl/start. xav?startbk=Bundesanzeiger_BGBl&jumpTo=bgbl120s0768.pdf#__bgbl__%2F%2F* %5B%40attr_id%3D%27bgbl120s0768.pdf %27%5D__1601186510410 [Accessed November 9, 2023]
Bundesamt für Arzneimittel und Medizinprodukte (BfArM) [Federal Office for Drugs and Medical Devices (BfArM)] (2022): Für Leistungserbringer [For service providers]. https://diga.bfarm.de/de/leistungserbringer [Accessed November 9, 2023]
Gerlinger G, Mangiapane N, Sander J. Digital health applications (DiGA) in medical and psychotherapeutic care. Opportunities and challenges from the perspective of the healthcare providers. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2021;64(10):1213–9. https://doi.org/10.1007/s00103-021-03408-8.
Albrecht U-V (Ed.): Chancen und Risiken von Gesundheits-Apps (CHARISMHA) [Opportunities and Risks of Health Apps (CHARISMHA)]; 2017 [cited November 9, 2023]. Available from: http://www.digibib.tu-bs.de/?docid=00060000
Ernsting C, Stuhmann LM, Dombrowski SU, et al. Associations of Health App Use and Perceived Effectiveness in People With Cardiovascular Diseases and Diabetes: Population-Based Survey. JMIR Mhealth Uhealth. 2019;7(3): e12179. https://doi.org/10.2196/12179.
Ernstings C, Dombrowski SU, Oedekoven M, et al. Using Smartphones and Health Apps to Change and Manage Health Behaviors: A Population-Based Survey. JMIR. 2017;19(4): e101. https://doi.org/10.2196/jmir.6838.
Scott AR, Alore EA, Naik AD, et al. Mixed-Methods Analysis of Factors Impacting Use of a Postoperative mHealth App. JMIR Mhealth Uhealth. 2017;5(2): e11. https://doi.org/10.2196/mhealth.6728.
Dahlhausen F, Zinner M, Bieske L, et al. Physicians’ attitudes toward prescribable mHealth apps and implications for adoption in Germany: mixed methods study. JMIR Mhealth Uhealth. 2021;9(11): e33012. https://doi.org/10.2196/33012.
Hickey E, McMillan B, Mitchell C. Practitioners should embrace, not ignore, health apps. BMJ. 2015;350: h2336. https://doi.org/10.1136/bmj.h2336.
Leigh S, Ashall-Payne L. The role of healthcare providers in mHealth adoption. Lancet Digit Health. 2019;1(2):e58–9. https://doi.org/10.1016/S2589-7500(19)30025-1.
Brandt CJ, Søgaard GI, Clemensen J, et al. General Practitioners‘ Perspective on eHealth and Lifestyle Change: Qualitative Interview Study. JMIR Mhealth Uhealth. 2018;6(4): e88. https://doi.org/10.2196/mhealth.8988.
Nguyen AD, Frensham LJ, Baysari MT, et al. Patients‘ use of mobile health applications: what general practitioners think. Fam Pract. 2019;36(2):214–8. https://doi.org/10.1093/fampra/cmy052.
Wangler J, Jansky M. Potentials of health apps in primary care – a survey among general practitioners. Präv Gesundheitsf. 2020;16(2):150–6. https://doi.org/10.1007/s10354-021-00814-0.
Peeters JM, Krijgsman JW, Brabers AE, et al. Use and uptake of eHealth in general practice: a cross-sectional survey and focus group study among health care users and general practitioners. JMIR Med Inform. 2016;4(2): e11. https://doi.org/10.2196/medinform.4515.
Wangler J, Jansky M. Health apps as instruments of prevention? – A qualitative study on the potential for the primary care setting. Präv Gesundheitsf. 2020;15(4):340–6. https://doi.org/10.1007/s11553-020-00769-x.
Mittermaier M, Sina C, Richter JG, et al. Practical use of digital health applications (DiGA) in internal medicine. Internist. 2022;63:245–54. https://doi.org/10.1007/s00108-022-01264-5.
Byambasuren O, Beller E, Glasziou P. Current Knowledge and Adoption of Mobile Health Apps Among Australian General Practitioners: Survey Study. JMIR Mhealth Uhealth. 2019;7(6): e13199. https://doi.org/10.2196/13199.
Bittner J (2017): So denken Ärzte über Digital Health: Eine Synopse der aktuellen Umfragen [This is how doctors think about digital health: A synopsis of current surveys]. https://blog.der-digitale-patient.de/synopse-aerztebefragungen-digital-health/ [Accessed November 9, 2023]
Radić Marija, Waack M, Donner I, et al.: Digitale Gesundheitsanwendungen: Die Akzeptanz steigern. Dtsch Arztebl 2021; 118(6): A-286–292
Wangler J, Jansky M. Significance and application potential of health apps in diabetological care – results of a survey study. Diabetologie und Stoffwechsel. 2023;18(01):69–77. https://doi.org/10.1055/a-1859-6400.
Wangler J, Jansky M. Two years of approved digital health applications in Germany - Perspectives and experiences of general practitioners with an affinity for their use. Eur J Gen Pract. 2023;29(1):2186396. https://doi.org/10.1080/13814788.2023.2186396.
Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM) (2022): Das Fast Track Verfahren für digitale Gesundheitsanwendungen (DiGA) nach § 139e SGB V. Ein Leitfaden für Hersteller, Leistungserbringer und Anwender [The Fast Track procedure for digital health applications (DiGA) according to Section 139e SGB V. A guide for manufacturers, service providers and users]. https://www.bfarm.de/SharedDocs/Downloads/DE/Medizinprodukte/diga_leitfaden.pdf?__blob=publicationFile [Accessed November 9, 2023]
Byambasuren O, Beller E, Hoffmann T, et al. Barriers to and facilitators of the prescription of mhealth apps in Australian general practice: qualitative study. JMIR MHealth UHealth. 2020;8(7): e17447. https://doi.org/10.2196/17447.
Faktorenanalyse FS. In: Baur N, Fromm S, editors. Datenanalyse mit SPSS für Fortgeschrittene. Ein Arbeitsbuch [Data analysis with SPSS for advanced users. A workbook]. Wiesbaden: Springer; 2008. p. 314–44.
Versluis A, Van Luenen S, Meijer E, et al.: SERIES: eHealth in Primary care. Part 4: addressing the challenges of implementation. Eur J Gen Pract 2020;26(1):140–145. doi: https://doi.org/10.1080/13814788.2020.1826431.
de Wilt T, Versluis A, Goedhart A, et al. General practitioners attitude towards the use of eHealth and online testing in primary care. Clinical eHealth. 2020;3:16–22. https://doi.org/10.1016/j.ceh.2020.02.002.
Stiftung Gesundheit (2021): Ärzte im Zukunftsmarkt Gesundheit 2021. Ein Jahr Digitale Gesundheitsanwendungen [Doctors in the future market of health 2021. One year of digital health applications]. https://www.stiftung-gesundheit.de/pdf/studien/aerzte-im-zukunftsmarkt-gesundheit_2021_2.pdf [Accessed November 9, 2023]
Spoont M, Greer N, Su J et al.: Rural vs. Urban Ambulatory Health Care: A Systematic Review. VA Evidence-based Synthesis Program Reports 2011.
Gruessner V (2017): Only 15% of Doctors Recommend Mobile Health Apps to Patients. https://mhealthintelligence.com/news/only-15-of-doctors-recommend-mobile-health-apps-to-patients [Accessed November 9, 2023]
Rohlender B, Reinhardt K (2017): Gesundheit 4.0 – Wie Ärzte die digitale Zukunft sehen [Health 4.0 – How doctors see the digital future]. http://www.hartmannbund.de/fileadmin/user_upload/Downloads/Umfragen/2017_HB-Bitkom_Start-ups.pdf [Accessed November 9, 2023]
Wangler J, Stachwitz P, Jansky M. Can a National Health Portal Support Primary Care? – A Survey of General Practitioners. Gesundheitswesen. 2021;83(8–9):596–603. https://doi.org/10.1055/a-1195-2312.
Dahlhausen F, Zinner M, Bieske L, et al. There’s an app for that, but nobody’s using it: Insights on improving patient access and adherence to digital therapeutics in Germany. Digital Health. 2022;8:205520762211046. https://doi.org/10.1177/20552076221104672.
Dufour JC, Grosjean J, Darmoni S, et al. ApiAppS: A Project to Study and Help Practitioners in Recommending mHealth Apps and Devices to Their Patients. Stud Health Technol Inform. 2019;264:1919–20. https://doi.org/10.3233/SHTI190713.
Harst L, Lantzsch H, Scheibe M. Theories Predicting End-User Acceptance of Telemedicine Use: Systematic Review. J Med Internet Res. 2019;21(5): e13117. https://doi.org/10.2196/13117.
Barmer (2020): BARMER-Umfrage zu Gesundheits-Apps – Ärzte stehen digitalen Helfern offen gegenüber [BARMER survey on health apps - Doctors are open to digital helpers]. https://www.barmer.de/presse/presseinformationen/pressemitteilungen/barmer-umfrage-zu-gesundheits-apps---aerzte-stehen-digitalen-helfern-offen-gegenueber-247444 [Accessed November 9, 2023]
Stiftung Gesundheit (2022): Ärzte im Zukunftsmarkt Gesundheit 2022. Digitale Gesundheitsanwendungen (DiGA) in der Praxis: Erkenntnisse und Erfahrungen [Doctors in the future market of health 2022. Digital health applications (DiGA) in practice: findings and experiences]. https://www.stiftung-gesundheit.de/pdf/studien/aerzte-im-zukunftsmarkt-gesundheit_2022_barrierefrei.pdf [Accessed December 12, 2023]
McKinsey & Company, Müller T, Padmanabhan P, Richter L, Silberzahn T (Eds.). E-Health Monitor 2022. Deutschlands Weg in die digitale Gesundheitsversorgung – Status quo und Perspektiven [E-Health Monitor 2022. Germany's path to digital healthcare – status quo and perspectives]. Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft; 2022.
Priebe JA, Stachwitz P, Hagen J, et al.: Einstellung zur digitalen Medizin im Schmerzbereich. Eine Umfrage unter Ärzten und Patienten der Deutschen Schmerzgesellschaft und Patientenorganisationen [Attitudes toward digital tools in pain medicine. Survey of German Pain Society health professional members and members of self-help groups]. Schmerz 2023;1–9 [Online ahead of print]. https://doi.org/10.1007/s00482-023-00708-7.
Frey S, Kerkemeyer L. Acceptance of digital health applications in non-pharmacological therapies in German statutory healthcare system: Results of an online survey. Digit Health. 2022;8:20552076221131144. https://doi.org/10.1177/20552076221131142.
Richter JG, Chehab G, Stachwitz P, et al. One year of digital health applications (DiGA) in Germany – Rheumatologists’ perspectives. Front Med (Lausanne). 2022;9:1000668. https://doi.org/10.3389/fmed.2022.1000668.
Posselt J, Klawunn R, Dierks M-L. Verordnung Digitaler Gesundheitsanwendungen (DiGA) an Menschen mit depressiven Erkrankungen: Ergebnisse einer qualitativen Studie. Z Allg Med. 2023;99(2):1–6. https://doi.org/10.1007/s44266-023-00034-2.
Brönneke JB, Hagen J, Kircher P, et al. Digitized healthcare in 2030-a possible scenario. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2021;64(10):1285–91. https://doi.org/10.1007/s00103-021-03416-8.
Krisam M, Prieß N. Digital Behavior Design für nachhaltig nachhaltig gesundheitsbewusstes Verhalten [Digital behavior design for sustainable, health-conscious behavior]. In: Baas J, editor. Gesundheit im Zeitalter der Plattform-Ökonomie [Health in the age of the platform economy]. Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft; 2022. p. 146–55.
Giebel GD, Speckemeier C, Abels C, et al. Problems and Barriers Related to the Use of Digital Health Applications: Scoping Review. J Med Internet Res. 2023;25: e43808. https://doi.org/10.2196/43808.
Sachverständigenrat zur Begutachtung der Entwicklung im Gesundheitswesen [Advisory Council for the Assessment of Developments in the Health Care System]: Digitalisierung für Gesundheit. Ziele und Rahmenbedingungen eines dynamisch lernenden Gesundheitssystems [Digitization for health. Goals and framework conditions of a dynamically learning health system]. (2021) https://www.degam.de/files/Inhalte/Degam-Inhalte/Aktuelles/2021/SVR_Gutachten_2021_online.pdf [Accessed November 9, 2023]
Houwink EJF, Kasteleyn MJ, Alpay L, et al. SERIES: eHealth in primary care. Part 3: eHealth education in primary care. Eur J Gen Pract 2020;26(1):108–18. https://doi.org/10.1080/13814788.2020.1797675.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research was not funded.
Author information
Authors and Affiliations
Contributions
The authors alone are responsible for the content and the writing of the paper. JW prepared, coordinated and implemented the project. Both JW and MJ contributed to the project design, analysis of transcripts and drafting of the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. The study did not involve collecting patient data or conducting clinical tests. Accordingly, the Ethics Commission of the State of Rhineland-Palatinate informed us that approval by an ethics committee would not be necessary. The researchers identified the participants and obtained their written informed consent to participate before the start of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Questionnaire: How can primary care benefit from digital health applications?
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wangler, J., Jansky, M. How can primary care benefit from digital health applications? – a quantitative, explorative survey on attitudes and experiences of general practitioners in Germany. BMC Digit Health 2, 14 (2024). https://doi.org/10.1186/s44247-024-00068-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44247-024-00068-x