Abstract
Background
Opioid use disorder is associated with a huge burden of disease and treatment gap. Delivery of psychosocial treatment using digital platforms can bridge the treatment gap to improve treatment access among individuals with opioid use disorder. The aim of this study was to assess the acceptability, feasibility and preliminary efficacy of a text-message intervention in patients with opioid use disorder in Nairobi, Kenya.
Methods
A feasibility pilot trial was conducted at a methadone clinic in Nairobi. A text-message intervention based on cognitive behaviour therapy was delivered for six weeks compared with a control group receiving standard treatment among 46 individuals on methadone treatment (30 in intervention and 16 in control group). Follow up was at six weeks and three months. Primary outcome was reduction in opioid use and retention in treatment. Implementation outcomes assessed were acceptability and feasibility of the intervention.
Results
The participants comprised 89.1% male with a mean age of 32 years (SD 8.7). There was a reduction in opioid use among all the participants post-intervention with higher reduction in the intervention group compared the control group with prevalence of opioid use at 35.7% and 56.3%, respectively although there was no statistically significance difference. Retention in methadone was 93.3% at six weeks and 83.3% at 3 months follow up among participants in the intervention group. High acceptability and satisfaction were reported with the intervention based on quantitative assessment post-intervention.
Conclusion
Results from this pilot feasibility study suggest that a text message intervention is acceptable and scan be implemented in substance use disorder treatment with promising effect in improving outcomes. Further research using a larger sample size is recommended.
Trial registration
Pan African Clinical Trial Registry: Registration number: PACTR202201736072847. Date of registration: 10/01/2022.
Similar content being viewed by others
Introduction
Opioid use is prevalent with significant burden of disease globally. According to the world drug report 2022, 60 million people reported past-year opioid use in 2020 with a two-fold increase between 2010–2020 [1, 2]. In Kenya opioid use is also prevalent [3, 4] with reported increase in multiple areas in the country [5]. Opioid use is associated with negative effects such as risk for opioid overdose, risk of infections among those using via injection as well as negative impact on families and employment [4].
The recommended treatment for opioid use disorder (OUD) is pharmacotherapy of which methadone is the most commonly used [6,7,8]. Psychosocial interventions are provided as adjunct treatment and include cognitive behaviour therapy (CBT) [9,10,11]. Despite the available treatment options for OUD, there still remains a huge treatment gap and low uptake of treatment. This is due to factors such as limited availability of treatment programs, individual barriers such as difficulty with regular treatment attendance, societal factors such as stigma [12,13,14,15] and barriers faced by treatment facilities that limit availability of psychosocial treatment such as low staffing, high staff turnover, limited finances and administrative factors such as national policies on provision of substance use disorder (SUD) treatment [1, 16].
There is growing use of digital interventions in psychosocial treatment delivery [17, 18]. These interventions can help address some of the challenges to improve access to psychosocial treatment for patients with OUD [17, 19, 20]. Advantages of digital interventions include privacy, convenience, reach, cost effectiveness, ability for remote delivery which saves time and could address the stigma associated with having to consult a therapist [16, 21, 22]. Among the digital platforms, mobile phones have the added advantage in being more portable which increases their utility in connecting with people with limited access to health care settings and have thus been used to offer digital treatment in several conditions including SUD [21, 23,24,25]. Text-messaging is increasingly being used in SUD treatment [26,27,28,29] and text-message interventions can help facilitate delivery of CBT in individuals with SUDs, as these interventions are associated with low cost, are highly scalable, user friendly and allow flexibility in treatment delivery [26, 30]. Text-message interventions have been used among individuals with OUD and have shown effectiveness in improving opioid use and other outcomes with high acceptability [31, 32].
Cognitive behaviour therapy combines training in behaviour skills, cognitive interventions, and lifestyle modification strategies. The aim is relapse prevention with emphasis on developing self-management skills and strategies to maintain the change. CBT has been used in a wide range of SUDs and is effective both as monotherapy or in combination with other psychosocial therapies or pharmacological interventions [33,34,35]. In OUD, CBT has been shown to improve outcomes such as abstinence from opioids, addiction severity and quality of life [35,36,37]. CBT application for SUD treatment in low and middle-income countries (LMICs) is limited [38, 39]. This can be due to challenges such as limited availability of quality training and supervision, high number of patients and high rate of clinician turnover [40, 41]. Some of these challenges can be circumvented by use of technology to deliver CBT [40, 42, 43].
Increase in digital platforms especially access to mobile phone has enabled use of digital interventions in healthcare. In Kenya, there is high phone ownership in the general population with a prevalence of feature phones and smartphones at 67.9% and 53.4% respectively in 2021 [44]. Among specific populations the prevalence ranges from 69% among youth attending outpatient clinics [45], 79% among adults in informal settlements [46] and 77.1% among individuals with OUD with majority using basic phones [47]. In addition, those without phones report access through others such as family and friends [46,47,48]. Mobile phone interventions have been used in Kenya predominantly through text messaging. These interventions have been used in conditions such as immunization, cancer screening and infectious diseases with high acceptability and effectiveness [49,50,51]. There is limited research on use of text-message intervention among individuals with SUD.
In Kenya research on interventions targeting SUD is limited [4]. In addition, there is limited use of digital interventions in SUD treatment in Kenya and other LMICs [52]. In Kenya, only two studies report on use of digital interventions in SUD whereby one study was conducted at a rural clinic [53] and the other among university students in Nairobi [54]. Despite the increase in methadone treatment clinics in Kenya from one in 2014 to current eight [55, 56], the retention rate is low at 54% [57] which indicates need to seek measures to improve outcomes. Patients on methadone treatment indicate need for psychosocial services in addition to methadone while on the other hand they report time limit as they have to go to work after the daily visit to the clinic [58]. This study therefore sought to assess the implementation of a digital intervention for psychosocial treatment among the patients with OUD. Prior to implementation of an intervention it is important to assess the acceptability (extent to which stakeholders think the intervention is agreeable and satisfactory) and feasibility (the extent to which an intervention can be applied in a given setting) in order to identify barriers and facilitators to the intervention [59]. Among individuals with SUD, use of a digital intervention as an add-on to an existing program and delivery in a clinic is more effective than those interventions used alone [60]. Majority of individuals on treatment at the clinic use text message and 88% were willing to receive psychosocial treatment via text message [47]. Therefore, the aim of this study was to describe the feasibility, acceptability and preliminary efficacy of a text-message intervention based on CBT among individuals with OUD on methadone treatment.
Methods
Study design
This study was a randomized feasibility trial conducted in accordance to consolidated standards of reporting trials (CONSORT) guidelines: extension for pilot and feasibility trials [61].
Study setting and population
This study was carried out at the Ngara Methadone Clinic in Nairobi, a public health facility offering treatment to individuals with OUD that has been in operation since February 2017. Treatment at the clinic is free of charge. The eligible participants had (1) age 18 years and above; (2) OUD as per DSM-5 criteria and were receiving methadone treatment [62]; (3) urine toxicology screen testing positive for non-medical opioids; (4) access to a phone that could send and receive text message; (5) ability to read and write in English or Kiswahili and (6) provided informed consent. Those with no access to phones with text message capability, unable to communicate via text message in English or Kiswahili were excluded.
Text-message intervention
This study used stage 1 of the National Institute of Health (NIH) stage model of development of a psychosocial intervention. This comprises stage 1a which involves development of the therapy and stage 1b which involves pilot testing of the intervention. A new intervention includes modification of an existing treatment method [63]. The initial step was a review of literature on use of CBT in SUD treatment and application of digital interventions to deliver CBT treatment. In addition, input was sought from clinicians (clinical psychologists and addiction counsellors) actively involved in provision of CBT for patients with substance use disorders to develop the actual messages to be sent to the participants. This is in line with previous research that involved development of a text message intervention [64]. Also the intervention was based on findings on mobile phone use and acceptability for digital interventions among individuals with OUD done prior to implementation [47].
The text message intervention in this study used CBT based on the CBT manual on the treatment of substance use [33]. Although designed for use in individuals with cocaine dependence, the structured format of the manual is recommended and has been used in several substance use disorders including OUD with digital delivery in some studies [42, 65,66,67]. There were six modules adapted for this study provided as one module per week over six weeks. In this study the module on HIV prevention was excluded since this is covered as part of standard treatment at the clinic. The adaptation in the context of this study was delivery of the modules via text messages compared to the face-to face delivery described in the manual [33]. The adapted model and contents of the modules is described in Table 1.
There were weekly text-messages for six weeks. The text message was in three parts: first to introduce the weekly module; second, teaching on the behaviour strategy; and finally, practical exercise for the strategies learnt in the module (homework). Participants were required to send the homework response back via text message and were allowed to ask any questions regarding the weekly module. The text-messages were sent on the same day to all participants. This sequence of text content was as proposed in the CBT manual therapists’ guidelines for structuring sessions which begin with introduction of skill topic, didactic instructions, and assessment through practice exercise [33]. However, modelling and role play done during a face-to-face session were absent in the digital intervention. An additional text-message reminding the participants on weekly practical exercise/ homework was sent to those who did not respond within two days. The weekly messages sent are attached as supplementary material.
Standard treatment
Standard treatment at the methadone clinic includes daily methadone dosing; review by clinical team for methadone dose adjustment if required or for any physical or psychiatric symptoms; psychosocial services that are mainly focused on enhancing clinic rules and addressing any psychosocial stressor that may arise. In addition, screening and treatment for co-occurring medical and psychiatric disorders is provided.
Recruitment
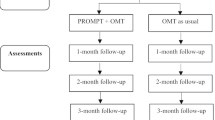
Participants were recruited during daily visits to the clinic. Staff at the clinic were notified about the study and asked to refer individuals meeting inclusion criteria to the research team. The research assistant then provided the individuals with information about the study and assessed for eligibility criteria. Those who met the inclusion criteria and were willing to participate in the study provided written informed consent. After an initial assessment (pre-intervention/baseline), participants were randomly assigned to either the treatment or control arm and then followed up. Participants received reimbursement of gift package worth Ksh 150 ($1.5) for time spent to fill questionnaire at baseline and 6-weeks follow up. Figure 1 shows the flow diagram of the recruitment, allocation to study arm and follow up.
Randomization and blinding
This was a two-arm randomized control feasibility trial. Participants were randomized to two groups, an intervention group that received text message intervention in addition to standard treatment as usual and a control group that received treatment as usual at 2:1 allocation ratio. Simple randomization using a computer program was used to generate the random numbers. Written allocation was sealed in individual opaque envelopes marked with study identification numbers. After an individual consented to participate in the study and had met the inclusion criteria, the participant was enrolled and given the initial assessment. They were then assigned the randomized study arm by the research assistant opening the sealed envelope to determine allocation. There was no blinding since the participants allocated to either group were aware of their treatment allocation.
Sample size determination
The recommended minimum sample size for pilot trials is 12 [68] with a range of 10–75 participants [69]. In this study an unequal randomization ratio of treatment to control of 2:1 was used, to allow for learning curve and hence maximize the information gained on the text message intervention (potential to improve treatment outcomes and assessment of acceptability and feasibility) while including a control group since this was a new intervention not used previously in the study setting [70]. This being a pilot study to assess feasibility of implementing a newly adapted digital intervention, no power computations were performed [71, 72]. The total sample size was 46 (30 participants in the intervention group and 16 participants in the control group) to allow accommodation for possible dropout.
Technical support
Participants were asked to inform and/or contact the researchers to address any technical difficulties they experienced. The research assistant was available at the clinic and participants were given a chance to seek any assistance during their daily visit to the clinic.
Outcomes and measures
Sociodemographic and clinical data
This was collected using a researcher-designed questionnaire. The variables collected include age, gender, educational level, marital status and employment, substance use, gambling history, current methadone dose and duration in treatment.
Primary outcomes
Opioid use
This was assessed using abstinence from opioids and change in frequency of use based on number of days a participant used non-medication opioids assessed by self-report and urine drug screen (UDS). The self-report was done using WHO Alcohol Smoking and Substance Involvement Screening Test (ASSIST) at baseline and timeline follow-back (TLFB) tool during follow up. The ASSIST is a research tool used to screen for problematic or risky substance use. A total score for each substance is obtained by summing up responses for questions. This score categorizes an individual to a risk category that indicates the risk for problematic health consequences based on their response for each substance [for alcohol: Low = 0–10, Moderate = 11–26 High = 27 + ; for other substances: Low = 0–3; Moderate = 4–26, High = 27 +] [73]. It has been previously used in Kenya [74, 75]. In this study we assessed lifetime use and use in past three months. Use in past three months was used to calculate the risk category at baseline. Timeline follow-back is a calendar-assisted structured interview used in assessment of substance use scored by an individual tabulating the number of days they used substances [76,77,78]. It has been used previously in Kenya [79, 80]. In this study we asked about substance use in past 30 days which was used as self-reported substance use at baseline and at six weeks follow up.
Retention in treatment
Retention was defined as number of days that a participant continued and remained in treatment at six weeks and those actively receiving methadone treatment at three months.
Secondary outcomes
Use of other substances use
Use of other substances was assessed using the ASSIST questionnaire and UDS at baseline assessment then reassessed through self-report using TLFB tool (past 30-day use) and UDS at end of treatment.
Psychiatry comorbidity
Comorbid psychiatric disorders was assessed via Mini international neuropsychiatric interview (MINI version7.02) [81]. In this study five modules were assessed namely; major depressive disorder suicidality, generalized anxiety disorder, posttraumatic stress disorder and antisocial personality disorder. In Kenya MINI has been used in previous studies [82, 83]. MINI is a licensed tool and permission to use the tool was given by the author to the principal investigator.
Addiction severity
Addiction severity was assessed by use of Maudsley Addiction Profile (MAP) at baseline, a brief structured interview that assesses problem substance use in four domains [84, 85]. Though not previously used in Kenya, MAP has been use regionally in South Africa [86].
Quality of life
Quality of life was assessed using World Health Organization Quality of Life short version instrument (WHOQOLBREF) It has 26 items that assess quality of life in four domains namely: Physical Health, Psychological Health, Social Health, and Environmental Health. The mean score of items within each domain is used to calculate the domain score which is then multiplied by 4 to make domain scores comparable with the scores used in the WHOQOL-100 [87, 88]. This tool has been used in Kenya [89].
Drug taking self-efficacy
The drug taking confidence questionnaire (DTCQ-8) which is a tool that assesses anticipatory coping self-efficacy over eight categories of high-risk situations for substance use was used. Participants respond how confident they are to resist substance use on a six-point scale ranging from ‘not at all’ to ‘very confident’ (20–100%). The means score for the eight questions gives the total score which then shows the level of self-efficacy with a lower the score signifying a lower the self-efficacy and vice versa [90].
Readiness to change
Readiness to change was assessed at baseline using Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) which is a 19-item tool used to assess readiness and motivation for change with good validity and reliability [91]. The 19 items are scored on a five-point Likert scale to yield three subscales namely (1) Recognition which assesses acknowledgement of a substance-related problem and desire for change; (2) Ambivalence which assesses perceived control over substance use and substance problems; (3) Taking steps which measures the extent to which an individual is making positive efforts to change substance-using behaviour. From these a score is calculated and classified in low, moderate and severe category to change [91].
Implementation outcomes
Acceptability
At six-week post-treatment follow up, an evaluation survey was conducted on feedback regarding various aspects of using the text-based intervention. The quantitative assessment was via a Likert scale–based assessment tool. Some questions in this tool were adapted from Client Satisfaction Questionnaire (CSQ 8) and System Usability Scale and additional questions specific to the content of text-based intervention. In addition, the questionnaire included a qualitative segment with three open-ended questions at the end. The responses to these questions were analyzed qualitatively and are reported separately.
Client satisfaction questionnaire (CSQ)
Client Satisfaction Questionnaire (CSQ-8) was developed to assess satisfaction in psychotherapy treatment as a shorter version of the original CSQ that had 18 items. Validation studies have shown good internal consistency and high correlations with other tools. The CSQ-8 items are scored on a scale from 1 to 4 with total score ranging from 8 to 32 [92, 93]. In this study we summarized the responses descriptively in Table 4. CSQ is a copyrighted tool, for which permission to use was requested from the author by the principal investigator. Detailed score of each item is attached as an Additional file 1.
System Usability Scale (SUS)
System Usability Scale (SUS) collects subjective data about technology product usability. A scoping review on methods used to test usability on developing eHealth technology reported that SUS was the most validated questionnaire. SUS is a 10- item scale in which the items are scored on a Likert scale from 0 (strongly disagree) to 4 (strongly agree) with half of the items reverse- scored [94]. In this study the term ‘system’ was replaced by ‘intervention’, but no other modification was made. We summarized the scores descriptively as shown in Table 4. Details of individual scores for all items is presented as Additional file 1: Appendix 2.
Feasibility assessment
This was assessed using participant engagement and adherence to the intervention. Engagement refers to the effort made by a client during course of treatment towards change, of which treatment participation is an early component [95, 96]. In this study engagement was defined a priori as use of the text message intervention for those enrolled assessed by response to the weekly practical homework at least once during the treatment period. This is based on findings whereby most studies define engagement in psychosocial treatment as attendance of at least one session or signing up for digital interventions [95, 97]. Adherence in digital interventions is based on usage behaviour such as number of logins or sessions completed [98, 99]. Adherence was defined a priori as those who used the digital intervention for at least half of the study duration (three weeks). This included those who acknowledged receipt of the text messages and/or responding to the weekly practical homework sent to the participants. This was based on past research whereby an attrition of 20–50% in psychosocial treatment is reported [95].
Data analysis
All analyses were conducted using Stata Version 13.1. Feasibility parameters were reported descriptively. Baseline population characteristics was summarized descriptively by treatment group whereby intervention and control groups were compared using Fisher’s Exact and Wilcoxon rank-sum tests. Treatment duration at baseline was summarized as number of years in methadone treatment and status at baseline which was categorized as follows: those newly enrolled to methadone treatment during the study period (new), those who had been on treatment but had resumed opioid use and were returning to treatment (Reinduction) and those who had positive urine test positive for opioids while on methadone treatment (continued treatment). To examine the efficacy of the intervention, opioid use rate at baseline and at follow up were compared. For post intervention evaluation data, a descriptive summary was done on individual responses to the questions on usability and satisfaction of the intervention. As a feasibility trial, the study was not powered for formal testing of intervention effectiveness; however, group differences for selected outcome measures were explored using Wilcoxon rank-sum tests conducted before and after overall and for each group separately for continuous outcomes and McNemar test for categorical outcomes. The significance level was set at p < 0.05.
Results
Participant enrollment
As shown in Fig. 1, 95 individuals with positive UDS for non-medical opioids were screened for eligibility of which 49 (51.5%) were excluded. The commonest reason for exclusion was lack of phones (35.7% of those screened and 69.3% of those excluded).
Sociodemographic and clinical characteristics of participants
The mean age of participants was 32 years (SD 8.7), range 22–63 years (IQR 10.5). Majority of participants were male (89.1%), had primary education of eight years or less (50%). As shown in Table 2 which summarizes the baseline sociodemographic and clinical profiles of participants, there was no significant difference among participants in intervention or control groups at baseline, except in age at first drug use (p = 0.045).
Based on ASSIST score the commonest substances used other than opioids were alcohol, cannabis, tobacco, and benzodiazepines. Majority (60.9%) of participants had high risk for opioid use as per ASSIST score at baseline. This is shown in Table 3.
Primary outcomes
Abstinence from opioid use
Overall, there was a reduction in opioid use from baseline to post intervention. There were more individuals with abstinence from opioids in the intervention group compared to controls both on self-report and based on UDS as shown in Fig. 2. However, there was no statistically significant difference between the groups (OR 0.43, 95% CI 0.12–1.51, p = 0.19). A reduction in frequency of use was also observed. At follow up, no participants reported use daily or almost daily; 3.6% reported weekly use compared to 23.3% at baseline and 21.4% reported using once or twice compared to 10.0% at baseline. This is summarized in Fig. 4.
Retention in treatment
Two participants (4.3%) were lost to follow up at six weeks and five (10.9%) at 3 months follow up. All participants lost to follow up were in the intervention group.
Implementation outcomes
Feasibility
System use
Overall, only five of 30 participants (16.7%) did not respond to any homework question and six (20%) responded to all the questions while 26.7% responded to five messages; 23.3% responded to four messages and 3.3% responded to one and two messages each.
Engagement
Twenty-five participants (83.3%) responded to at least one homework question.
Adherence
Twenty-three (76.7%) responded to at least half of the messages.
No participant requested to withdraw from the study and the post-intervention interview, most participants responded to the follow-up questionnaire whereby invite to respond was sent via message. Also, two participants who had not responded to any message participated in the qualitative interviews and gave feedback on the intervention.
Response to weekly homework questions
Figure 3 shows response to the messages by week. There was higher use of the intervention at week 1 and 6 with dips at week 3,4,5. When participants were asked which module, they found most helpful there was an almost similar average score for all the modules. This is shown in Additional file 1: Appendix 2. We did comparisons based on: 1) type of phone used during the intervention which whereby 53.6% used smartphones, 39.3% used regular phone and 7.1% used both types at different times during the study period. A higher number of those using smartphones responded in four and more weeks. 2) Status at baseline: majority of those who did not provide any response were those with continued opioid use during treatment while those who had been reinducted to treatment comprised majority of those who responded to five- and six-weeks’ homework questions. This is shown in figures attached as Additional file 1: Appendices 3 and 4.
Acceptability and satisfaction
System usability
As shown in Table 4, the majority of participants reported the intervention as easy to use based on system usability scores with only 7.4% reporting that the intervention was complex. Majority of participants agreed (66.7%) or strongly agreed (25.9%) that the various components of the intervention were well integrated and majority disagreed or strongly disagreed that they need to learn a lot of things before using the intervention.
Satisfaction with intervention
There was high satisfaction with the intervention based on client satisfaction questionnaire, summarized in Table 4. All the participants reported that they got the service they wanted, 66.7% reported that most of their needs were met and 70% were satisfied or very satisfied with the intervention. Regarding the delivery of the intervention, 66.7% found the treatment duration as just right; 92.6% found the frequency of messages as right and all participants reported the message content as right or adequate.
Secondary outcomes
Reduction in other substance use
There was an overall reduction in other substance use at follow up based on urinary drug screen and self-report. A similar pattern of reduction in frequency use was also noted, whereby less participants reported daily or almost daily use of substances at follow up. Of note is that tobacco was the most used substance at follow up. This is summarized in Figs. 4 and 5.
Self-efficacy
There was an overall significant increase in DCTQ-8D scores after the intervention (p < 0.001). When sub-group analyses were conducted using Wilcoxon signed rank test, there was a significant increase in the intervention group (p < 0.001), while no significant increase was observed in the control group (p = 0.075). This is shown in Table 5.
Readiness to change
As shown in Table 3, the SOCRATES score showed majority in very low to low score in recognition docile, majority in medium score for the ambivalence docile and majority had high scores in the taking steps docile.
Addiction severity
The scores in MAP shown high risk at baseline based on risky behaviour, missed employment and engagement in illegal activities. This is shown in details on Table 3.
Discussion
This study aimed to assess the feasibility, acceptability, and preliminary efficacy of a text message intervention among individuals with OUD. The findings showed that use of a text message intervention is feasible, acceptable and has clinical effect on reducing opioid and other substance use.
At enrollment, majority were excluded due to lack of access to a phone. This percentage although high is similar to the pattern observed for mHealth interventions in other patient populations in Kenya where main reason for exclusion was lack of phone [100,101,102]. It could be partly related to the fact that the study enrolled participants who had current opioid use hence may have lost phones or not stable enough to maintain a phone. Also, there is a high phone turnover among individuals with OUD with some reporting to sell phones to buy drugs [47, 103, 104]. This shows a possible challenge that needs to be considered when designing similar interventions in the study population. Some studies assessing digital interventions among individuals with OUD have provided phones to participants [16] or provided access to computers at the clinic for patients, but this may not be applicable in our setting or for long-term treatment. An approach that can be used to circumvent this, is to also include participants with access to phone through other family members which is common in our setting [47]. This can be explored in future studies.
There was an overall reduction in opioid use among all the participants with greater proportion in the intervention group. Although no statistical difference was observed, these findings show promising effect of a digital intervention in OUD treatment. Similar findings have been reported in use of text message intervention among individuals with OUD although some studies are feasibility trials with short treatment duration ranging from seven to 28 days [105, 106]. In a study with a sample of 25 participants in each arm using a text-message CBT intervention among individuals with opioid and stimulant use, those in intervention group had lower odds of opioid use although the differences were not observed for other substances. Self-reported frequency of use was also lower at follow up compared to baseline [31]. These findings imply that a text message intervention can be used in individuals with OUD to improve outcomes.
The retention in treatment was 93.3% at 6 weeks and 83.3% at 3 months in the intervention arm of this study. This is similar to retention in treatment for individuals with OUD in previous studies [107]. This can be explained partly by the fact that treatment as usual meant participants come to the clinic daily for the methadone treatment hence were more likely to be notified of the follow up evaluation during the clinic visits. Although all the individuals lost to follow up were in the intervention group, reasons for the loss to follow were not identified. Of note however is that the loss to follow up was based on those not coming to the clinic for methadone treatment at three months follow up and therefore may not be related to the intervention.
Feasibility of using a text message intervention was demonstrated by high engagement and adherence in the intervention group. These results are comparable to other studies assessing use of digital interventions in OUD treatment [31, 32]. Of note is that in this study, engagement was based on response to homework questions during the study period. However, as noted above, the invite to respond to the follow-up questionnaire was sent by message and most participants responded. Also, two participants who had not responded to any message participated in the interviews and gave feedback on the intervention. This implies that although some participants did not respond to the questions, they read the messages and participated in the intervention. Future studies need to have strategies to assess use of intervention throughout the intervention period.
A higher response was noted at the start of the intervention and the final week compared to week 3, 4, and 5. On the other hand, when asked on preference for the modules, there was almost similar preference for all modules. This shows that different modules may appeal differently to participants. A similar pattern of use of intervention more at the start with reduced use over time is reported in other studies [28]. In the study by Glasner et al., [31] there was variable engagement reported depending on the type of response required for the messages e.g. an average response to 80% of text message that required yes or no, 48% to messages with multiple-choice questions and 57% of messages with open-ended questions. There was also variable utilization of additional features with the option for craving support having highest use. This shows response to the messages may be affected by requiring long responses for the weekly homework question. Also, variable response rate can arise due to habituation, response fatigue and perceived intrusive by participants [108]. This highlights the role of personalization in a text message intervention [109, 110].
Comparison done for response to homework based on status at enrollment showed that those who were being reinducted in treatment were more likely to respond to more questions. Past research shows that previous treatment attendance is associated with better outcomes for digital interventions [111, 112]. This can be related to motivation to remain abstinent or the current treatment enhances what was learnt in previous treatment. Also, those with smartphones provided more responses compared to regular phones. This shows that the interface of message display may affect the response rate which is a limitation of text message interventions [109]. These are factors that need to be considered in future studies.
Overall, there was good acceptability and satisfaction with the text message intervention. Majority of the participants found the intervention easy to use, intervention met their expectations and would recommend to a friend. In addition, duration and frequency of messages was reported as adequate. This is comparable to findings of studies on use of text message intervention for other substance [28, 113] and opioid use disorder [32, 114, 115]. This shows that a text message intervention is acceptable and can be implemented in the study population.
For the secondary outcomes, there was reduced use of other substances such as alcohol, cannabis and benzodiazepines although statistical significance was not assessed. This is similar previous research, as in one study on web-based intervention for OUD, there was no significant difference in effectiveness of the intervention based on primary substance of use [116]. This further shows promising effect of a text-message intervention in improving substance use outcomes since majority of individuals with OUD use multiple substances. In addition, drug-using self-efficacy improved following treatment with significant difference in the intervention arm. This is similar to a finding following use of a digital intervention among individuals with OUD [31, 117]. This is significant since higher self-efficacy is related to lower risk of substance use recurrence [118, 119].
A reduction in substance use was also observed in the control group. This can be explained by the fact that those in control group were receiving standard treatment which includes psychosocial treatment hence this may have influenced the results. The study findings may have also been influenced by factors observed in the study at baseline. These include: polysubstance use by majority, difference between participants in intervention and control groups based on age at first substance use, high risk score for opioid use on ASSIST and low to medium scores by majority in the readiness to change scale These factors need to be explored in future studies with large sample size to allow assessment of association between these factors and observed outcomes from the intervention.
Strengths and limitations
The strengths of this study include use of a CBT theory-based digital intervention approach in treatment for patients with OUD, with focus on a well-defined population comprising adults with OUD on methadone treatment and use of a control group that received active treatment which allowed for comparison on outcomes.
Limitations for this study include: first the study population was individuals with current opioid use hence limits the generalizability of the findings to other individuals with substance use disorders or those on methadone treatment but not currently using opioids. Second, there was lack of a control group that was matched for time and attention with the intervention group since text messages were only sent to the intervention group who were required to read and respond to the text message while the control received treatment as usual. Third, the short duration of intervention and follow up may have affected the outcomes observed. This has been cited as a limitation in previous studies on use of digital intervention in patients with SUD. However, this being a feasibility study, duration of treatment is among the factors that were assessed in the post treatment evaluation. Fourth, there was no blinding and most outcomes were self-reported and not objective, hence biases such as social desirability and recall bias might have occurred whereby those who knew they received the intervention (or even those who did not) might have reported a reduction in substance use without actually doing so. This is partly reflected in the difference between self-reported substance use and substance use based on UDS. Finally, due to the small sample size, this study may have not had enough power to allow detection of small effect from the text message intervention.
Conclusion
The study findings demonstrated that implementing a text-message intervention among individuals with OUD was feasible, the intervention was rated as acceptable and there was reduced opioid and other substance use post-intervention. Although the study was not powered to detect statistically significant difference, these findings have clinical implications that a text-message intervention can be used to provide/augment psychosocial treatment to individuals with OUD on methadone treatment with the potential to reduce opioid and other substance use and enhance self-efficacy.
In addition, there are implications for research. This was a feasibility trial hence further research is recommended with firstly using a larger sample powered to detect statistical difference and secondly with longer follow up period among participants with other substance use disorders without limitation at a methadone clinic to compare if there is a difference in effectiveness of the text-message intervention based on primary drug used.
Availability of data and materials
All data used and reported in this current study are available from the corresponding author upon reasonable request.
Abbreviations
- ASSIST:
-
Alcohol, smoking and substance involvement tool
- CBT:
-
Cognitive behaviour therapy
- CI:
-
Confidence interval
- CONSORT:
-
Consolidated standards of reporting trials
- CSQ:
-
Client satisfaction questionnaire
- DSM:
-
Diagnostic and statistical manual for mental Disorders
- DTCQ:
-
Drug taking confidence questionnaire
- HIV:
-
Human Immunodeficiency Virus
- IQR:
-
Inter-quartile range
- MAP:
-
Maudsley addiction profile
- MINI:
-
Mini International neuropsychiatric interview
- OR:
-
Odds Ratio
- OUD:
-
Opioid use disorder
- SOCRATES:
-
Stages of change, readiness and treatment eagerness scale
- SD:
-
Standard Deviation
- SUD:
-
Substance use disorder
- SUS:
-
System Usability Scale
- TLFB:
-
Timeline follow-back
- UDS:
-
Urine drug screen
- WHOQOLBREF:
-
World health organization quality of life short version instrument
References
United Nations office on drug and crime (UNODC). World drug report 2022: Global overview drug demand drug supply. United Nations Publ. 2022. Accessed at: https://www.unodc.org/unodc/en/data-and-analysis/world-drug-report-2022.html.
Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, et al. Series Drug Use 1 Global patterns of opioid use and dependence : harms to populations, interventions, and future action. Lancet. 2019;394(10208):1560–79. https://doi.org/10.1016/S0140-6736(19)32229-9.
Kurth AE, Cherutich P, Conover R, Chhun N, Bruce RD, Lambdin BH. The Opioid Epidemic in Africa And Its Impact. Curr Addict Rep. 2018;5(4):428–53.
Jaguga F, Kiburi SK, Temet E, Barasa J, Karanja S, Kinyua L, et al. A systematic review of substance use and substance use disorder research in Kenya. PLoS ONE. 2022;17:1–54. https://doi.org/10.1371/journal.pone.0269340.
Lelei K, Muteti J, Okioma V, Njega A. Extent of Heroin Use in Kenya. Afican J Alcohol Drug Abus. 2021;5:81–2.
Carley JA, Oesterle T. Therapeutic Approaches to Opioid Use Disorder : What is the Current Standard of Care ? Int J Gen Med. 2021;14:2305–11.
Ayanga D, Shorter D, Kosten TR. Update on pharmacotherapy for treatment of opioid use disorder. Expert Opin Pharmacother. 2016;17(17):2307–18. https://doi.org/10.1080/14656566.2016.1244529.
Sofuoglu M, Devito EE, Carroll K. Pharmacological and Behavioral Treatment of Opioid Use Disorder. Psych Res Clin Pr. 2019;1(1):4–15.
Dugosh K, Abraham A, Seymour B, Mcloyd K, Chalk M, Festinger D. A Systematic Review on the Use of Psychosocial Interventions in Conjunction With Medications for the Treatment of Opioid Addiction. J Addict Med. 2016;10(2):91–101.
Rice D, Corace K, Wolfe D, Esmaeilisaraji L, Michaud A, Grima A, et al. Evaluating comparative effectiveness of psychosocial interventions adjunctive to opioid agonist therapy for opioid use disorder : A systematic review with network. PLoS One. 2020;15(12):e0244401. https://doi.org/10.1371/journal.pone.0244401.
Zerden L, Guan T, Lombardi B, Sharma A, Garcia-Rico Y. Psychosocial Interventions in Office-Based Opioid Treatment: A Systematic Review. J Soc Soc Work Res. 2020;11(1):103–31.
United Nations Office on Drugs and Crime U and WHO. International standards for the treatment of drug use disorders: revised edition inorporating results of field testing. USA: SAS; 2020.
Wu L, Zhu H, Swartz MS, Sciences B, Policy F. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend. 2017;169:117–27.
Jones CM, Campopiano M, Baldwin G, Mccance-katz E. National and State Treatment Need and Capacity for Opioid Agonist Medication-Assisted Treatment. Am J Public Health. 2015;105(8):e55-63.
International Harm Reduction. Global State of Harm Reduction: 2019 updates. Harm Reduct Int. 2019;(November 2019):1–63. Available from: https://www.hri.global/global-state-of-harm-reduction-2019
Guarino H, Acosta M, Marsch L, Xie H, Aponte-Melendez Y. A Mixed-methods Evaluation of the Feasibility, Acceptability and Preliminary Efficacy of a Mobile Intervention for Methadone Maintenance Clients. Psychol Addict Behav. 2016;30(1):1–11.
Boumparis N, Schulte MHJ, Riper H. Digital Mental Health for Alcohol and Substance Use Disorders. Curr Treat Options Psych. 2019;6:352–66.
Goldberg S, Lam S, Simonsson O, Torous J, Sun S. Mobile phone-based interventions for mental health : A systematic meta-review of 14 meta- analyses of randomized controlled trials. PLOS Digit Heal. 2022;1(1):e0000002. https://doi.org/10.1371/journal.pdig.0000002.
Ferreri F, Bourla A, Mouchabac S, Karila L. e-Addictology : An Overview of New Technologies for Assessing and intervening in Addictive Behaviors. Front Psychiatry. 2018;9:51.
Kaner EFS, Beyer FR, Garnett C, Crane D, Brown J, Muirhead C, et al. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community ‐ dwelling populations. Cochrane Database Syst Rev. 2018;CD011479. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011479.pub2/full#0.
Ashford RD, Giorgi S, Mann B, Pesce C, Sherritt L, Ungar L, et al. Digital recovery networks: Characterizing user participation, engagement, and outcomes of a novel recovery social network smartphone application. J Subst Abuse Treat. 2020;109:50–5.
Erbe D, Eichert H, Riper H, Erbert D. Blending Face-to-Face and Internet-Based Interventions for the Treatment of Mental Disorders in Adults : Systematic Review. J Med Internet Res. 2017;19(9):e306.
Collins KM, Armenta RF, Cuevas-mota J, Liu L, Strathdee SA, Garfein RS, et al. Factors associated with patterns of mobile technology use among persons who inject drugs. Subst Abus. 2016;37(4):606–12.
Milward J, Day E, Wadsworth E, Strang J, Lynskey M. Mobile phone ownership, usage and readiness to use by patients in drug treatment. Drug Alcohol Depend. 2015;146:111–5. https://doi.org/10.1016/j.drugalcdep.2014.11.001.
Tofighi B, Chemi C, Ruiz-valcarcel J, Hein P, Hu L. Smartphone Apps Targeting Alcohol and Illicit Substance Use : Systematic Search in in Commercial App Stores and Critical Content Analysis Corresponding Author. JMIR mHealth uHealth. 2019;7(4):e11831.
Keoleian V, Polcin D, Galloway GP, Francisco S. Text messaging for addiction: A review. J Psychoact Drugs. 2016;47(2):158–76.
Watson T, Simpson S, Hughes C. Text messaging interventions for individuals with mental health disorders including substance use : A systematic review. Psychiatry Res. 2016;243:255–62. https://doi.org/10.1016/j.psychres.2016.06.050.
Noble JM, Vuong W, Surood S, Urichuk L, Greenshaw AJ, Agyapong VIO. Text4Support Mobile-Based Programming for Individuals Accessing Addictions and Mental Health Services — Retroactive Program Analysis at Baseline, 12 Weeks, and 6 Months. Front Psychiatry. 2021;12:640795.
Shalaby R, Adu MK, Gindi HM El, Agyapong VIO. Text Messages in the Field of Mental Health : Rapid Review of the Reviews. Front Pharmacol. 2022;13:921982.
Glasner S, Chokron Garneau H, Ang A, Ray L, Venegas A, Rawson R, et al. Preliminary Efficacy of a Cognitive Behavioral Therapy Text Messaging Intervention Targeting Alcohol Use and Antiretroviral Therapy Adherence: A Randomized Clinical Trial. PLoS ONE. 2020;15(3):e0229557.
Glasner S, Patrick K, Ybarra M, Reback CJ, Ang A, Kalichman S, et al. Promising outcomes from a cognitive behavioral therapy text-messaging intervention targeting drug use, antiretroviral therapy adherence, and HIV risk behaviors among adults living with HIV and substance use disorders. Drug Alcohol Depend. 2022;231:109229.
Langdon KJ, Scherzer C, Ramsey S, Carey K, Rich J, Ranney ML. Feasibility and acceptability of a digital health intervention to promote engagement in and adherence to medication for opioid use disorder. J Subst Abuse Treat. 2021;131:108538. https://doi.org/10.1016/j.jsat.2021.108538.
Carroll K. Therapy manuals for drug addiction: A cognitive-Behavioural Approach: Treating cocaine addiction. US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse; 1998. NIH Publication Number 98-4308.
Sudhir PM. Cognitive behavioural interventions in addictive disorders. Indian J Psychiatry. 2020;60(Suppl 4):s479–84.
Zamboni L, Centoni F, Fusina F, Mantovani E, Rubino F, Lugoboni F, et al. The Effectiveness of Cognitive Behavioral Therapy Techniques for the Treatment of Substance Use Disorders A Narrative Review of Evidence. J Nerv Ment Dis. 2021;209(11):835–45.
Pan S, Jiang H, Du J, Chen H, Li Z. Efficacy of Cognitive Behavioral Therapy on Opiate Use and Retention in Methadone Maintenance Treatment in China : A Randomised Trial. PLoS ONE. 2015;10(6):e0127598.
Zhuang S, An S, Zhao Y. Effect of cognitive behavioural interventions on the quality of life in Chinese heroin-dependent individuals in detoxification : a randomised controlled trial. J Clin Nurs. 2013;23:1239–48.
Verhey IJ, Ryan GK, Scherer N, Magidson JF. Implementation outcomes of cognitive behavioural therapy delivered by non - specialists for common mental disorders and substance - use disorders in low - and middle - income countries : a systematic review. Int J Ment Health Syst. 2020;14:40. https://doi.org/10.1186/s13033-020-00372-9.
Beck A, Nadkarni A, Calam R, Naeem F, Husain N. Increasing access to Cognitive Behaviour Therapy in Low and Middle Income Countries : A strategic framework. Asian J Psychiatr. 2016;22:190–5. https://doi.org/10.1016/j.ajp.2015.10.008.
Carroll K, Kiluk B. Cognitive Behavioral Interventions for Alcohol and Drug Use Disorders: Through the Stage Model and Back Again. Psychol Addict Behav. 2017;31(8):847–61.
Glasner-Edwards S, Patrick K, Ybarra ML, Reback CJ, Rawson RA, Garneau HC, et al. A Cognitive Behavioral Therapy – Based Text Messaging Intervention Versus Medical Management for HIV-Infected Substance Users : Study Protocol for a Pilot Randomized Trial. JMIR Res Protoc. 2016;5(2):e131.
Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, et al. Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. Am J Psychiatry. 2008;165(7):881–8.
Carroll K, Ball S, Martino S, Nich C, Babuscio TA, Rounsaville BJ. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: a 6-month follow-up of CBT4CBT. Drug Alcohol Depend. 2009;100(1–2):178–81.
Communications Authority of Kenya. First quarter sector statistics report for the financial year 2021 / 2022 ( July - September 2021 ). 2022;1–30. Available from: www.ca.go.ke
Kharono B, Kaggiah A, Mugo C, Seeh D, Guthrie BL, Moreno M, et al. Mobile technology access and use among youth in Nairobi , Kenya : implications for mobile health intervention design. mHealth, 2022;8:7. https://dx.doi.org/10.21037/mhealth-21-23.
Jennings Mayo-Wilson L, Kang BA, Mathai M, Mak’anyengo MO, Ssewamala FM. Mobile phone access, willingness, and usage for HIV-related services among young adults living in informal urban settlements in Kenya: A cross-sectional analysis. Int J Med Inform. 2022;161:104728. https://doi.org/10.1016/j.ijmedinf.2022.104728.
Kiburi SK, Paruk S, Chiliza B. Mobile phone ownership, digital technology use and acceptability of digital interventions among individuals on opioid use disorder treatment in Kenya. Front Digit Heal. 2022;4:975168.
Jennings L, Ong’Ech J, Simiyu R, Sirengo M, Kassaye S. Exploring the use of mobile phone technology for the enhancement of the prevention of mother-to-child transmission of HIV program in Nyanza, Kenya: A qualitative study. BMC Public Health. 2013;13(1):1131.
Gibson DG, Ochieng B, Kagucia EW, Were J, Hayford K, Moulton LH, et al. Mobile phone-delivered reminders and incentives to improve childhood immunisation coverage and timeliness in Kenya (M-SIMU): a cluster randomised controlled trial. Lancet Glob Heal. 2017;5(4):e428-38. https://doi.org/10.1016/S2214-109X(17)30072-4.
Oduor K, Ogweno S, Ajwang’ D, Okinyi N. Incorporating mhealth interventions into kenya’s health infrastructure to augment universal health coverage, service delivery improvement approach. South East Eur J Public Heal. 2021;2021(Special Issue 2):1–12.
Stocks J, Ibrahim S, Park L, Huchko M. Mobile Phone Ownership and Use Among Women Screening for Cervical Cancer in a Community-Based Setting in Western Kenya: Observational Study. JMIR Public Heal Surveill. 2022;8(6):e28885.
Ojeahere I, Kiburi S, Agbo P, Kumar R, Jaguga F. Telehealth interventions for substance use disorders in low- and- middle income countries : A scoping review. PLOS Digit Heal. 2022;1(11):e0000125. https://doi.org/10.1371/journal.pdig.0000125.
Harder VS, Musau AM, Musyimi CW, Ndetei DM, Mutiso VN. A Randomized Clinical Trial of Mobile Phone Motivational Interviewing for Alcohol Use Problems in Kenya. Addiction. 2019; https://doi.org/10.1002/central/CN-02050557/full
Musyoka CM, Mbwayo A, Donovan DM, Mathai M. Student peer mentoring : Feasibility and acceptability of mHealth-based tool for alcohol and substance abuse prevention by peer mentors at a university in Kenya. PLOS Digit Heal. 2023;2(1):e0000177. https://doi.org/10.1371/journal.pdig.0000177.
Rhodes T, Guise A, Ndimbii J, Strathdee S, Ngugi E, Platt L, et al. Is the promise of methadone Kenya’s solution to managing HIV and addiction? A mixed-method mathematical modelling and qualitative study. BMJ Open. 2015;5(3):e007198.
Mbogo LW, Sambai B, Monroe-wise A, Ludwig-barron NT, Guthrie BL, Bukusi D, et al. Participation in methadone programs improves antiretroviral uptake and HIV viral suppression among people who inject drugs in Kenya. J Subst Abuse Treat. 2022;134:108587. https://doi.org/10.1016/j.jsat.2021.108587.
Kiburi S, Ngarachu E, Mogaka B, Maina G. Sociodemographic, clinical profile and the association with retention in treatment among patients receiving methadone treatment in Nairobi, Kenya. Afr J Alcohol Drrug Abus. 2021;6:51–66.
Kiburi SK, Mwangi J, Maina G. Exploring the experiences of clients receiving opioid use disorder treatment at a methadone clinic in Kenya : a qualitative study. Addict Sci Clin Pract. 2022;17(71):1–11. https://doi.org/10.1186/s13722-022-00352-z.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for Implementation Research : Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm Policy Ment Heal. 2011;38(2):65–76.
Boumparis N, Karyotaki E, Schaub MP, Cuijpers P, Riper H. Internet interventions for adult illicit substance users : a meta-analysis. 2017. p. 1521–32.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ. 2016;355:i5239.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: (DSM-5). 5th ed. Arlington: American Psychiatric Association; 2013.
Onken LS, Carroll KM, Shoham V, Cuthbert BN. Reenvisioning Clinical Science: Unifying the Discipline to Improve the Public Health Lisa. Clin Psychol Sci. 2014;2(1):22–34.
Muench F, Weiss RA, Morgenstern J. Developing a theory driven text messaging intervention for addiction care with user driven content. Psychol Addict Behav. 2013;27(1):315–21.
Kiluk B, Nich C, Buck MB, Devore KA, Frankforter TL, Lapaglia DM, et al. Randomized Clinical Trial of Computerized and Clinician-Delivered CBT in Comparison With Standard Outpatient Treatment for Substance Use Disorders : Primary Within-Treatment and Follow-Up Outcomes. Am J Psychiatry. 2018;175(9):853–63.
Shi JM, Henry SP, Dwy SL, Orazietti SA, Carroll KM. Randomized pilot trial of Web-based cognitive-behavioral therapy adapted for use in office-based buprenorphine maintenance. Subst Abus. 2019;40(2):132–5.
Tetrault JM, Holt SR, Cavallo DA, O’Connor PG, Gordon MA, Corvino JK, et al. Computerized Cognitive Behavioral Therapy for Substance Use Disorders in a Specialized Primary Care Practice: a Randomized Feasibility Trial to Address the RT Component of SBIRT. J Addict Med. 2020;14(6):e303-9. https://doi.org/10.1002/central/CN-02123312/full.
Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat. 2005;4(4):287–91.
Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res. 2016;25(3):1057–73.
Peckham E, Brabyn S, Cook L, Devlin T, Dumville J, Torgerson DJ. The use of unequal randomisation in clinical trials - An update. Contemp Clin Trials. 2015;45:113–22. https://doi.org/10.1016/j.cct.2015.05.017.
Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. Pilot Study Article Need To Rename. BMC Med Res Methodol. 2010;10(1):1–10.
Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–9.
Humeniuk R, Ali RL. Validation of the Alcohol, Smoking and Substance Involvement Screening Test ( ASSIST ) and Pilot Brief Intervention : A Technical Report of Phase II Findings of the WHO ASSIST Project Prepared by Rachel Humeniuk & Robert Ali on behalf of the WHO ASSIST P. 2006. (January).
Mawia C, Id M, Mbwayo A, Donovan D, Mathai M. Alcohol and substance use among first-year students at the University of Nairobi, Kenya : Prevalence and patterns. 2020. p. 1–15.
Mokaya AG, Mutiso V, Musau A, Tele A, Kombe Y, Nganga Z, et al. Substance Use among a Sample of Healthcare Workers in Kenya: A Cross-Sectional Study. J Psychoactive Drugs. 2016;48(4):310–9. http://dx.doi.org/10.1080/02791072.2016.1211352.
Robinson S, Sobell LC, Sobell MB, Leo G. Reliability of the Timeline Followback for cocaine, cannabis and cigarette use. Psychol Addict Behav. 2012;1–11. https://doi.org/10.1037/a0030992.
Sobell LC, Brown J, Leo GI, Sobell MB. The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug Alcohol Depend. 1996;42:49–54.
Fals-stewart W, Farrell TJO, Freitas TT, Mcfarlin SK, Rutigliano P. The Timeline Followback Reports of Psychoactive Substance Use by Drug-Abusing Patients : Psychometric Properties. J Consult Clin Psychol. 2000;68(1):134–44.
Giusto A, Green EP, Simmons RA, Ayuku D, Patel P, Puffer ES. A multiple baseline study of a brief alcohol reduction and family engagement intervention for fathers in Kenya. J Consult Clin Psychol. 2020;88(8):708–25.
Papas RK, Sidle JE, Gakinya BN, Baliddawa JB, Martino S, Mwaniki MM, et al. Treatment outcomes of a stage 1 cognitive-behavioral trial to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction. 2011;106(12):2156–66.
Sheehan D, Lecrubier Y, Sheehan K, Janavs J, Weiljer E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview ( MINI ) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12:232–41.
Kwobah E, Epstein S, Mwangi A, Litzelman D, Atwoli L. Prevalence of psychiatric morbidity in a community sample in Western Kenya. BMC Psychiatry. 2017;17:30.
Khasakhala LI, Ndetei DM, Mathai M, Harder V. Major depressive disorder in a Kenyan youth sample: relationship with parenting behavior and parental psychiatric disorders. Ann Gen Psychiatry. 2013;12(1):15.
Marsden J, Gossop M, Stewart D, Best D, Farrell M, Lehmann P, et al. The Maudsley Addiction Profile ( MAP ): a brief instrument for assessing treatment outcome. Addiction. 1998;93(12):1857–68.
Marsden J, Corbelli C. New European Instruments for Treatment Outcome Research : Reliability of the Maudsley Addiction Profile and Treatment Perceptions Questionnaire in Italy, Spain and Portugal. 2000. p. 115–22.
Dannatt L, Chb MB, Cloete KJ, Kidd M, Weich L, Chb MB. Frequency and correlates of comorbid psychiatric illness in patients with heroin use disorder admitted to Stikland Opioid Detoxification Unit, South Africa. S Afr J Psychiatr. 2014;20(3):77–82.
Skevington SM, Lotfy M, O'Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment : Psychometric properties and results of the international field trial. A Report from the WHOQOL Group. Qual Life Res. 2004;299–310. https://doi.org/10.1023/B:QURE.0000018486.91360.00.
Strada L, Vanderplasschen W, Buchholz A, Schulte B. Measuring quality of life in opioid-dependent people : a systematic review of assessment instruments. Qual Life Res. 2017;26(12):3187–200.
Kinyanjui DWC, Kathuku DM, Mburu JM. Quality of life among patients living with epilepsy attending the neurology clinic at kenyatta national hospital, Nairobi, Kenya : a comparative study. Health Qual Life Outcomes. 2013;11(1):1 (Available from: Health and Quality of Life Outcomes).
Sklar S, Annis HM, Turner NE. Development and validation of the Drug-taking confidence Questionnaire: A measure of coping self efficacy. Addict Behav. 1997;22(5):655–70.
Miller WR, Tonigan JS. Assessing Drinkers ’ Motivation for Change : The Stages of Change Readiness and Treatment Eagerness Scale ( SOCRATES ). Psychol odf Addict Behav. 1996;10(2):81–9.
De WEF, Hendriks M. The Client Satisfaction Questionnaire : Psychometric Properties in a Dutch Addict Population. Eur Addict Res. 2005;11:157–62.
Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: Development of a general scale. Eval Program Plann. 1979;2:197–207.
Lewis JJR. Revisiting the Factor Structure of the System Usability Scale. J Usability Stud. 2017;12(4):183–92.
Holdsworth E, Bowen E, Brown S, Howat D. Client engagement in psychotherapeutic treatment and associations with client characteristics, therapist characteristics, and treatment factors. Clin Psychol Rev. 2014;34(5):428–50. https://doi.org/10.1016/j.cpr.2014.06.004.
Simpson DD, Joe GW. A longitudinal evaluation of treatment engagement and recovery stages. J Subst Abuse Treat. 2004;27(2):89–97.
Borghouts J, Eikey E, Mark G, De Leon C, Schueller SM, Schneider M, et al. Barriers to and facilitators of user engagement with digital mental health interventions: Systematic review. J Med Internet Res. 2021;23(3):e24387.
Sieverink F, Kelders SM, Gemert-Pijnen V. Clarifying the concept of adherence to ehealth technology: Systematic review on when usage becomes adherence. J Med Internet Res. 2017;19(12):1–16.
Flett JAM, Fletcher BD, Riordan BC, Patterson T, Hayne H, Conner TS. The peril of self-reported adherence in digital interventions: A brief example. Internet Interv. 2019;18(August):100267. https://doi.org/10.1016/j.invent.2019.100267.
Nordberg B, Mwangi W, Van Der Kop ML, Were E, Kaguiri E, Kågesten AE, et al. The effect of weekly interactive text - messaging on early infant HIV testing in Kenya : a randomised controlled trial ( WelTel PMTCT ) Academic Model Providing Access to Healthcare. Sci Rep. 2021;11:22652. https://doi.org/10.1038/s41598-021-00972-6.
Jones RM, Kimenju G, Subbiah S, Styles A, Pearson N, Rajasekharan S. A Short Message Service ( SMS ) increases postpartum care-seeking behavior and uptake of family planning of mothers in peri- urban public facilities in Kenya. PLoS One. 2020;15(9):e0239213. https://doi.org/10.1371/journal.pone.0239213.
Odeny B, McGrath CJ, Langat A, Pintye J, Singa B, Kinuthia J, et al. Male partner antenatal clinic attendance is associated with increased uptake of maternal health services and infant BCG immunization: a national survey in Kenya. BMC Pregnancy Childbirth. 2019;19(1):284.
Milward J, Day E, Wadsworth E, Strang J, Lynskey M. Mobile phone ownership, usage and readiness to use by patients in drug treatment. Drug Alcohol Depend. 2015;146:111–5.
McClure EA, Acquavita SP, Harding E, Stitzer ML. Utilization of communication technology by patients enrolled in substance abuse treatment. Drug Alcohol Depend. 2013;129(1–2):145–50.
Schuman-Olivier Z, Borodovsky JT, Steinkamp J, Munir Q, Butler K, Greene MA, et al. MySafeRx : a mobile technology platform integrating motivational coaching, adherence monitoring, and electronic pill dispensing for enhancing buprenorphine / naloxone adherence during opioid use disorder treatment : a pilot study. Addict Sci Clin Pract. 2018;31:21. https://doi.org/10.1186/s13722-018-0122-4.
Suffoletto B, Yanta J, Kurtz R, Cochran G, Douaihy A, Chung T. Acceptability of an Opioid Relapse Prevention Text-message Intervention for Emergency Department Patients. J Addict Med. 2017;11(6):475–82.
Ruadze E, Todadze K. Retention in Georgia opioid substitution therapy program and associated factors. Harm Reduct J. 2016;13(35):1–9. https://doi.org/10.1186/s12954-016-0124-z.
MacDougall S, Jerrott S, Clark S, Campbell L, Murphy A, Wozney L. Text Message Interventions in Adolescent Mental Health and Addiction Services : Scoping Review. JMIR Ment Heal. 2021;8(1):e16508.
Suffoletto B. Text Message Behavioral Interventions : From Here to Where ? Curr Opin Psychol. 2016;1(9):16–21.
Tofighi B, Nicholson JM, Mcneely J, Muench F, Lee JD. Mobile phone messaging for illicit drug and alcohol dependence: A systematic review of the literature. Drug Alcohol Rev. 2017;36(4):477–91.
Christensen DR, Landes RD, Jackson L, Marsch LA, Mancino MJ, Chopra MP, et al. Adding an Internet-delivered treatment to an efficacious treatment package for opioid dependence. J Consult Clin Psychol. 2014;82(6):964–72.
Kim SJ, Marsch LA, Acosta MC, Guarino H, Aponte-Melendez Y. Can persons with a history of multiple addiction treatment episodes benefit from technology delivered behavior therapy? A moderating role of treatment history at baseline. Addict Behav. 2016;54:18–23. https://doi.org/10.1016/j.addbeh.2015.11.009.
Mason MJ, Zaharakis NM, Russell M, Childress V. A pilot trial of text-delivered peer network counseling to treat young adults with cannabis use disorder. J Subst Abuse Treat. 2018;89:1–10.
Kathuria H, Shankar D, Cobb V, Newman J, Bulekova K. Integrating Social Determinants of Health With Tobacco Treatment for Individuals With Opioid Use Disorder : Feasibility and Acceptability Study of Delivery Through Text Messaging. JMIR Form Res. 2022;6(9):e36919.
Tofighi B, Grazioli F, Bereket S, Grossman E, Aphinyanaphongs Y, Lee JD. Text Message Reminders for Improving Patient Appointment Adherence in an Of fi ce-Based Buprenorphine Program : A Feasibility Study. Am J Addict. 2017;26:581–6.
Cochran G, Stitzer M, Campbell ANC, Hu M-C, Vandrey R, Nunes EV. Web-based treatment for substance use disorders: differential effects by primary substance. Addict Behav. 2015;45:191–4.
Hodges J, Waselewski M, Harrington W, Franklin T, Schorling K, Huynh J, et al. Six ‑ month outcomes of the HOPE smartphone application designed to support treatment with medications for opioid use disorder and piloted during an early statewide COVID ‑ 19 lockdown. Addict Sci Clin Pract. 2022;1–11. https://doi.org/10.1186/s13722-022-00296-4
Kadden R, Litt MD. The role of self-efficacy in the treatment of substance use disorders. Addict Behav. 2011;36(12):1120–6.
Hayaki J, Conti MT, Bailey GL, Herman DS, Anderson BJ, Stein MD. Negative affect-associated drug refusal self-efficacy, illicit opioid use, and medication use following short-term inpatient opioid withdrawal management. J Subst Abuse Treat. 2021;126:108309. https://doi.org/10.1016/j.jsat.2021.108309.
Funding
The authors report no external funding for this study.
Author information
Authors and Affiliations
Contributions
SKK was in the study conception and design, acquisition, analysis and interpretation of data and drafting and revising the manuscript. SP and BC were involved in design, interpretation of data, drafting and revising the manuscript. EKK was involved in interpretation of data and revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods in this study were performed in accordance with the Declaration of Helsinki. Ethical approval was obtained from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal and Kenyatta National Hospital/University of Nairobi ethics review committee. Participation in the study was voluntary and written informed consent was obtained from the participants prior to enrolling in the study.
Consent to publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1
. Table showing a summary of schedule for the outcome assessments during the study period. Appendix 2. Participant responses on system usability, acceptability and satisfaction with the intervention – with details for each score category. Appendix 3. Figure showing the comparison of response to weekly homework based on status at enrollment. Appendix 4. Figure showing the comparison of response to weekly homework based on type of phone (smartphone versus regular phones).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kiburi, S.K., Kwobah, E.K., Paruk, S. et al. Feasibility, acceptability and preliminary efficacy of a cognitive behavior therapy text-message intervention among individuals with opioid use disorder in Kenya: a randomized feasibility trial. BMC Digit Health 1, 14 (2023). https://doi.org/10.1186/s44247-023-00014-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44247-023-00014-3