Abstract
Background
Physical activity, sedentary behaviour, and sleep are key components to health and well-being. Compositional data analysis of activity data overcomes the limitations of traditional statistical approaches and comprehensively assesses the association of all activities throughout a 24-hour day. Few studies have used compositional analysis to explore associations between movement behaviours and mental health. This study examined the association between 24-hour activity compositions and mental health in middle-aged Australian adults.
Methods
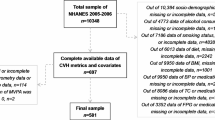
This study used cross-sectional data from participants (n = 322; mean age 40.4 years; 58.1% female; 47.8% university degree; 84.8% partnered) in the longitudinal Annual Rhythms in Adults’ lifestyle and health study (Adelaide, Australia). Activity composition (sleep, sedentary behaviour, light physical activity, and moderate-to-vigorous physical activity) was derived using 24-hour Fitbit accelerometry from the first month of participation (December). Mental health outcomes (depression, anxiety, and stress) were obtained from the Depression Anxiety Stress Scale 21-item short-form (DASS-21). The associations between activity composition (conveyed as isometric log ratios) and DASS-21 scores were examined using compositional multi-level linear regression models with a random intercept for clustering of individuals within families. Using the compositional time reallocation model, expected differences in mental health were examined for hypothetical time reallocations between individual activities.
Results
Favourable associations were observed when time (15 min) was reallocated to light physical activity from sleep (depression: -0.31 [95% CI=-0.57: -0.06]; anxiety: -0.20 [95% CI=-0.37: -0.03] and from sedentary behaviour (depression: -0.29 [95% CI=-0.46: -0.13]; anxiety: -0.14 [95% CI=-0.25: -0.03]; stress: -0.16 [95% CI=-0.31: -0.01]). Detrimental associations were observed when time was reallocated away from light physical activity to sleep (depression: 0.32 [95% CI = 0.07: 0.58]; anxiety: 0.20 [95% CI = 0.03: 0.37]) and to sedentary behaviour (depression: 0.30 [95% CI = 0.13: 0.48); anxiety: 0.15 [95% CI = 0.03: 0.26]; stress: 0.17 [95% CI = 0.01: 0.32]). There were no associations when time was allocated to or from moderate-to-vigorous physical activity.
Conclusion
The way adults spend their time across a 24-hour day is associated with their mental health. Spending more time in light physical activity appears favourable if this time is taken from sleep and sedentary behaviour. These findings provide support for “move more, sit less” public health messages.
Trial registration
This study was prospectively registered on the Australian New Zealand Clinical Trial Registry (Trial ID: ACTRN12619001430123) on the 16/10/2019.
Similar content being viewed by others
Background
Mental health disorders are one of the leading causes of the global health-related burden, with substantial costs to individuals and society [1, 2]. One in eight people worldwide were affected by a mental health disorder in 2019 [3], and 44% experience a mental health disorder in their lifetime [4, 5]. Anxiety is the most prevalent mental health disorder [3], and depression is the leading cause of mental health-related disease burden [6]. Furthermore, the worldwide prevalence of stress and distress ranges between 35 and 38% [7,8,9]. Overall, the annual global costs of mental health disorders is an estimated $2.5 trillion, and this is projected to increase to $6 trillion by 2030 [10].
Physical activity, sedentary behaviour, and sleep each impact the overall health and wellbeing of individuals [11,12,13]. Higher physical activity and adequate amounts of sleep are consistently associated with improved mental health [14,15,16,17,18,19], while excessive sedentary behaviour can adversely affect mental health and may increase the risk of future chronic diseases [20,21,22,23,24]. Yet, only 17% of Australian adults meet the national physical activity guidelines [25, 26] and 40%, have difficulty achieving recommended levels of sleep of seven to nine hours a night [27, 28]. Furthermore, 70% of Australian adults spend more than 4 h per day sitting [29], and 40% of their waking time was spent online in 2020 (a 10% increase from 2019 [30]).
To date, most studies have evaluated physical activity, sedentary behaviour, and sleep as independent factors impacting mental health. Yet, these behaviours are not truly independent factors. There are always 24-hours within a day, so if time spent in one activity increases, time in another must decrease [31]. Therefore, evaluating the whole 24-hour day is important to comprehensively understand the association between activity compositions (physical activity, sedentary behaviour, and sleep) and mental health. Until recently, studies generally did not examine the whole 24-hour day since the variables are perfectly multi-collinear [32]. Perfect multi-collinearity indicates perfect linear relationships between multiple variables. The issue of perfect multi-collinearity can be overcome through compositional data analysis (CoDA); a statistical approach which has relatively recently been applied in behavioural research [31]. The use of CoDA with activity data allows a comprehensive assessment of the association of all daily activities and mental health. CoDA expresses the 24-hour (1440-minute) data as a set of isometric log ratios constructed to represent all relative information about the activity data, whilst avoiding perfect multi-collinearity [33]. Interpretation of compositional models is relative; changes in one activity are always accompanied by changes in one or more other activities. Effect sizes can be expressed in terms of time reallocations, such as how much mental health is estimated to differ when time is reallocated from one activity to another within the daily composition.
Few studies have used CoDA to analyse the associations between daily activities and mental health in adults. Findings from these studies have reported that reallocating from time at work to time spent sleeping or undertaking physical activity is associated with improved mental health [33], and that reallocating time from sedentary behaviour and light physical activity to moderate-to-vigorous physical activity or sleep is associated with decreased anxiety [34]. In contrast, other studies have reported no significant associations between changes in activity compositions and mental health [35, 36]. However, limitations of previous work include the use of self-report measures of activity compositions [33] (which may introduce recall or social desirability bias), and the focus on specific populations including retiring older adults [33], adult office workers [35], adults with chronic obstructive pulmonary disease (COPD) [34] and young and middle-aged adults [36]. The way adults spend their time in physical activity, sedentary behaviour, and sleep may have important implications for their mental health, yet further research is required to explore these associations among more representative samples whilst incorporating objective measures of 24-hour activity compositions. Therefore, the aims of this study were to use CoDA to evaluate how objectively measured 24-hour physical activity, sedentary behaviour, and sleep were associated with symptoms of depression, anxiety, and stress among middle-aged adults.
Methods
Design
The study used data from a prospective cohort study named “Annual Rhythms in Adults’ lifestyle and health” (ARIA), which examined changes in daily activity patterns, diet, weight, and mental health symptoms in adults across a year [37]. The ARIA study was approved by the University of South Australia Human Research Ethics Committee (Protocol number: 201,901). Participants provided informed and written consent before beginning the study. The study was registered on the Australian New Zealand Clinical Trial Registry (Trial ID: ACTRN12619001430123).
Participants and procedure
The ARIA study consisted of a sample of 375 adults recruited in three waves from greater metropolitan Adelaide, South Australia, who were followed for 13 months. Waves one and two were parents and guardians of children partaking in an ongoing children’s cohort study, named the “Life on Holidays” study, recruited in SES strata [38]. Wave three were parents of primary school-aged children recruited from the general population using Facebook posts and advertisements, and through referrals from existing participants. Wave three participants were purposively sampled to address sample imbalances from waves one and two (i.e. wave three emphasised the recruitment of lower SES and male participants). ARIA wave one participants commenced in December 2019, and wave two and three participants commenced in December 2020.
Inclusion criteria were: 18 to 64 years of age, residing in greater metropolitan Adelaide, South Australia, access to a Bluetooth-enabled phone, tablet, desktop computer, or laptop, internet access, parent/guardian of a child involved in the “Life on Holidays” study (or parent/guardian of a primary school-aged child for wave three), ambulant, and able to read English. Exclusion criteria were: an implanted electronic medical device, pregnancy, having a life-threatening or serious illness that impacted daily lifestyles.
A baseline face-to-face home visit was conducted prior to the start of data collection. During the home visit, participants were provided with a Fitbit Charge 3, a Fitbit Aria 2 smart body weight scale or a Fitbit Aria Air scale (Fitbit Inc., San Francisco, CA, USA) and a weigh-in reminder flyer. During the home visit, participant’s height was calculated to the nearest 0.1 cm using a stadiometer (Leicester Height Measure MKII, England) following the International Society for the Advancement of Kinanthropometry assessment procedures [39]. In addition, participants completed an online or paper baseline survey regarding their work status, family structure, household characteristics, and demographic information (age, sex, income, and education). Online surveys (delivered using Survey Monkey software) were used to capture diet and mental health at eight time points throughout the year (December, January, March, April, June, August, October, and December). Participants were provided with a $100 honorarium at study completion and were allowed to keep their Fitbit equipment. For the secondary analysis presented here, mental health data were obtained from the January survey (which recalled December) and 24-hour activity data were from the Fitbit data recorded in the first December period (December 2019 for wave one, and December 2020 for waves two and three).
Variables
Demographics. Participants self-reported their date of birth, sex, marital status (never married, widowed, divorced, separated but not divorced, married or de facto), highest education level (year 12 or lower, certificate III/IV, diploma, advanced diploma, bachelor, postgraduate, or higher degree), household gross income (AU$; <$50,000, $50,000-$99,999, $100,000-$199,999, >$200,000), and current smoking status (yes, no).
Body weight. Body weight was assessed by the Fitbit Aria smart scales. Bodyweight measures using the Fitbit Aria have shown to be within ≤ 0.5 kg compared with a certified scale in healthy adults [40]. Participants were asked to weigh themselves at the same time each day, preferably in the morning after voiding, wearing minimal clothing, and before eating or drinking. Data were synced to the participants’ Fitbit accounts and were gathered remotely by the purpose-built research software called Fitnesslink, developed by Portal Australia for the ARIA study. The first valid weigh-in (i.e., on, or after 1st December) was used to calculate body mass index.
Activity compositions. Daily minutes of sleep, sedentary behaviour, light physical activity, and moderate-to-vigorous physical activity were derived from Fitbit Charge 3 fitness trackers. Participants continuously wore the Fitbit Charge 3 on their non-dominant wrist for 24 h a day over 13 months, including whilst sleeping but excluding when undertaking water-based activities or when charging the tracker. The first month of activity data (December) was used for the analysis. One month of data was chosen to match the survey time frame, which asked about activities and mental health in the last month. Various Fitbit models have shown acceptable reliability and validity for sleep (Fitbit Charge 2 compared to polysomnography 0.61 specificity and 0.96 sensitivity [41, 42]), moderate-to-vigorous physical activity (Fitbit Flex compared to Actigraph GT3X + r = 0.73 [43]), sedentary time (Fitbit Charge 3 compared to activPAL: ICC = 0.94, 95% CI: 0.92–0.96 [44]), and total daily energy expenditure (Fitbit Flex assessed against doubly labelled water in free-living conditions r = 0.33 [45]). Data captured from the Fitbit tracker were synced to the participants’ Fitbit accounts and were gathered remotely via the Fitnesslink software.
Each minute of the day was classified as one of five activities: sleep, sedentary, light, moderate, or vigorous physical activity by Fitbit’s proprietary algorithm. Daily moderate-to-vigorous physical activity was totalled as the number of minutes spent in moderate and vigorous activity. Minutes determined as sedentary (logged when other activities were not identified) and with absent heart rate data were classified as non-wear. Valid days were characterised as a minimum of 18 h wear time including a sleep period. Only participants who had at least three weekdays and one weekend day in the first December of valid data were included in the analysis [46].
Mental health. Symptoms of depression, anxiety, and stress were assessed using the DASS-21 [47]. The DASS-21 is a 21-item questionnaire addressing the areas of stress, anxiety, and depression felt over the past month by participants. Participants responded with answers ranging from zero “did not apply to me at all” to three “applied to me very much, or most of the time”. As recommended, to enable comparability with the DASS-42 long version, the DASS-21 raw scores were doubled. The DASS-21 has demonstrated validity and reliability (Cronbach’s alpha 0.82–0.90 for all three subscales [48,49,50]).
Statistical analysis
Means and standard deviations were used to represent DASS-21 scores for the pooled sample. The average daily activity composition of sleep, sedentary behaviour, light physical activity, and moderate-to-vigorous physical activity were described using compositional means (geometric means of each activity composition, adjusted linearly so that collectively the behaviours amounted to 1440 min). The associations between activity composition (conveyed as isometric log ratios) and DASS-21 depression, anxiety and stress scores were examined using compositional multi-level linear regression models with a random intercept to account for clustering of individuals within families. Using a cross-sectional compositional time reallocation model conducted in R version 4.1.0 using the compositions package, expected differences in mental health were examined for time reallocations between individual activities [36]. All models were tested for outlying observations, normality, linearity, and homoscedasticity of residuals to ensure assumptions were not violated. Covariates included sex, age, and education. Model-based dose-response curves quantified the expected difference in mental health for time reallocations between activities (e.g., increasing sleep by 20 min by reducing sedentary behaviour by 20 min). Descriptive analyses were carried out in SPSS (V.25, International Business Machines Corporation, New York, NY, USA).
Results
Demographics
A total of 322 participants had valid DASS-21 and activity data and were therefore included in the analysis. Participant baseline characteristics are shown in Table 1. Participants comprised of 58.1% females, with an average age of 40.4 years (standard deviation, SD = 5.9 years), were mainly non-smokers (91.9%), and had an average BMI of 28.7 kg/m2 (SD = 6.2). Participants were mostly well educated (47.8% bachelor, postgraduate, or higher degree), partnered (84.8% married or de facto), and approximately half had an overall household income of between AU$100,000 and AU$199,999 (47.7%) (Table 1). Participants had an average of 25 valid days of accelerometry data (SD 6, range 6–31) with an average of 23.1 h of wear time (SD 1.3, range 18.0–24.0). On average, participants spent approximately seven and a half hours per day sleeping, ten hours per day sedentary, five hours per day undertaking light physical activity, and half an hour per day undertaking moderate-to-vigorous physical activity at baseline.
Associations between activity compositions and mental health
Estimated differences and 95% confidence intervals in DASS scores associated with reallocations between individual activities are shown in Table 2. Favourable associations were observed when time (15 min) was reallocated to light physical activity from sleep (depression: -0.31 [95% CI=-0.57: -0.06]; anxiety: -0.21 [95% CI=-0.37: -0.03] and from sedentary behaviour (depression: -0.29 [95% CI=-0.46: -0.13]; anxiety: -0.14 [95% CI=-0.25: -0.03]; stress: -0.16 [95% CI=-0.31: -0.01]). Detrimental associations were observed when time was reallocated away from light physical activity to sleep (depression: 0.32 [95% CI = 0.07: 0.58]; anxiety: 0.20 [95% CI = 0.03: 0.37]) and to sedentary behaviour (depression: 0.30 [95% CI = 0.13: 0.48); anxiety: 0.15 [95% CI = 0.03: 0.26]; stress: 0.17 [95% CI = 0.01: 0.32]). Reallocating time to or from moderate-to-vigorous intensity physical activity was not associated with depression, anxiety or stress.
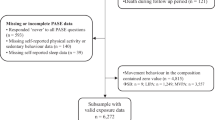
The expected differences in DASS (a) depression, (b) anxiety, and (c) stress scores for reallocations of time between sleep, light physical activity, and sedentary behaviour, keeping the other activities constant, at the mean composition, is shown in Fig. 1. Reallocations with sleep and sedentary behaviour are shown as separate lines. Negative values on the x-axis indicate time taken away from light physical activity and reallocated to sleep or sedentary behaviour, while positive values on the x-axis indicate time taken away from sleep or sedentary behaviour and reallocated to light physical activity. Reallocations from sleep and sedentary behaviour to light physical activity were associated with reduced depression scores, whereas reallocations from light physical activity to sleep and sedentary behaviour were associated with higher depression scores. The estimated dose-response curves were relatively linear. Reallocations from light physical activity and sedentary behaviour to sleep were associated with increased anxiety and stress scores, whereas reallocations from sleep to light physical activity and sedentary behaviour were associated with reduced anxiety and stress scores. The estimated dose-response curves were relatively linear.
Estimated differences in DASS (a) depression, (b) anxiety, and (c) stress scores (y-axis), associated with reallocations of time spent in light physical activity (x-axis). Note: LPA = light physical activity, SB = sedentary behaviour. Adjusted for age, sex, and highest education. Reallocations between light physical activity and sleep were not significant for stress and are therefore not shown
Discussion
This study evaluated the association between 24-hour activity compositions and mental health in middle-aged adults. Compositional time reallocation analysis suggested that reallocating time to light physical activity from sleep and sedentary behaviour was associated with lower depression, anxiety, and stress. In addition, reallocating time to more sedentary behaviour and more sleep from light physical activity was associated with poorer mental health. Reallocating time to or from moderate-to-vigorous physical activity had no association with depression, anxiety or stress.
The present findings showed that reallocating more time to light physical activity was associated with improved depression, anxiety and stress. These findings are consistent with findings from previous experimental and observational research, which indicate that higher amounts of light, or low intensity, physical activity are associated with improved mental health outcomes in healthy adults [51,52,53]. Furthermore, our findings are consistent with previous studies using traditional isotemporal substitution analyses [16] and CoDA analyses [33], which found improved mental health outcomes when time spent sleeping was reallocated to light physical activity [16], and when time spent in sedentary behaviour was reallocated to physical activity [33]. These findings provide support for current national activity recommendations or public health messages such as “move more, sit less”. However, in contrast to previous findings [54, 55], our present findings suggested that moderate-to-vigorous physical activity was not associated with improved mental health outcomes. For example, Nakagawa et al. found that reallocating time to moderate-to-vigorous physical activity (assessed using self-report) was associated with improved mental health symptoms, including depression, anxiety, and stress among young adults [54]. Differences in our findings, compared with previous findings may be attributed to the different samples (middle age versus young adults only) and different methods to assess physical activity (objective versus self-report).
In particular, we collected activity data using Fitbit fitness trackers, and the findings showed that, on average, participants undertook approximately half an hour of moderate-to-vigorous physical activity per day. Previous studies have used fitness trackers or accelerometers from a variety of manufacturers to measure activity compositions. In addition, varying cut points have been used to determine time spent in energy expenditure bands, resulting in different classifications. For example, in a study looking at participants with COPD, participants undertook approximately 90 min of moderate-to-vigorous physical activity a day [34]. It appears that the Fitbit algorithms may have a higher cut point for defining activity therefore underestimating moderate-to-vigorous intensity compared to research accelerometers [56]. This may explain why significant associations were detected for light physical activity but not moderate-to-vigorous intensity physical activity in our study.
Our findings showed that reallocating more time towards sleep was associated with worse mental health. This finding may be considered unexpected, and there is a general understanding that more sleep is beneficial [12, 57]. For example, Olds et al. found that older adults in retirement slept for seven to nine hours a night on average and increased sleep durations were associated with improved mental health [33]. However, previous studies have found that sleeping for greater than nine hours a night is associated with poorer mental health outcomes [57,58,59]. On average, participants in the present study slept for approximately seven and a half hours a night, which sits within recommended guidelines [28]. It is possible that there is an optimal sleep duration, beyond which the mental health associations become detrimental (i.e., an inverted U-shaped relationship). Further research among participants that are sleep deprived may produce different results. Alternatively, given the cross-sectional nature of the analysis, the results may be explained by reverse causation, whereby having poorer mental health leads to longer sleep durations.
This study has a number of strengths. It is one of the first studies to analyse the association between activity compositions and mental health using CoDA, thus contributing to the growing evidence in this area. The activity data were collected using activity trackers, therefore minimising the risk of recall and selection bias [33, 34]. This study used a 24-hour wear protocol with a threshold of 18 h to define a valid day and 4 days of data, including a weekend day, for inclusion in the analysis. This resulted in a large volume of data, with included participants having an average of 25 valid days of data with 23 h of data per day. We note, however, that there could still be systematic errors given that wear time may be less complete during certain times of the day or on certain days.
Limitations of this work include the cross-sectional design, therefore limiting the ability to infer causality of associations. Fitbits may use different cut points to classify activities than research accelerometers, making comparison of results more difficult. Participants were residents of the greater Adelaide region and had relatively high educational attainment and income, therefore the generalisability of these findings to other populations is unclear. Furthermore, the sample’s stress, anxiety, and depression scores were generally within normal ranges. It is likely that results may be different among samples with worse mental health outcomes. We note that data for wave 2 and 3 participants were collected during the COVID-19 pandemic. At this time, there were some continuing restrictions in Adelaide, Australia, including international travel restrictions and density restrictions in public venues, which may have affected participants’ activity and mental health, though participants’ daily lives were relatively unrestricted compared to most countries.
Future research evaluating the longitudinal associations between daily activity compositions and mental health would provide further information about the potential direction of the observed relationships. Additionally, research in different population, such as adults with more symptoms of depression, anxiety and stress or diagnosed mental health disorders, is needed.
In conclusion, this study examined how activity compositions were associated with mental health in a sample of middle-aged adults from Adelaide, Australia. The 24-hour activity compositions (sleep, sedentary behaviour, light physical activity, moderate-to-vigorous physical activity) were associated with symptoms of depression, anxiety, and stress. Reallocation of time to light physical activity from sleep or sedentary behaviour was associated with the most beneficial associations with mental health. Findings suggest that among healthy adults, encouraging more light physical activity may help optimise mental health.
Data Availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARENA:
-
Alliance for Research in Exercise, Nutrition and Activity
- ARIA:
-
Annual Rhythms in Adults’ lifestyle and health
- CoDA:
-
Compositional data analysis
- COPD:
-
Chronic obstructive pulmonary disease
- DASS:
-
Depression Anxiety Stress Scale
- HREC:
-
Human Research Ethics Committee
- NHMRC:
-
National Health and Medical Research Council
References
World Health Organization. Depression and other common mental disorders: global health estimates. World Health Organization. 2017. https://apps.who.int/iris/handle/10665/254610. License: CC BY-NC-SA 3.0 IGO.
Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, Abbafati C, Adolph C, Amlag JO, Aravkin AY, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312):1700–12.
Institute for Health Metrics and Evaluation., Global Health Data Exchange 2019: University of Washington; 2022.
Australian Bureau of Statistics. National Survey of Mental Health and Wellbeing: summary of results 2007. Australian Government; 2022. https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/2007.
Australian Bureau of Statistics. National Study of Mental Health and Wellbeing, 2021 – 2011, Australian Government., 2022, url: https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/latest-release.
Patel V, Chisholm D, Parikh R et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. The Lancet. 2016;387(10028):1672–1685.
Necho M, Tsehay M, Birkie M, et al. Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Int J Soc Psychiatry. 2021;67(7):892–906.
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33(2):e100213.
Chaix B, Delamon G, Guillemassé A, Brouard B, Bibault J-E. Psychological distress during the COVID-19 pandemic in France: a national assessment of at-risk populations. Gen psychiatry. 2020;33(6):e100349.
Marquez PV, Saxena S. Making Mental Health a Global Priority. Cerebrum 2016, 2016:cer-10-16.
Abdin S, Welch R, Byron-Daniel J, Meyrick J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: a systematic review. Public Health. 2018;160(1):70–6.
Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, Jansson-Fröjmark M, Palagini L, Rücker G, Riemann D. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019;43(1):96–105.
Rodriguez-Ayllon M, Cadenas-Sánchez C, Estévez-López F, Muñoz NE, Mora-Gonzalez J, Migueles JH, Molina-García P, Henriksson H, Mena-Molina A, Martínez-Vizcaíno V. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019;49(9):1383–410.
McHugh JE, Lawlor BA. Exercise and social support are associated with psychological distress outcomes in a population of community-dwelling older adults. J Health Psychol. 2012;17(6):833–44.
Thivel D, Tremblay A, Genin PM, Panahi S, Rivière D, Duclos M. Physical activity, inactivity, and sedentary behaviors: definitions and implications in occupational health. Front Public Health. 2018;6(2):288.
Whitehead BR, Blaxton JM. Daily well-being benefits of physical activity in older adults: does time or type matter? Gerontologist. 2017;57(6):1062–71.
Matricciani L, Bin YS, Lallukka T, Kronholm E, Wake M, Paquet C, Dumuid D, Olds T. Rethinking the sleep-health link. Sleep Health. 2018;4(4):339–48.
Swanson CM, Kohrt WM, Buxton OM, Everson CA, Wright KP Jr, Orwoll ES, Shea SA. The importance of the circadian system & sleep for bone health. Metabolism. 2018;84(1):28–43.
Worley SL. The extraordinary importance of sleep: the detrimental effects of inadequate sleep on health and public safety drive an explosion of sleep research. Pharm Ther. 2018;43(12):758–63.
Griffiths A, Kouvonen A, Pentti J, Oksanen T, Virtanen M, Salo P, Väänänen A, Kivimäki M, Vahtera J. Association of physical activity with future mental health in older, mid-life and younger women. Eur J Public Health. 2014;24(5):813–8.
Henson J, Yates T, Biddle SJ, Edwardson CL, Khunti K, Wilmot EG, Gray LJ, Gorely T, Nimmo MA, Davies MJ. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56(5):1012–20.
Mansoubi M, Pearson N, Biddle SJ, Clemes S. The relationship between sedentary behaviour and physical activity in adults: a systematic review. Prev Med. 2014;69(2):28–35.
Sullivan AN, Lachman ME. Behavior change with fitness technology in sedentary adults: a review of the evidence for increasing physical activity. Front Public Health. 2017;4(3):289.
Strasser B, Fuchs D. Role of physical activity and diet on mood, behavior, and cognition. Neurol Psychiatry Brain Res. 2015;21(3):118–26.
Australian Institute of Health and Welfare. Physical activity repot. Canberra., 2022, url: https://www.aihw.gov.au/reports-data/behaviours-risk-factors/physical-activity/overview.
The Department of Health and Aged Care. Physical activity and exercise guidelines for all Australians: For adults (18 to 64 years). Australian Government, Canberra 2022. url: https://www.health.gov.au/health-topics/physical-activity-and-exercise/physical-activity-and-exercise-guidelines-for-all-australians/for-adults-18-to-64-years.
Parliament of Australia. Inquiry into sleep health awareness in australia: Insufficient Sleep, Canberra, 2018 url: https://www.aph.gov.au/Parliamentary_Business/Committees/House/Health_Aged_Care_and_Sport/SleepHealthAwareness/Report/section?id=committees%2Freportrep%2F024220%2F26953.
South Australia Health. Getting Enough Sleep, Governemnt of South Australia., 2022, url: https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/healthy+living/healthy+sleep/getting+enough+sleep.
Australian Bureau of Statistics: 4324.0.55.001 - Microdata: National Health Survey, 2014–15. Canberra. ; 2016, url: https://www.abs.gov.au/Ausstats/abs@.nsf/c1061106e0c3442fca2568b5007b861d/afe17893065f4400ca2568a900143b61!OpenDocument.
Digital. 2021 Australia, url: https://wearesocial.com/au/digital-2021-australia.
Dumuid D, Pedišić Ž, Palarea-Albaladejo J, Martín-Fernández JA, Hron K, Olds T. Compositional data analysis in time-use epidemiology: what, why, how. Int J Environ Res Public Health. 2020;17(7):2220.
Dumuid D, Stanford TE, Martin-Fernández J-A, Pedišić Ž, Maher CA, Lewis LK, Hron K, Katzmarzyk PT, Chaput J-P, Fogelholm M. Compositional data analysis for physical activity, sedentary time and sleep research. Stat Methods Med Res. 2018;27(12):3726–38.
Olds T, Burton NW, Sprod J, Maher C, Ferrar K, Brown WJ, van Uffelen J, Dumuid D. One day you’ll wake up and won’t have to go to work: the impact of changes in time use on mental health following retirement. PLoS ONE. 2018;13(6):199605.
Lewthwaite H, Olds T, Williams MT, Effing TW, Dumuid D. Use of time in chronic obstructive pulmonary disease: longitudinal associations with symptoms and quality of life using a compositional analysis approach. PLoS ONE. 2019;14(3):e0214058.
Larisch L-M, Bojsen-Møller E, Nooijen CF, Blom V, Ekblom M, Ekblom Ö, Arvidsson D, Fridolfsson J, Hallman DM, Mathiassen SE. Effects of two randomized and controlled multi-component interventions focusing on 24-Hour Movement Behavior among Office Workers: a compositional data analysis. Int J Environ Res Public Health. 2021;18(8):4191.
Curtis RG, Dumuid D, Olds T, Plotnikoff R, Vandelanotte C, Ryan J, Edney S, Maher C. The association between time-use behaviors and physical and mental well-being in adults: a compositional isotemporal substitution analysis. J Phys Activity Health. 2020;17(2):197–203.
Curtis RG, Olds T, Fraysse F, Dumuid D, Hendrie GA, Esterman A, Brown WJ, Ferguson T, Lagiseti R, Maher CA. Annual rhythms in adults’ lifestyle and health (ARIA): protocol for a 12-month longitudinal study examining temporal patterns in weight, activity, diet, and wellbeing in australian adults. BMC Public Health. 2021;21(1):1–8.
Watson A, Maher C, Tomkinson GR, Golley R, Fraysse F, Dumuid D, Lewthwaite H, Olds T. Life on holidays: study protocol for a 3-year longitudinal study tracking changes in children’s fitness and fatness during the in-school versus summer holiday period. BMC Public Health. 2019;19(1):1–8.
Reid RER, Insogna JA, Carver TE, Comptour AM, Bewski NA, Sciortino C, Andersen RE. Validity and reliability of fitbit activity monitors compared to ActiGraph GT3X + with female adults in a free-living environment. J Sci Med Sport. 2017;20(6):578–82.
Shook RP, Yeh H-W, Welk GJ, Davis AM, Ries D. Commercial Devices provide estimates of Energy Balance with varying degrees of Validity in Free-Living adults. J Nutr. 2021;152(2):630–8.
de Zambotti M, Goldstone A, Claudatos S, Colrain IM, Baker FC. A validation study of Fitbit Charge 2™ compared with polysomnography in adults. Chronobiol Int. 2018;35(4):465–76.
Mantua J, Gravel N, Spencer R. Reliability of sleep measures from four personal health monitoring devices compared to research-based actigraphy and polysomnography. Sensors. 2016;16(5):646.
Reid RE, Insogna JA, Carver TE, Comptour AM, Bewski NA, Sciortino C, Andersen RE. Validity and reliability of fitbit activity monitors compared to ActiGraph GT3X + with female adults in a free-living environment. J Sci Med Sport. 2017;20(6):578–82.
Carpenter C, Yang CH, West D. A comparison of sedentary behavior as measured by the Fitbit and ActivPAL in College Students. Int J Environ Res Public Health. 2021;18(8):3914.
Murakami H, Kawakami R, Nakae S, Yamada Y, Nakata Y, Ohkawara K, Sasai H, Ishikawa-Takata K, Tanaka S, Miyachi M. Accuracy of 12 wearable devices for estimating physical activity energy expenditure using a metabolic chamber and the doubly labeled water method: validation study. JMIR mHealth and uHealth. 2019;7(8):13938.
Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11):531–S543.
Ronk FR, Korman JR, Hooke GR, Page AC. Assessing clinical significance of treatment outcomes using the DASS-21. Psychol Assess. 2013;25(4):1103–10.
Oei TP, Sawang S, Goh YW, Mukhtar F. Using the depression anxiety stress scale 21 (DASS-21) across cultures. Int J Psychol. 2013;48(6):1018–29.
Henry JD, Crawford JR. The short-form version of the Depression anxiety stress scales (DASS‐21): construct validity and normative data in a large non‐clinical sample. Br J Clin Psychol. 2005;44(2):227–39.
Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression anxiety stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176.
Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Prev Med. 2008;46(5):397–411.
Buman MP, Hekler EB, Haskell WL, Pruitt L, Conway TL, Cain KL, Sallis JF, Saelens BE, Frank LD, King AC. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–65.
Chu I-H, Buckworth J, Kirby TE, Emery CF. Effect of exercise intensity on depressive symptoms in women. Ment Health Phys Act. 2009;2(1):37–43.
Nakagawa T, Koan I, Chen C, Matsubara T, Hagiwara K, Lei H, Hirotsu M, Yamagata H, Nakagawa S. Regular moderate-to vigorous-intensity physical activity rather than walking is associated with enhanced cognitive functions and mental health in young adults. Int J Environ Res Public Health. 2020;17(2):614.
Perales F, Pozo-Cruz Jd P-C, Bd. Impact of physical activity on psychological distress: a prospective analysis of an australian national sample. Am J Public Health. 2014;104(12):91–7.
Feehan LM, Geldman J, Sayre EC, Park C, Ezzat AM, Yoo JY, Hamilton CB, Li LC. Accuracy of Fitbit devices: systematic review and narrative syntheses of quantitative data. JMIR mHealth and uHealth. 2018;6(8):10527.
Kodsi A, Bullock B, Kennedy GA, Tirlea L. Psychological interventions to improve sleep in young adults: a systematic review and Meta-analysis of Randomized controlled trials. Behav sleep Med. 2021;1(2):1–18.
Magee CA, Caputi P, Iverson DC. Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Med. 2011;12(4):346–50.
van Mill JG, Hoogendijk WJ, Vogelzangs N, van Dyck R, Penninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry. 2010;71(3):239–46.
Acknowledgements
None.
Funding
This project is funded by the Australian National Health and Medical Research Council (APP1163338). The funding body was not involved in the study design, data collection, interpretation of data, data analysis, or in the preparation of the manuscript. CM receives an Investigator Grant from the Medical Research Future Fund (1193862). DD receives an Early Career Research Fellowship from the National Health and Medical Research Council (1162166).
Author information
Authors and Affiliations
Contributions
HM, RC, TF, DD, and CM designed the study. HM, RC, and TF contributed to data collection. DD led the statistical analysis. All authors interpreted the results. HM and BS wrote the original manuscript. RC, TF, DD, BS and CM reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have declared that they have no competing interests.
Ethics approval and consent to participate
Ethics approval was received before recruitment of participants by the University of South Australia Human Research Ethics Committee (Protocol number: 201901). Participants provided informed and written consent prior to commencing the study. This prospective study was registered on the Australian New Zealand Clinical Trial Registry (Trial ID: ACTRN12619001430123).
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Curtis, R.G., Dumuid, D., McCabe, H. et al. The association between 24-hour activity, sedentary and sleep compositions and mental health in Australian adults: a cross-sectional study. JASSB 2, 15 (2023). https://doi.org/10.1186/s44167-023-00024-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44167-023-00024-6