Abstract
Background
Noninvasive ventilation (NIV) is widely employed as the initial treatment for patients with chronic acute exacerbation of obstructive pulmonary disease (AECOPD). Nevertheless, high-flow nasal cannula (HFNC) has been increasingly utilized and investigated to mitigate the issues associated with NIV. Flow rate may play a significant role in diaphragmatic function among subjects recovering from AECOPD. Based on these observations, we conducted a physiological study to assess the impact of HFNC therapy on diaphragmatic function, as measured by US, respiratory rate (RR), gas exchange, and patient comfort at various flow rates.
Methods
A prospective physiological pilot study enrolled subjects with a diagnosis of AECOPD who required NIV for more than 24 h. After stabilization, these subjects underwent a 30-min trial using NIV and HFNC at different sequential flow rates (30–60 L/min). At the end of each trial, diaphragmatic displacement (DD, cm) and diaphragmatic thickness fraction (DTF, %) were measured using ultrasound. Additionally, other physiological variables, such as RR, gas exchange, and patient comfort, were recorded.
Results
A total of 20 patients were included in the study. DD was no different among trials (p = 0.753). DTF (%) was significantly lower with HFNC-30 L/min compared to HFNC-50 and 60 L/min (p < 0.001 for all comparisons). No significant differences were found in arterial pH and PaCO2 at discontinuation of NIV and at the end of HFNC trials (p > 0.050). During HFNC trials, RR remained unchanged without statistically significant differences (p = 0.611). However, we observed that HFNC improved comfort compared to NIV (p < 0.001 for all comparisons). Interestingly, HFNC at 30 and 40 L/min showed greater comfort during trials.
Conclusions
In subjects recovering from AECOPD and receiving HFNC, flows above 40 L/min may not offer additional benefits in terms of comfort and decreased respiratory effort. HFNC could be a suitable alternative to COT during breaks off NIV.
Similar content being viewed by others
Introduction
Noninvasive ventilation (NIV) is widely employed as the initial treatment for patients with chronic acute exacerbation of obstructive pulmonary disease (AECOPD) who experience acute hypercapnic respiratory failure caused by different triggers [1]. In these subjects, the application of NIV has demonstrated efficacy in improving respiratory gas exchange, reducing the need for endotracheal intubation (ETI), and enhancing overall survival [2, 3]. Nevertheless, high-flow nasal cannula (HFNC) has been increasingly utilized and investigated to mitigate the issues associated with NIV, including interface discomfort, pressure injury, sleep disturbances, and patient-ventilator asynchrony [4, 5]. HFNC facilitates secretion clearance, prevents epithelial injury, and mitigates airway inflammation [6]. HFNC delivers positive airway pressure, countering intrinsic positive end-expiratory pressure (PEEPi) and thereby reducing the isometric workload linked with dynamic hyperinflation. However, some patients may experience heightened inspiratory effort as flow rates escalate, potentially stemming from discomfort, increased dynamic hyperinflation, or elevated expiratory resistance [7].
Recent meta-analyses in COPD found that HFNC significantly reduces PaCO2 compared to conventional oxygen therapy (COT) [8,9,10]. On the other hand, conflicting results are observed in patients with AECOPD, one meta-analysis concluded no significant benefit in reducing ETI compared with NIV [11], while another indicated that HFNC is non-inferior to NIV in decreasing the risk of ETI during AECOPD [12]. HFNC has some physiological advantages for AECOPD patients: heated and humidified gas delivery, anatomical dead space washout, “PEEP” (positive end-expiratory pressure) effect, provision of stable inspired oxygen fraction (FiO2), and treatment comfort [13]. In addition, HFNC allows us to combine with vibrating mesh nebulizers to deliver aerosol therapy without impairing the performance of respiratory support [14].
Although the physiological effects of HFNC are well known, few studies have assessed the diaphragmatic function in subjects recovering from an AECOPD treated with HFNC to individualize this treatment [15, 16]. Ultrasonography (US) is a simple tool available at the bedside that allows the evaluation of diaphragm function, present or abolished, through M-mode, with the measurement of diaphragmatic displacement (DD, cm) and its force through the measurement of diaphragm thickening fraction (DTF, %) [17,18,19]. Both measures are affected in various ways by subjects admitted to the emergency department with AECOPD [20, 21]. Flow rate may play a significant role in diaphragmatic function among subjects recovering from an AECOPD. Based on these observations, we conducted a physiological study to assess the impact of HFNC therapy on diaphragmatic function, as measured by US, respiratory rate (RR), gas exchange, and patient comfort at various flow rates.
Methods
Study design
This prospective physiological pilot study was carried out at the respiratory intermediate care unit (RICU) of the Hospital General de Agudos Juan A. Fernández, Buenos Aires, Argentina, from March 2022 to March 2023. The institutional review boards reviewed the protocol and authorized prospective data collection (identified code no. 2663). Written informed consent to participate was obtained from each subject or their relatives.
Subjects
Patients with a previous diagnosis of COPD who were admitted to the RICU with AECOPD and required NIV for acute hypercapnic respiratory failure (pH ≤ 7.35 with a PaCO2 ≥ 45 mmHg) [22]. Underlying COPD could be documented by spirometry and defined by an FEV1/FVC < 0.70 or, alternatively, highly suspected underlying COPD. Subjects with suspected underlying COPD without previous spirometry should have a history of smoking and emphysema on chest radiograph or computed tomography scan without other reasons for respiratory acidosis [23].
After initial management and stabilization with NIV, patients were eligible for inclusion in the study. Inclusion criteria were as follows: (1) NIV duration exceeding 24 h, (2) full patient cooperation, (3) arterial pH ≥ 7.35 during NIV, (4) RR ≤ 30 breaths per minute, and (5) clinical stability, indicated by the absence of dyspnea measured on a visual analog scale (VAS), the absence of pain, agitation, and fever.
Exclusion criteria were as follows: (1) Diaphragm paralysis, (2) clinical signs of distress or respiratory muscle fatigue, (3) hemodynamic instability (systolic arterial pressure < 90 mmHg or mean arterial pressure < 60 mmHg or requirement of vasoactive agents), (4) cardiac arrhythmia, (5) impaired renal function, and (6) NIV intolerance.
Study protocol
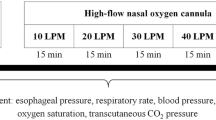
After enrollment, all patients underwent five 30-min trials sequentially, as outlined in the study protocol illustrated in Fig. 1. The first trial utilized NIV delivered by a dedicated ventilator (Astral 150, ResMed, San Diego, CA, USA) equipped with a low-pressure oxygen source via a non-vented face mask with a blue elbow and double-limb circuit (FreeMotion RT041, Fisher and Paykel, Auckland, New Zealand). Subsequently, patients were transitioned to HFNC using standard devices (Airvo 2, Fisher and Paykel, Auckland, New Zealand) with a medium-sized cannula. Flow rates of 30, 40, 50, and 60 L/min were sequentially administered, with a temperature set to 34 °C. FiO2 was adjusted to maintain oxygen saturation measured by pulse oximetry (SpO2) 88–92% and kept constant throughout the protocol. We also encouraged patients to breathe with their mouths closed as often as possible to enhance the maximum effect of HFNC.
Patients remained on HFNC following completion of the study. However, if agitation or alterations in mental status, use of respiratory accessory muscles, paradoxical motion of the abdomen, dyspnea, pH < 7.30, or hemodynamic instability (systolic blood pressure < 90 mmHg or > 180 mmHg) occurred, the protocol was discontinued.
Data collection
Upon admission, we documented demographic data including age, gender, body mass index (BMI), long-term oxygen therapy, Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification, comorbidities, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, Glasgow Coma Scale, vital signs, and arterial blood gases (ABG) at admission. We also recorded NIV settings and the number of days until clinical stability.
Diaphragmatic ultrasonography
At the end of each trial, after excluding the presence of a hemidiaphragm chronic elevation or paralysis with ultrasound, two investigators (I. C. and V. C.), unaware of the study aims, independently performed bedside sonographic evaluation of the right hemidiaphragm. The following ultrasound device was used: a Philips Lumify® ultrasound machine (Philips Medical Systems, Bothell, WA, USA) with a convex transducer, a Sonoscape S6® ultrasound machine (Yizhe Building, Yuquan Road, Shenzhen, 518,051, China).
Diaphragm displacement (DD [cm]) was assessed on the right side by using the subcostal view in B-mode and transverse scanning. We use right-side approach as the restricted acoustic window presented by the spleen and gastric bubble on the left side. This limitation is attributed to the swift inspiratory lung movement observed in dyspneic subjects and the acoustic impediment posed by air within the bowel and stomach [19, 24]. The US measurements were always performed during spontaneous breathing. DTF was assessed at both end-expiration (DTF-exp [mm]) and end-inspiration (DTF-insp [mm]) phases. The DTF, serving as an indirect measure of diaphragmatic effort [24,25,26], was computed using the following formula: DTF (%) = ([DTF-insp — DTF-exp]/DTF-exp) × 100. Compared with DD, DTF (%) is a more sensitive and qualitatively accurate parameter and provides a more comprehensive measure of diaphragm contraction. For each patient, three evaluations of DD were conducted on the right side, and three measurements of expiratory and inspiratory DTF were taken on the right side. The average values for DD, as well as expiratory and inspiratory thickness, were calculated. Two operators performed all measurements for each participant.
Other physiological variables
We evaluated gas exchange by ABG at NIV discontinuation and at the end of HFNC trials. RR was measured during the trials, and patient comfort was assessed using the visual analog scale (VAS) (0 = representing the worst possible comfort and 10 = representing no discomfort).
Simple sizes calculation
Given the physiological design of the study, we did not conduct a formal sample size calculation. Consistent with previous investigations employing similar designs on the topic [7, 27], we aimed to enroll 20 subjects. This sample size was deemed adequate for drawing meaningful conclusions on these endpoints.
Statical analysis
The normality of data distribution was assessed by the Shapiro–Wilk test. Normally distributed variables are expressed as mean ± standard deviation and were analyzed by repeated measures analysis of variance (ANOVA) followed by a post hoc pairwise comparison with Bonferroni adjustment. Non-normally distributed variables are expressed as median and interquartile range (IQR) and were compared by Friedman’s two-way ANOVA by ranks with a Dunn’s test post hoc pairwise comparison with Bonferroni correction. Categorical variables are expressed as frequency and percentage. The reproducibility of US measurements was expressed as the intra-class correlation coefficient (ICC). The coefficient of repeatability was calculated as the British Standards Institution repeatability coefficient (twice the standard deviation of the differences in repeated measurements). A p-value of less than 0.05 was considered statistically significant. The statistical analysis was performed using R Studio (Version 1.3.1093, R Foundation for Statistical Computing, Vienna, Austria).
Results
Patients’ characteristics
A total of 20 patients were included in the study, with a median age of 65 (interquartile range [IQR], 62–71) years. Fifteen (75%) of these were men. Regarding clinical characteristics, the subjects had a median body mass index (BMI) of 27.6 (19.4–31.9 kg/m2) and a median APACHE II score of 15 (9–17) points. Fifteen subjects (60%) were classified as GOLD IV. The patients’ characteristics are listed in Table 1.
Ultrasonography measurements
At the time of NIV discontinuation, the median applied PEEP was 7 (6–8) cmH2O, while the PSV was 10 (8–12) cmH2O, and FiO2 was 35 (30–42) %. DD was no different among trials (p = 0.753). Diaphragm TF (%) was significantly lower with HFNC-30 L/min compared to HFNC-50 and 60 L/min (p < 0.001 for all comparisons). Diaphragm TF (%) was not different between HFNC-30 and 40 L/min. All data are displayed in Table 2.
Other physiological variables
No significant differences were found in arterial pH and PaCO2 at discontinuation of NIV and at the end of HFNC trials (p > 0.050). During HFNC trials, RR remained unchanged without statistically significant differences (p = 0.611). The values of the changes in ABG during the interruption of NIV and at the end of the trial with HFNC, along with the trend of RR during the study, are presented in Fig. 2. Interestingly, HFNC at 30 and 40 L/min showed greater comfort during trials.
Reproducibility of US
ICC were all above 0.96. Coefficients of repeatability ranged around 5–7% for intra-or inter-analyzer repeatability and around 10–13% for intra or inter-observer repeatability.
Adverse events
The protocol was safely concluded in all 20 patients without any adverse effects. NIV reinstitution within the following 48 h occurred in seven patients (35%).
Discussion
In this preliminary, physiological prospective pilot study, we evaluated the effects of HFNC at different flow rates on diaphragmatic function in subjects recovering from an AECOPD who had initially been managed and stabilized with NIV. We found that (1) DD and RR were similar across different flow rates during HFNC therapy; (2) diaphragm TF (%) was higher during HFNC-50 and 60 L/min; (3) HFNC improved patient comfort compared to NIV, with the greatest improvement observed at HFNC-30 and 40 L/min; and (4) HFNC flow rate did not provide significant change in arterial pH and PaCO2.
DD has been extensively studied as an index of diaphragmatic contractile activity [17]. Recent studies indicate that this index does not correlate with other indices of inspiratory effort [28]. In subjects under invasive mechanical ventilation (IMV), DD during an assisted breath represents the combined effect of two forces acting in the same direction: the force generated by the diaphragm’s own contraction and the passive displacement caused by the pressure provided by the ventilator. Although the subjects in our study were not on IMV, they were receiving respiratory support (NIV and HFNC). Longhini et al., in a physiological crossover study involving subjects with acute hypercapnic respiratory failure requiring NIV for 24 h, investigated the impact of transitioning to COT and HFNC-50 L/min. They evaluated diaphragmatic function and other variables [16]. Similar to our findings, they observed no significant difference in DD and RR between the different trials. In contrast to subjects with stable COPD, diaphragm US proved to be a feasible and reliable clinical approach for assessing diaphragm dysfunction in dyspneic hypercapnic acute respiratory failure patients undergoing NIV. Evaluating DD 2 h after NIV initiation was a better predictor of NIV failure compared to pH, PaCO2, and left expiratory diaphragmatic thickness [20]. In critically ill patients, the most commonly used criterion to indicate diaphragmatic dysfunction is a DD < 1–1.1 cm [18, 21]. Recent investigations have reported the presence of diaphragmatic dysfunction in 25–30% of subjects with AECOPD admitted with acute hypercapnic respiratory failure [26, 29]. However, in our study, we did not observe diaphragmatic dysfunction.
Ultrasonography can be used to directly image the diaphragm. Its identification relies on the bright echoes reflected from the attached parietal pleura and peritoneal membranes. Additionally, ultrasonography has been employed to assess the length and thickness of the zone of apposition against the rib cage at different lung volumes. Vivier et al. showed that diaphragm thickening accurately predicts changes in inspiratory muscle effort in response to changes in PSV levels during NIV in subjects after extubation [25]. The DTF (%) could serve as a valuable tool for evaluating diaphragmatic function and its impact on respiratory workload across various scenarios, including during noninvasive respiratory support (NRS) [30]. Additionally, DTF (%) correlates with muscle strength and shortening. In the absence of diaphragm dysfunction, DTF (%) can estimate changes in WOB during NRS, similar findings demonstrated by Umbrello et al. in patients under IMV [28, 30].
The directional changes in DTF (%) following flow increases during HFNC treatment can be explained by findings reported in non-intubated subjects with acute hypoxemic respiratory failure. Higher flow rates linearly improve respiratory drive, end-expiratory lung volume (EELV), lung mechanics, and oxygenation. Meanwhile, effort and minute ventilation decrease exponentially, with most of the beneficial effects achieved at a flow rate of 30 L/min [31]. However, in subjects with COPD, these results may be opposite. Rittayamai et al. investigated the impact of HFNC at flow rates of 10–50 L/ min in COPD subjects who had been previously stabilized with NIV. They encouraged the subjects to keep their mouths closed during HFNC therapy and observed an increase in work of breathing (WOB) at flow rates above 40 L/ min [7]. Similar to our results, with flow rates greater than 50 and 60 L/min, the DTF (%) increased. We hypothesize that patient discomfort, worsening dynamic hyperinflation, or increased resistance to breathing could explain the observed increase in WOB with HFNC at a flow rate of 50 L/min. A study comparing HFNC at 30 L/min vs COT in patients with stable COPD found significant increases in EELV with HFNC. The increase in EELV with HFNC may have aggravated dynamic hyperinflation and effort to breathe in some COPD patients [32]. While comfort during HFNC was higher than NIV, during HFNC-50 and 60 L/min, subjects reported slightly more discomfort in our study. One explanation for this may be due to turbulent airflow, which can increase inspiratory resistance during HFNC therapy with the mouth closed. This turbulent airflow could be generated during the inspiratory phase under HFNC with the mouth closed, particularly when the HFNC flow rate exceeds the inspiratory flow, reverting its direction. This phenomenon could be explained by the findings of Vieira et al. which showed during HFNC at 40 L/min, and inspiratory and expiratory airway resistance was higher with the mouth closed than with the mouth open [33]. The positive airway pressure generated by HFNC with mouth closed can play an important role in terms of clinical effects, and the increased expiratory resistance during HFNC may also contribute to physiological benefits. The increased expiratory resistance during HFNC, especially with the mouth closed, is a mechanism that induces a longer expiratory phase, thereby lowering the RR and minute ventilation [34, 35]. COPD subjects often adopt pursed-lip breathing which helps alleviate expiratory flow limitation and dynamic hyperinflation [36]. In fact, the effect of HFNC on expiratory resistance mimic the pursed-lip breathing effect. In obstructive patients, by contrast, high-flow rates should be used with caution to avoid an excessive increase in airway resistances [7].
Regarding gas exchange, we did not find a significant reduction in arterial pH and PaCO2 with HFNC. The reduction of anatomical dead space and the consequent elimination of CO2 are the mechanism that has been proposed to explain the decrease in PaCO2 [37]. Indeed, PaCO2 directly controls the activity of inspiratory muscles alone, and therefore, its reduction may lead to a decrease in diaphragmatic effort. A study by Bräunlich et al. [38] compared HFNC, nasal CPAP, and nasal NIV in 67 hospitalized COPD patients. They found that increasing the flow rate from 20 to 30 L/min improved CO2 elimination and reduced PaCO2. However, considering the significant reduction in RR with similar PaCO2 levels during NIV and HFNC, it is reasonable to assume that tidal volume is higher under these conditions, unlike COT, as already demonstrated by other authors [16].
In COPD subjects with hypercapnic acute respiratory failure, the rate of NIV discontinuation failure may be relatively high [39]. This inability to maintain unassisted spontaneous breathing depends on an excessive load, which increases diaphragm contraction to an extent that cannot be sustained over time. Longhini et al. reported that although COT caused a marked increase in DTF (%) and HFNC allowed it to remain unchanged. Therefore, according to these results and ours, in subjects recovering from an AECOPD, HFNC could be used during NIV breaks [16, 40].
This study presents limitations:
-
(1)
Since it is a sequential study and not a randomized crossover design, the effect of treatment duration on many physiological variables cannot be ruled out.
-
(2)
Operator influence on diaphragm ultrasonography was considered. To mitigate this, ultrasound assessments were independently performed by two operators. Consistent with prior research, a high ICC was observed, minimizing the risk of bias.
-
(3)
Limitations related to the device prevented the measurement of tidal volume during HFNC and PEEPi levels.
-
(4)
The level of PSV and PEEP during NIV in our study was lower compared to levels reported in previous studies, and most patients were stabilized before study inclusion. This factor may introduce a bias favoring HFNC in terms of decreased WOB.
Conclusion
In subjects recovering from an AECOPD and receiving HFNC, flows above 40 L/min may not offer additional benefits in terms of comfort and decreased respiratory effort. HFNC could be a suitable alternative to COT during breaks off NIV.
Availability of data and materials
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Abbreviations
- NIV:
-
Noninvasive ventilation
- AECOPD:
-
Acute exacerbation of obstructive pulmonary disease
- ETI:
-
Endotracheal intubation
- HFNC:
-
High-flow nasal cannula
- WOB:
-
Work of breathing
- PEEPi:
-
Intrinsic positive end-expiratory pressure
- PaCO2 :
-
Arterial carbon dioxide tension
- FiO2 :
-
Inspired oxygen fraction
- COT:
-
Conventional oxygen therapy
- PEEP:
-
Positive end-expiratory pressure
- PSV:
-
Pressure support ventilation
- DD:
-
Diaphragmatic displacement
- DTF:
-
Diaphragm thickening fraction
- US:
-
Ultrasonography
- RICU:
-
Respiratory intermediate care unit
- GOLD:
-
Global initiative for chronic obstructive lung diseases
- RR:
-
Respiratory rate
- VAS:
-
Visual analog scale
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- ICC:
-
Intra-class correlation coefficient
- IMV:
-
Invasive mechanical ventilation
- EELV:
-
End-expiratory lung volume
References
Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S et al (2017) Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J 50:1602426. https://doi.org/10.1183/13993003.02426-2016
Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A et al (1995) Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 333:817–822. https://doi.org/10.1056/NEJM199509283331301
Squadrone E, Frigerio P, Fogliati C, Gregoretti C, Conti G, Antonelli M et al (2004) Noninvasive vs invasive ventilation in COPD patients with severe acute respiratory failure deemed to require ventilatory assistance. Intensive Care Med 30:1303–1310. https://doi.org/10.1007/S00134-004-2320-7
Carron M, Freo U, Bahammam AS, Dellweg D, Guarracino F, Cosentini R et al (2013) Complications of non-invasive ventilation techniques: a comprehensive qualitative review of randomized trials. Br J Anaesth 110:896–914. https://doi.org/10.1093/BJA/AET070
Cammarota G, Simonte R, De Robertis E (2022) Comfort during non-invasive ventilation Front Med (Lausanne) 9:874250. https://doi.org/10.3389/FMED.2022.874250
Veenstra P, Veeger NJGM, Koppers RJH, Duiverman ML, van Geffen WH (2022) High-flow nasal cannula oxygen therapy for admitted COPD-patients. A retrospective cohort study PLoS One 17:e0272372. https://doi.org/10.1371/JOURNAL.PONE.0272372
Rittayamai N, Phuangchoei P, Tscheikuna J, Praphruetkit N, Brochard L (2019) Effects of high-flow nasal cannula and non-invasive ventilation on inspiratory effort in hypercapnic patients with chronic obstructive pulmonary disease: a preliminary study. Ann Intensive Care 9:1–8. https://doi.org/10.1186/S13613-019-0597-5/FIGURES/3
Zhang L, Wang Y, Ye Y, Gao J, Zhu F, Min L (2023) Comparison of high-flow nasal cannula with conventional oxygen therapy in patients with hypercapnic chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 18:895. https://doi.org/10.2147/COPD.S402506
Yang H, Huang D, Luo J, Liang Z, Li J (2023) The use of high-flow nasal cannula in patients with chronic obstructive pulmonary disease under exacerbation and stable phases: a systematic review and meta-analysis. Heart Lung 60:116–126. https://doi.org/10.1016/J.HRTLNG.2023.02.016
Duan L, Xie C, Zhao N (2022) Effect of high-flow nasal cannula oxygen therapy in patients with chronic obstructive pulmonary disease: a meta-analysis. J Clin Nurs 31:87–98. https://doi.org/10.1111/JOCN.15957
Bonnevie T, Elkins M, Paumier C, Medrinal C, Combret Y, Patout M et al (2019) Nasal high flow for stable patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. COPD 16:368–377. https://doi.org/10.1080/15412555.2019.1672637
Du Y, Zhang H, Ma Z, Liu J, Wang Z, Lin M et al (2023) High-flow nasal oxygen versus noninvasive ventilation in acute exacerbation of chronic obstructive pulmonary disease patients: a meta-analysis of randomized controlled trials. Can Respir J 2023:12. https://doi.org/10.1155/2023/7707010
Bruni A, Garofalo E, Procopio D, Corrado S, Caroleo A, Biamonte E et al (2022) Current practice of high flow through nasal cannula in exacerbated COPD patients. Healthcare. 10:536. https://doi.org/10.3390/HEALTHCARE10030536
Colaianni-Alfonso N, Macloughlin R, Espada A, Saa Y, Techera M, Toledo A et al (2023) Delivery of aerosolized bronchodilators by high-flow nasal cannula during COPD exacerbation. Respir Care 68:721–726. https://doi.org/10.4187/RESPCARE.10614
Di mussi R, Spadaro S, Stripoli T, Volta CA, Trerotoli P, Pierucci P, et al. High-flow nasal cannula oxygen therapy decreases postextubation neuroventilatory drive and work of breathing in patients with chronic obstructive pulmonary disease. Crit Care 2018;22. https://doi.org/10.1186/S13054-018-2107-9.
Longhini F, Pisani L, Lungu R, Comellini V, Bruni A, Garofalo E et al (2019) High-flow oxygen therapy after noninvasive ventilation interruption in patients recovering from hypercapnic acute respiratory failure: a physiological crossover trial. Crit Care Med 47:E506–E511. https://doi.org/10.1097/CCM.0000000000003740
Matamis D, Soilemezi E, Tsagourias M, Akoumianaki E, Dimassi S, Boroli F et al (2013) Sonographic evaluation of the diaphragm in critically ill patients Technique and clinical applications. Intensive Care Med 39:801–10. https://doi.org/10.1007/S00134-013-2823-1
Vetrugno L, Guadagnin GM, Barbariol F, Langiano N, Zangrillo A, Bove T (2019) Ultrasound imaging for diaphragm dysfunction: a narrative literature review. J Cardiothorac Vasc Anesth 33:2525–2536. https://doi.org/10.1053/J.JVCA.2019.01.003
Boussuges A, Gole Y, Blanc P (2009) Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values. Chest 135:391–400. https://doi.org/10.1378/CHEST.08-1541
Cammarota G, Sguazzotti I, Zanoni M, Messina A, Colombo D, Vignazia GL et al (2019) Diaphragmatic ultrasound assessment in subjects with acute hypercapnic respiratory failure admitted to the emergency department. Respir Care 64:1469–1477. https://doi.org/10.4187/RESPCARE.06803
Barbariol F, Deana C, Guadagnin GM, Cammarota G, Vetrugno L, Bassi F. Ultrasound diaphragmatic excursion during non-invasive ventilation in ICU: a prospective observational study. Acta Bio Medica : Atenei Parmensis 2021;92. https://doi.org/10.23750/ABM.V92I3.11609.
Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J 2017;50. https://doi.org/10.1183/13993003.02426-2016.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A et al (2005) Standardisation of spirometry. Eur Respir J 26:319–338. https://doi.org/10.1183/09031936.05.00034805
Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D et al (2015) Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med 41:642–649. https://doi.org/10.1007/S00134-015-3687-3
Vivier E, Dessap AM, Dimassi S, Vargas F, Lyazidi A, Thille AW et al (2012) Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation. Intensive Care Med 38:796–803. https://doi.org/10.1007/S00134-012-2547-7
Marchioni A, Castaniere I, Tonelli R, Fantini R, Fontana M, Tabbì L, et al. Ultrasound-assessed diaphragmatic impairment is a predictor of outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease undergoing noninvasive ventilation. Crit Care 2018;22. https://doi.org/10.1186/S13054-018-2033-X.
Mauri T, Turrini C, Eronia N, Grasselli G, Volta CA, Bellani G et al (2017) Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med 195:1207–1215. https://doi.org/10.1164/RCCM.201605-0916OC
Umbrello M, Formenti P, Longhi D, Galimberti A, Piva I, Pezzi A, et al. Diaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: a pilot clinical study. Crit Care 2015;19. https://doi.org/10.1186/S13054-015-0894-9.
Antenora F, Fantini R, Iattoni A, Castaniere I, Sdanganelli A, Livrieri F et al (2017) Prevalence and outcomes of diaphragmatic dysfunction assessed by ultrasound technology during acute exacerbation of COPD: a pilot study. Respirology 22:338–344. https://doi.org/10.1111/RESP.12916
Vega ML, Schifino G, Pisani L, Catalanotti V, Prediletto I, Nava S (2023) Diaphragm thickening fraction and inspiratory effort in patients with SARS-COV II pneumonia receiving different non-invasive respiratory supports. Pulmonology 29:424–427. https://doi.org/10.1016/J.PULMOE.2023.02.001
Mauri T, Alban L, Turrini C, Cambiaghi B, Carlesso E, Taccone P et al (2017) Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med 43:1453–1463. https://doi.org/10.1007/S00134-017-4890-1/METRICS
Fraser JF, Spooner AJ, Dunster KR, Anstey CM, Corley A (2016) Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomised crossover trial. Thorax 71:759–761. https://doi.org/10.1136/THORAXJNL-2015-207962
Vieira F, Bezerra FS, Coudroy R, Schreiber A, Telias I, Dubo S et al (1985) High flow nasal cannula compared to continuous positive airway pressure: a bench and physiological study. J Appl Physiol 2022(132):1580–1590. https://doi.org/10.1152/JAPPLPHYSIOL.00416.2021
Pinkham MI, Domanski U, Franke KJ, Hartmann J, Schroeder M, Williams T et al (1985) Effect of respiratory rate and size of cannula on pressure and dead-space clearance during nasal high flow in patients with COPD and acute respiratory failure. J Appl Physiol 2022(132):553–563. https://doi.org/10.1152/JAPPLPHYSIOL.00769.2021
Mündel T, Feng S, Tatkov S, Schneider H (1985) Mechanisms of nasal high flow on ventilation during wakefulness and sleep. J Appl Physiol 2013(114):1058–1065. https://doi.org/10.1152/JAPPLPHYSIOL.01308.2012
Visser FJ, Ramlal S, Dekhuijzen PNR, Heijdra YF (2011) Pursed-lips breathing improves inspiratory capacity in chronic obstructive pulmonary disease. Respiration 81:372–378. https://doi.org/10.1159/000319036
Möller W, Celik G, Feng S, Bartenstein P, Meyer G, Eickelberg O et al (2015) Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol 118:1525. https://doi.org/10.1152/JAPPLPHYSIOL.00934.2014
Bräunlich J, Köhler M, Wirtz H (2016) Nasal highflow improves ventilation in patients with COPD. Int J Chron Obstruct Pulmon Dis 11:1077–1085. https://doi.org/10.2147/COPD.S104616
Lun CT, Chan VL, Leung WS, Cheung APS, Cheng SL, Tsui MSN et al (2013) A pilot randomized study comparing two methods of non-invasive ventilation withdrawal after acute respiratory failure in chronic obstructive pulmonary disease. Respirology 18:814–819. https://doi.org/10.1111/RESP.12080
Spoletini G, Mega C, Pisani L, Alotaibi M, Khoja A, Price LL et al (2018) High-flow nasal therapy vs standard oxygen during breaks off noninvasive ventilation for acute respiratory failure: a pilot randomized controlled trial. J Crit Care 48:418–425. https://doi.org/10.1016/J.JCRC.2018.10.004
Funding
None.
Author information
Authors and Affiliations
Contributions
NCA, GM, and LV are the guarantors of the content of the manuscript and contributed to all aspects of the study. NCA, IV, VC, SMG, and LV contributed substantially to study design, data collection, and data analysis. NCA, IV, VC, and LV contributed with project design and implementation. All authors reviewed the final manuscript. NCA and LV should be considered as authors equally.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethical committee (code register 2663), and informed consent was obtained from participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Colaianni-Alfonso, N., Castro, I., Cáceres, V. et al. Effect of high-flow nasal cannula at different flow rates on diaphragmatic function in subjects recovering from an acute exacerbation of COPD: a physiological prospective pilot study. J Anesth Analg Crit Care 4, 37 (2024). https://doi.org/10.1186/s44158-024-00173-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44158-024-00173-3