Abstract
Background
The use of extracorporeal carbon dioxide removal (ECCO2R) is less invasive than extracorporeal membrane oxygenation (ECMO), and intraoperative control of gas exchange could be feasible. The aim of this study in intermediate intraoperative severity patients undergoing LT was to assess the role of intraoperative ECCO2R on emergency ECMO requirement in patients.
Methods
Thirty-eight consecutive patients undergoing lung transplantation (LT) with “intermediate” intraoperative severity in the intervals 2007 to 2010 or 2011 to 2014 were analyzed as historical comparison of case-matched cohort retrospective study. The “intermediate” intraoperative severity was defined as the development of intraoperative severe respiratory acidosis with maintained oxygenation function (i.e., pH <7.25, PaCO2 >60 mmHg, and PaO2/FiO2 >150), not associated with hemodynamic instability. Of these 38 patients, twenty-three patients were treated in the 2007–2010 interval by receiving “standard intraoperative treatment,” while 15 patients were treated in the 2011–2014 interval by receiving “standard intraoperative treatment + ECCO2R.”
Results
ECMO requirement was more frequent among patients that received “standard intraoperative treatment” alone than in those treated with “standard intraoperative treatment + ECCO2R” (17/23 vs. 3/15; p = 0.004). The use of ECCO2R improved pH and PaCO2 while mean pulmonary artery pressure (mPAP) decreased.
Conclusion
In intermediate intraoperative severity patients, the use of ECCO2R reduces the ECMO requirement.
Similar content being viewed by others
Background
Perioperative management of patients undergoing lung transplant (LT) encompass to address serious respiratory and cardiac complications including systemic hypotension, pulmonary hypertension, right ventricular dysfunction, hypercapnia, and hypoxemia [1, 2]. Although LT is generally performed off-pump, extracorporeal support is necessary for up to 30 to 40% of the patients in whom various cardiopulmonary assistance techniques have been used [2,3,4]. The use of cardiopulmonary bypass (CPB), introduced in clinical practice since in the early 1980s, radically changed the approach to LT in more severely sick patients and allowed to treat cases in extremely serious conditions [5]. On the other hand, CPB implies the use of anticoagulants and the related increase in bleeding and inflammation associated with primary graft dysfunction (PGD) and pulmonary complications [6, 7]. Perioperative use of extracorporeal membrane oxygenation (ECMO) has been subsequently introduced in LT for rescue treatment of severe respiratory failure and advanced hemodynamic instability [6, 7]. Due to the centrifugal pump and closed-circuit membrane oxygenator, ECMO overcomes some of the CPB-related limitations as the necessity for high-dose heparin, the wide air-blood interface, and systemic inflammatory reaction [7, 8].
Extracorporeal carbon dioxide removal (ECCO2R) has been successfully used in moderate ARDS to selectively reduce arterial carbon dioxide partial pressure (PaCO2) [9]. This technique has the potential advantage, when compared to CPB and ECMO, of being partially associated with lower anticoagulation and device-related complications, with less invasiveness (i.e., single venous double-lumen catheter) [10]. Despite ECCO2R use is not associated with improved oxygenation, this device induces PaCO2 reduction by a single venous double lumen catheter at a lower flow rate than ECMO [11, 12]. In thoracic surgery, ECCO2R has been used before LT as a “bridge” to organ availability and in patients with PGD after LT, but there is no report on intraoperative ECCO2R use during LT [13, 14].
This case-matched cohort retrospective study in patients undergoing LT is intended to evaluate the role of intraoperative ECCO2R on emergency ECMO requirements.
Methods
The clinical records of all consecutive patients undergoing LT at Transplant Centre of Policlinico Umberto I, University of Rome “Sapienza”, Rome, Italy, between November 2007 and March 2014, were retrieved with the approval of the Ethical Committee of Policlinico Umberto I (Protocol Number 756/13). Patients were categorized according to the clinical conditions into 3 groups: “high”, “low,” and “intermediate” intraoperative severity. Patients receiving preoperatively extracorporeal lung support (ECMO or ECCO2R) as a bridge to transplant, those undergoing re-transplant or those who developed intraoperative severe acute hypoxemia (PaO2/FiO2 ≤150) or hemodynamic instability (mean arterial pressure (MAP) ≤ 60 mmHg and Cardiac Index (CI) ≤ 2.5 L/min/m2, despite vasopressors infusion) were considered “high severity” and excluded from data analysis. Patients that intraoperatively maintained respiratory stability (i.e., pH ≥7.25, PaCO2 ≤60 mmHg, and PaO2/FiO2 >150) were considered “low risk” and excluded from this data analysis. Patients that developed intraoperative severe respiratory acidosis with maintained oxygenation function (i.e., pH <7.25, PaCO2 >60 mmHg, and PaO2/FiO2 >150), not associated with hemodynamic instability, were considered at “intermediate” intraoperative severity and their data were selectively analyzed. Data from patients presenting “intermediate” intraoperative severity treated between in the intervals 2007–2010 or 2011–2014 were analyzed as a historical comparison of case-matched cohort. Patients with “intermediate” intraoperative severity treated in the 2007–2010 interval received “standard intraoperative treatment” as compared with those treated in the 2011–2014 interval that received “standard intraoperative treatment + ECCO2R.”
For both groups, “standard intraoperative treatment” included protective mechanical ventilation, permissive hypercapnia ≤60 mmHg, and inhaled nitric oxide or a continuous infusion of prostaglandin. Pressure controlled mechanical ventilation (Zeus® Infinity® Dräger, Germany) was set in order to achieve a tidal volume (TV) of 6–8 ml/kg, a plateau pressure <30 cmH2O, pulmonary end-expiratory pressure (PEEP) 6–8 cmH2O, and FiO2 up to obtain peripheral oxygen saturation (SpO2) >90% [15–17].
Dobutamine and norepinephrine were titrated to maintain a CI ≥2.5 L/min/m2 and a MAP ≥60mmHg. To reduce pulmonary hypertension and to avoid lung ischemic-reperfusion damages, inhaled nitric oxide (iNO) 10–20 ppm was administered (Optikinox® Air Liquide, France) along with prostaglandin E2 continuous intravenous administration at 10–20 ng/kg/min rate [18]. Anemia was treated with red blood cell pack transfusion, for hemoglobin values <9 g/dl. Patients who developed severe intraoperative hypoxemia (PaO2/FiO2 ≤150) or persistent severe respiratory acidosis (i.e., pH <7.25, PaCO2 >60 mmHg) received intraoperative ECMO. When ECMO was initiated during surgery, venous-arterial RotaFlow® (Maquet, Hirrlingen, Germany) was used after femoral artery and vein cannulation: the vein cannula was inserted using percutaneous Seldinger technique and the arterial with surgical preparation. Extracorporeal blood flow was started at 30% of CI. It was then modified according to hemodynamic parameters.
In patients undergoing LT during the 2011–2014 period and presenting “intermediate” clinical severity (i.e., pH <7.25, PaCO2 >60 mmHg, and PaO2/FiO2 >150), CO2 removal was achieved using ECCO2R (Prolung® device, Estor). The femoral or jugular vein was accessed via a double lumen catheter (14 F; Arrow International Inc. Reading PA) inserted and connected to the extracorporeal circuit. Blood flow was driven through the circuit by a non-occlusive low flow roller pump (80–350 ml/min) through a polimethylpentene oxygenator cartridge membrane connected to an 8 L/min sweep gas flow source delivering FiO2 1.0 oxygen.
The ECCO2R treatment was started at the intraoperative development of severe respiratory acidosis with maintained oxygenation function (i.e., pH <7.25, PaCO2 >60 mmHg, and PaO2/FiO2 >150) that always occurred after the beginning of the first OLV and before the clamping of the pulmonary artery.
Heparin continuous infusion administration of 10–15 IU/kg/h was used as an anticoagulant to maintain activated clotting time (ACT) between 120 and 150s in patients undergoing ECCO2R, while in patients undergoing ECO our anticoagulation target was an ACT between 180 and 200s with an activated partial thromboplastin Time (aPTT) ratio >2.
The following variables were recorded in all patients: MAP, heart rate (HR), mPAP, CI (Vigilance®, Edwards Lifescienses System), central venous pressure (CVP), mixed O2 venous saturation (SvO2), CO2 end-tidal (EtCO2), SpO2, body temperature, and diuresis. The primary endpoint was the emergency ECMO requirement in the 2 groups. Secondary endpoints were efficacy of ECCO2R measured as changes in blood gas analysis (BGA) and impact on systemic and pulmonary hemodynamic (i.e., MAP, HR, and mPAP) recorded every 20 min after the beginning of CO2 removal and throughout the intraoperative period. Length of intensive care unit (ICU) stay, duration of postoperative mechanical ventilation, and mortality at 30 postoperative days were also recorded. Complications related to ECCO2R use were also recorded, including mechanical complications due to circuit components or pump malfunction and patient-related complications: vascular damages, bleeding, hemodynamic instability, myocardial dysfunction, or cardiac arrhythmias and intravascular embolism.
Continuous variables were described by medians (interquartile ranges) or mean (standard deviation) as appropriate. SPSS Software (IBM) was used for statistical analysis. To evaluate differences between the 2 groups, Fisher’s exact test and χ2 test with 95% confidence intervals for categorical variables was used; Student’s t test was used to analyze continuous variables. Statistical significance was set at a p value lower than 0.05 for all variables. Assuming that 20% of the subjects in the reference population have the factor of interest, and after applying continuity correction, the study would require a sample size of 15 for each group (i.e., a total sample size of 30, assuming equal group sizes), to achieve a power of 80% for detecting a difference in proportions of 0.6 between the two groups (test - reference group) at a two-sided p value of 0.05.
Results
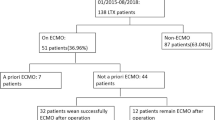
Seventy-four patients underwent LT at the Transplant Centre of Policlinico Umberto I “Sapienza” University of Rome between November 2007 and March 2014, 9 of these were excluded from the study, 8 received ECMO or ECCO2R as a “bridge” to transplant, and 1 was recipient of re-transplant (Fig. 1). Out of the remaining 65 patients, 38 presented “intermediate” intraoperative severity, 23 in the 2007–2010 and received “standard intraoperative treatment,” and 15 in the 2011–2014 and received “standard intraoperative treatment + ECCO2R”. There were no significant differences in demographic, baseline hemodynamic, and blood gasses data (Table 1).
Flow-chart of the study protocol. Legend: Between November 2007 and March 2014, 74 patients underwent lung transplantation, and 9 of these were excluded from the study because of urgent surgery or retransplant. Out of the remaining 65 patients, 38 presented “intermediate” intraoperative severity: 23 patients in the 2007–2010 who “received standard intraoperative treatment,” 15 patients in the 2011–2014 who received “standard intraoperative treatment + extracorporeal carbon dioxide removal (ECCO2R). “Intermediate” intraoperative severity: patients who developed intraoperative severe respiratory acidosis with maintained oxygenation function (i.e., pH <7.25, paCO2 >60mmHg PaO2/FiO2 >150), not associated with hemodynamic instability
The need for ECMO, in patients that presented “intermediate” intraoperative severity, was more frequent among patients treated in the 2007–2010 period that received “standard intraoperative treatment” alone than in those treated in the 2011–2014 period that received “standard intraoperative treatment + ECCO2R” (17/23 vs. 3/15; p = 0.004) (Table 2).
Urgent ECMO was used in 20 patients, 3 (20%) in standard intraoperative treatment + ECCO2R group, and 17 (73.9%) in standard intraoperative treatment group (p: 0.004 OR = 11.3 CI = 2.36–54.5) (Table 2).
In the “Standard intraoperative treatment” group, acidosis and hemodynamic instability were determining factors for urgent ECMO: in 8 patients, it happened during the first OLV period, in 4 patients during the first pulmonary artery clamping, in 2 patients during the second OLV time, in the last 3 patients after the second pulmonary artery clamping.
In the “Standard intraoperative treatment + ECCO2R” group, causing factors for ECMO were mainly respiratory adverse events, during the second pulmonary artery clamping, related to the PGD of the first lung implanted.
Data analysis of hemodynamic and respiratory variables showed a decrease in mPAP and PaCO2 values along with an improvement in pH values, starting after 20 min and thereafter throughout the intraoperative period, while systemic hemodynamic variables and PaO2/FiO2 remained stable (Table 3, Fig. 2). The 30-day mortality rate was 20% (3/15) in the “standard intraoperative treatment + ECCO2R” group and 39% (9/23) in the “standard intraoperative treatment” (p = 0.55). Mortality among patients who received ECMO was similar among “standard intraoperative treatment + ECCO2R” and “standard intraoperative treatment” (3/15, 20% vs 9/23, 39.1%).
Changes in PaCO2, mPAP and pH in the 15 patients undergoing ECCO2R. Legend: PaCO2 = Arterial Carbon Dioxide Partial Pressure; mPAP = mean pulmonary artery blood pressure; T0 = double lung ventilation at the beginning of LT; T1 = single lung ventilation (preclamping of the pulmonary artery); T2 = clamping of the pulmonary artery; T3= after 40 min from clamping; T4 = after 90 min from clamping; T5 = after 120 min from clamping; T6 = declamping of the pulmonary artery; primary axis (on the left) = values of PaCO2 and mPAP in mmHg; secondary axis (on the right) = values of pH. All values are reported as mean and standard deviation. ECCO2R was started between T1 and T2 and continued until the end of the surgery
Complications of ECCO2R included tube damages occurred twice with the system, but never with ECMO circuit. Three patients required wound and thoracic surgical revision because of ECMO-related bleeding (1 in the “standard intraoperative treatment + ECCO2R” group and 2 in the “standard intraoperative treatment” group). No other complications were reported.
Discussion
This case-matched cohort retrospective study, in patients undergoing LT and presenting “intermediate” clinical severity, originally reports that intraoperative ECCO2R decreases emergency ECMO requirement. In these patients, when intraoperative respiratory acidosis develops, ECCO2R use safely and effectively blunts pH/PaCO2 changes and associates with reduced mPAP (Fig. 2). These results confirm the efficacy of ECCO2R in CO2 removal, already proven in ultraprotective ventilation in chronic obstructive pulmonary disease (COPD) and in ARDS patients, and extend its role to the perioperative treatment of patients undergoing LT [19,19,21]. Limited and promising evidence is currently available on the perioperative use of ECCO2R in thoracic surgery, and these include a 69-year-old man undergone left pneumonectomy treated with resection of a single right upper lobe lesion; and the report of ECCO2R adjunct to conventional treatment as a bridge to LT [22]. The ECCO2R use has also been tested in the immediate postoperative period in case PGD when conventional therapies (ventilatory support, inhaled nitric oxide administration, and intravenous prostaglandin) were not sufficient to provide adequate gas exchange and control pulmonary hypertension [23,23,25].
Patients selected for this cohort study represent an “intermediate group” in terms of clinical severity, do not present severe hypoxemia, are not receiving preoperative extracorporeal lung support with either ECMO or ECCO2R, and are not scheduled for re-transplant neither present with severe refractory arterial hypotension or reduced CI; on the other hand, the respiratory function was severely compromised and associated with advanced respiratory acidosis. For this reason, we consider that the presented data intended to fulfill the need for a therapeutic intraoperative “precision medicine” strategy [26]. In both groups, a protective mechanical ventilation strategy was set according to the recommendations to minimize the ventilator-induced lung injury and in particular hyperinflation [17]. Prior to inclusion mechanically ventilated patients presented a hypercapnia (PaCO2 >60mmHg) and respiratory acidosis (pH< 7.25), while ventilation was optimized within the limitations imposed by lung-protective ventilation [17, 27]. Permissive hypercapnia with moderate respiratory acidosis (PaCO2 40–60 mmHg with pH >7.25) was considered acceptable in order to reduce the risk of dynamic hyperinflation, barotrauma, and volutrauma [28]. Patients presenting severe intraoperative respiratory acidosis (i.e., pH <7.25 and PaCO2 >60 mmHg) were free from metabolic and perfusion mismatch, maintaining a MAP ≥60 mmHg and CI ≥2.5 l/min/m2, with or without vasopressors infusion [27, 28]. Patients with severe hypoxemia PO2/FiO2 <150 were excluded and underwent to an ECMO support.
Study limitations
The present study has some limitations: first, it is a single-center case-matched cohort retrospective study. This methodological approach does not provide evidence that possesses an equivalent strength than those derived by a randomized controlled trial; furthermore, we could not apply matched analysis techniques with propensity score without significantly reducing the sample size. Nevertheless, the number of recruited patients (based on a dedicated sample size calculation) is sufficient to support the presented results and it should be considered as a preliminary experience for designing a multicenter prospective study.
Conclusion
In conclusion, intraoperative ECCO2R use in patients undergoing LT is safe and along with “optimal” mechanical ventilation and hemodynamic management, effectively contributes to prevent respiratory acidosis and hypercapnia. This approach, when accomplished in patients presenting with “intermediate severity” and compared to ECMO has the advantage of using smaller intravascular cannulation and lower blood flow, thus exposing to a reduced risk for vascular damage and bleeding complications. The safety and efficacy of intraoperative ECCO2R use potentially make this treatment a safe and useful step into an escalating step-wise work-up to support respiratory function in patients undergoing LT. Future studies are necessary to define the clinical indications, to improve the design of membrane CO2 removal, and to further reduce invasiveness.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ECCO2R:
-
Extracorporeal carbon dioxide removal
- ECMO:
-
Extracorporeal membrane oxygenation
- CO2 :
-
Carbon dioxide
- LT:
-
Lung transplantation
- PaCO2 :
-
Arterial carbon dioxide partial pressure
- mPAP:
-
Mean pulmonary artery pressure
- CPB:
-
Cardiopulmonary bypass
- PGD:
-
Primary graft dysfunction
- ARDS:
-
Acute respiratory distress syndrome
- TV:
-
Tidal volume
- PEEP:
-
Pulmonary end-expiratory pressure
- FiO2 :
-
Fraction of inspired oxygen
- SpO2 :
-
Peripheral oxygen saturation
- MAP:
-
Mean arterial pressure
- CI:
-
Cardiac Index
- iNO:
-
Inhaled nitric oxide
- ACT:
-
Activated clotting time
- aPTT:
-
Activated partial thromboplastin time
- HR:
-
Heart rate
- CVP:
-
Central venous pressure
- SvO2 :
-
Mixed oxygen venous saturation
- EtCO2 :
-
End-tidal CO2
- BGA:
-
Blood gas analysis
- ICU:
-
Intensive care unit
- COPD:
-
Chronic obstructive pulmonary disease
- OLV:
-
One lung ventilation
- SLT:
-
Single lung transplant
- DSLT:
-
Double sequential lung transplant
References
Hoechter DJ, Von Dossow V (2016) Lung transplantation: from the procedure to managing patients with lung transplantation. Curr Opin Anaesthesiol 29:8–13
Nagendran M, Maruthappu M, Sugand K (2011) Should double lung transplant be performed with or without cardiopulmonary bypass? Interact Cardiovasc Thorac Surg 12:799–804
Ius F, Tudorache I, Warnecke G (2018) Extracorporeal support, during and after lung transplantation: the history of an idea. J Thorac Dis 10:5131–5148
Machuca TN, Collaud S, Mercier O, Cheung M, Cunningham V, Kim SJ et al (2015) Outcomes of intraoperative extracorporeal membrane oxygenation versus cardiopulmonary bypass for lung transplantation. J Thorac Cardiovasc Surg 149:1152–1157
Reitz BA, Burton NA, Jamieson SW, Bieber CP, Pennock JL, Stinson EB, Shumway NE (1980) Heart and lung transplantation: autotransplantation and allotransplantation in primates with extended survival. J Thorac Cardiovasc Surg 80:360–372
Bermudez CA, Shiose A, Esper SA, Shigemura N, D’Cunha J, Bhama JK et al (2014) Outcomes of intraoperative venoarterial extracorporeal membrane oxygenation versus cardiopulmonary bypass during lung transplantation. Ann Thorac Surg 98:1936–1942
Biscotti M, Yang J, Sonett J, Bacchetta M (2014) Comparison of extracorporeal membrane oxygenation versus cardiopulmonary bypass for lung transplantation. J Thorac Cardiovasc Surg 148:2410–2405
Rali AS, Chandler J, Sauer A, Solomon MA, Shah Z (2021) Venoarterial extracorporeal membrane oxygenation in cardiogenic shock: lifeline of modern day CICU. J Intensive Care Med 36(3):290–303
Abrams D, Brodie D (2017) Extracorporeal membrane oxygenation for adult respiratory failure: 2017 update. Chest 152:639–649
Combes A, Fanelli V, Pham T, Ranieri VM, European Society of Intensive Care Medicine Trials Group and the “Strategy of Ultra-Protective lung ventilation with extracorporeal CO2 removal for new-onset moderate to severe ARDS” (SUPERNOVA) investigators (2019) Feasibility and safety of extracorporeal CO2 removal to enhance protective ventilation in acute respiratory distress syndrome: the SUPERNOVA study. Intensive Care Med 45:592–600
Boyle AJ, Sklar MC, McNamee JJ, Brodie D, Slutsky AS, Brochard L, McAuley DF, International ECMO network (ECMONet) (2018) Extracorporeal carbon dioxide removal for lowering the risk of mechanical ventilation: research questions and clinical potential for the future. Lancet Respir Med 6:874–884
Alessandri F, Pugliese F, Mascia L, Ranieri MV (2018) Intermittent extracorporeal CO2 removal in chronic obstructive pulmonary disease patients: a fiction or an option. Curr Opin Crit Care 24:29–34
Ricci D, Boffini M, Del Sorbo L, El Qarra S, Comoglio C, Ribezzo M et al (2010) The use of CO2 removal devices in patients awaiting lung transplantation: an initial experience. Transplant Proc 42:1255–1258
Moscatelli A, Ottonello G, Nahum L, Lampugnani E, Puncuh F, Simonini A et al (2010) Noninvasive ventilation and low-flow veno-venous extracorporeal carbon dioxide removal as a bridge to lung transplantation in a child with refractory hypercapnic respiratory failure due to bronchiolitis obliterans. Pediatr Crit Care Med 11:8–12
Nicoara A, Anderson-Dam J (2017) Anesthesia for Lung Transplantation. Anesthesiol Clin 35:473-489
Kachulis B, Mitrev L, Jordan D (2017) Intraoperative anesthetic management of lung transplantation patients. Best Pract Res Clin Anaesthesiol 31:261–272
Lucangelo U, Del Sorbo L, Boffini M, Ranieri VM (2012) Protective ventilation for lung transplantation. Curr Opin Anaesthesiol 25:170–174
Waldow T, Alexiou K, Witt W et al (2004) Protection of lung tissue against ischemia/reperfusion injury by preconditioning with inhaled nitric oxide in an in situ pig model of normothermic pulmonary ischemia. Nitric Oxide 10:195–201
Terragni PP, Del Sorbo L, Mascia L, Urbino R, Martin EL, Birocco A et al (2009) Tidal volume lower than 6 ml/kg enhances lung protection: role of extracorporeal carbon dioxide removal. Anesthesiology 111:826–835
Del Sorbo L, Pisani L, Filippini C, Fanelli V, Fasano L, Terragni P et al (2015) Extracorporeal CO2 removal in hypercapnic patients at risk of noninvasive ventilation failure: a matched cohort study with historical control. Crit Care Med 43:120–127
McRae K, de Perrot M (2018) Principles and indications of extracorporeal life support in general thoracic surgery. J Thorac Dis 10:S931–S946
Iacovazzi M, Oreste N, Sardelli P, Barrettara B, Grasso S (2012) Extracorporeal carbon dioxyde removal for additional pulmonary resection after pneumonectomy. Minerva Anestesiol 78:381–384
Ruberto F, Bergantino B, Testa MC, D’Arena C, Zullino V, Congi P et al (2013) Low-flow venoveous CO2 removal in association with lung protective ventilation strategy in patients who develop severe progressive respiratory acidosis after lung transplantation. Transplant Proc 45:2741–2745
Ruberto F, Bergantino B, Testa MC, D’Arena C, Bernardinetti M, Diso D et al (2014) Low-flow veno-venous extracorporeal CO2 removal: first clinical experience in lung transplant recipients. Int J Artif Organs 37:911–917
Ruberto F, Pugliese F, D'Alio A, Perrella S, D’Auria B, Ianni S et al (2009) Extracorporeal removal CO2 using a venovenous, low-flow system (Decapsmart) in a lung transplanted patient: a case report. Transplant Proc 41:1412–1414
Goligher EC, Amato MBP, Slutsky AS (2017) Applying precision medicine to trial design using physiology. Extracorporeal CO2 removal for acute respiratory distress syndrome. Am J Respir Crit Care Med 196:558–568
Hilty MP, Riva T, Cottini SR, Kleinert EM, Maggiorini A, Maggiorini M (2017) Low flow veno-venous extracorporeal CO2 removal for acute hypercapnic respiratory failure. Minerva Anestesiol 83:812–823
Morisaki H, Serita R, Innami Y, Kotake Y, Takeda J (1999) Permissive hypercapnia during thoracic anaesthesia. Acta Anaesthesiol Scand 43:845–849
Acknowledgements
Not applicable.
Funding
The authors declare that they have no competing interests and no financial interests. They have no funding source.
Author information
Authors and Affiliations
Contributions
FR, FA, and MP were responsible for the conception, design, analysis, and writing of the study; FR, MP, KB, PC, DD, and FV were involved with the collection and interpretation of data; FR, MP, FA, VZ, FV, FB, and FP participated in data management, review, and editing of the manuscript. The authors have approved the submitted version of the manuscript and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethical Committee of Policlinico Umberto I, Rome (Protocol Number 756/13).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ruberto, F., Alessandri, F., Piazzolla, M. et al. Intraoperative use of extracorporeal CO2 removal (ECCO2R) and emergency ECMO requirement in patients undergoing lung transplant: a case-matched cohort retrospective study. J Anesth Analg Crit Care 2, 22 (2022). https://doi.org/10.1186/s44158-022-00050-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44158-022-00050-x