Abstract
Background
A reduction in right ventricular (RV) function during recovery from prolonged endurance exercise has been documented alongside RV dilatation. A relative elevation in pulmonary artery pressure and therefore RV afterload during exercise has been implicated in this post-exercise dysfunction but has not yet been demonstrated. The current study aimed to assess RV structure and function and pulmonary artery pressure before, during and after a 6-h cycling exercise bout.
Methods
Eight ultra-endurance athletes were recruited for this study. Participants were assessed prior to exercise supine and seated, during exercise at 2, 4 and 6 h whilst cycling seated at 75% maximum heart rate, and post-exercise in the supine position. Standard 2D, Doppler and speckle tracking echocardiography were used to determine indices of RV size, systolic and diastolic function.
Results
Heart rate and RV functional parameters increased from baseline during exercise, however RV structural parameters and indices of RV systolic and diastolic function were unchanged between in-exercise assessment points. Neither pulmonary artery pressures (26 ± 9 mmHg vs 17 ± 10 mmHg, P > 0.05) nor RV wall stress (7.1 ± 3.0 vs 6.2 ± 2.4, P > 0.05) were significantly elevated during exercise. Despite this, post-exercise measurements revealed RV dilation (increased RVD1 and 3), and reduced RV global strain (− 21.2 ± 3.5 vs − 23.8 ± 2.3, P = 0.0168) and diastolic tissue velocity (13.8 ± 2.5 vs 17.1 ± 3.4, P = 0.019) vs pre-exercise values.
Conclusion
A 6 h cycling exercise bout at 75% maximum heart rate did not alter RV structure, systolic or diastolic function assessments during exercise. Pulmonary artery pressures are not elevated beyond normal limits and therefore RV afterload is unchanged throughout exercise. Despite this, there is some evidence of RV dilation and altered function in post-exercise measurements.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Exercise induced changes in cardiac structure and function during recovery from prolonged endurance exercise have been well documented and are commonly referred to as exercise induced cardiac fatigue. Recent research has focused on the right ventricle (RV) and a reduction in both systolic and diastolic RV function has been reported from prolonged endurance exercise of several modalities [5, 21, 28, 31]. Dilatation of the RV is also evident following greater duration endurance exercise suggestive of a possible overload to the right heart [15, 25, 30]. Endurance cycling, the modality used in the current study, is among those associated with reduced RV function, as assessed by echocardiographic [32, 33] and cardiac MRI techniques [5].
The majority of studies investigating cardiac fatigue have focused on comparisons between pre-race and recovery measures, with a void in the literature focusing on the in-exercise response of the RV. There are a limited number of studies assessing cardiac function during exercise. An increase in RV systolic tissue velocity has been demonstrated during submaximal cycling exercise [11, 35] with results indicating a physiological linear response between increasing exercise intensity and increasing contractility. However, there are no data available to characterise the diastolic functional response of the RV during exercise. Using more novel techniques, Goebel et al. [11], Tan et al. [35] and La Gerche et al. [14] applied strain imaging to the RV during submaximal cycling, stress echo and progressive maximal cycling respectively and reported an increase in RV strain. Banks et al. [2] report a reduction in RV strain and strain rates at 150 min of running. However, participants in this study were transferred from the treadmill to echo bed and stopped exercising for the duration of the assessment. Heart rate drops significantly on exercise cessation and the echocardiograms were obtained with subjects in a supine as opposed to upright position therefore impacting on load and not giving a true reflection of in-exercise RV function. The equivocal results and short duration exercise stimuli employed make firm conclusions about the in-exercise RV response challenging.
Several possible mechanisms have been suggested to explain cardiac fatigue in the RV. These include beta-adrenergic receptor down-regulation [2] and subsequent reduction in contractility; inflammation or biomarker release [18]; or an elevated RV afterload secondary to a disproportionally elevated pulmonary compared to systemic pressure [17]. The pulmonary circulation has a limited capacity for vasodilation and therefore pulmonary artery pressures (PAP) during exercise are relatively higher when compared to the systemic circulation and can reach values indicative of pulmonary hypertension during prolonged endurance exercise [13]. La Gerche et al. have quantified this disproportionate RV exercise stroke work in a semi-supine progressive cycling exercise fitness test and reported significantly elevated PAP up to 61 mmHg during exercise. The use of cardiac MRI to derive RV end systolic volume and echocardiography to estimate PAP does not afford simultaneous assessment of the components that RV wall stress is calculated from and although the authors attempt to correct for the two techniques involved in the measurement, there is a large potential for error. The concurrent assessment of RV structure and function alongside pulmonary artery pressures using echocardiography may aid the understanding of temporal exercise induced changes in a prolonged upright exercise bout. The aim of this study is therefore to build on previous research and assess RV structure and function and pulmonary artery pressures before, at 2-h intervals during, and following a 6-h cycling exercise bout. We hypothesised that PAP would be elevated during prolonged strenuous cycling exercise and that RV dysfunction and structural enlargement would be present post-exercise.
Methods
Sample population
Eight well trained male ultra-endurance athletes (Body mass 77.8 ± 11 kg, height 179 ± 6 cm, BP 136/88 mmHg, age 40 ± 7 years, VO2 max 51.9 ± 10 ml kg min−1) gave written informed consent to participate in this study. Participants self-reported: no known cardiovascular disease, no prescribed medications and no comorbidities or family history of cardiovascular disease. Ethical approval was granted by the University Ethics Committee.
Protocols
Participants underwent a maximal oxygen uptake test (Oxycon, Care Fusion, Hoechberg, Germany and SRM bike, Jülich, Germany) at 30 W increments every 3 min to determine their maximum heart rate on a separate day to the 6-h cycling session. Participants were requested to avoid vigorous training, alcohol, and caffeine for a minimum of 24 h prior to the assessment. On the day of the cycling session, systolic and diastolic blood pressure was assessed prior to and immediately after exercise using standard auscultation (Dinamap pro, GE Healthcare, Horten, Norway). Echocardiography assessments were done prior to the exercise session in both supine and seated positions; at 2-, 4- and 6-h intervals during the exercise bout (seated cycling); and in the supine position immediately post exercise. All images were acquired using a commercially available ultrasound system (Vivid Q, GE Medical, Horten, Norway) with a 1.5–4 MHz phased array transducer. In-exercise images were obtained by a single experienced sonographer (DLO) with the participant on their own road cycling bike fixed to a turbo trainer device cycling at 75% maximum heart rate. Images were recorded to DVD in raw DICOM format and data were analysed offline by a single experience sonographer (RNL) using commercially available software (EchoPac version 7, GE Medical, Horten, Norway). A minimum of three cardiac cycles were averaged for all peak indices.
Conventional 2D, Doppler and tissue Doppler echocardiography
The RV was assessed in accordance with British Society of Echocardiography guidelines [38] providing structural indices at the outflow tract (RVOTplax, RVOT1, and RVOT2) and at the inflow (RVD1, RVD2, RVD3). RV diastolic area (RVAd) and systolic area (RVAs) were measured, and the fractional area change calculated (RVFAC). A pulsed wave tissue doppler imaging (TDI) sample positioned at the tricuspid annulus allowed the assessment of RV S’, E’ and A’ myocardial velocities. Right ventricular systolic pressure (RVSp) was derived from the tricuspid regurgitant jet (TR velocity) using continuous wave Doppler. The regurgitant signal was improved for resting and exercise measurements using agitated saline administered via a three way stop cock cannula inserted into the antecubital vein as previously described [1]. This technique has been shown to improve the accuracy of both resting and exercising assessments of pulmonary artery pressures [20] and agitated saline was therefore administered to our participants immediately prior to echocardiographic assessment at rest, at 2, 4 and 6 h intervals into the cycling session and during post-exercise assessment. Pulmonary artery systolic pressure (PASP) was calculated as (PASP (mmHg) = RVSp + 5 mmHg). For RV end-systolic wall stress, Laplace’s law was used to calculate according to the formula Pr/2 h where P (pressure) was quantified as PASP, r (radius) was calculated using the formula r = \({0.620(\mathrm{RVSa})}^\frac{1}{3}\), assuming spherical geometry as previously described [24] and h was quantified as RV wall thickness.
2D myocardial speckle tracking
Based on a previous study by our group suggesting limited feasibility, comparability and reliability of myocardial speckle tracking to derive RV longitudinal strain above 50% maximum heart rate, we have only assessed RV strain at rest pre and post-exercise [23]. A modified apical 4 chamber image with lateral transducer movement was acquired for assessment of the RV strain. For all images the system was optimised as previously described [30]. Offline analysis allowed the assessment of peak global longitudinal RV strain (calculated as an average of 6 myocardial segments from base to apex of the RV free wall and septum) and RV free wall strain calculated as an average of the 3 myocardial basal, mid and apical segments of the RV free wall.
Statistics
Echocardiographic data were analysed for normality of distribution using a Shapiro–Wilk test. Seated baseline and peak data at 2, 4 and 6 h of exercise were compared using a one-way repeated measures ANOVA. Pre- to post-exercise supine data were compared using a paired samples T-test. All statistical tests were performed using commercially available software (IBM SPSS version 22) and statistical significance was set as P < 0.05.
Results
Exercise responses
Heart rate was significantly higher during exercise at 2, 4 and 6 h compared to baseline (P = 0.04, 0.04 and 0.03 respectively, Table 1). There was a significant increase (P = 0.003) in TAPSE from baseline to 4 h and RV S’ and RV A’ were also significantly elevated (P = 0.001, 0.015 and 0.006 and > 0.001 respectively, Table 1) from baseline at 2, 4 and 6 h into exercise. There were no significant differences in RVFAC, TR velocity, PASP or RV wall stress from baseline to in-exercise measures (P > 0.05, Table 1). There were also no significant differences in RV structural parameters RVOTplax, RVOT1, RVOT2, RVD1, RVD2, RVD3, RVAd and RVAs from baseline to in-exercise assessment points (P > 0.05, Table 1).
Pre- and post-exercise comparison
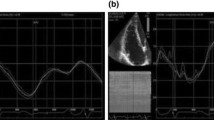
Body mass (77.8 ± 11 and 78 ± 11.3 kg) and diastolic blood pressure (78 ± 8 and 70 ± 5 mmHg) were unchanged pre- to post-exercise (P > 0.05). Heart rate (HR) was significantly increased post-exercise (75 ± 11 beats min−1) compared to pre-exercise (55 ± 10 beats min−1, P = 0.001) and systolic blood pressure was significantly reduced (P = 0.04) pre- to post-exercise (136 ± 13 to 123 ± 10 mmHg). Structural parameters RVOTplax, RVOT 1 and 2, RVD2, RVAd, and RVAs were not significantly different pre- to post-exercise (P > 0.05, Table 2). In contrast, RVD1 and RVD3 were significantly larger post-exercise versus baseline (RVD1 50.0 ± 2.5 mm vs 46.4 ± 4.7, P = 0.02; RVD3 88.4 ± 4.7 vs 84.8 ± 5.4 mm, P = 0.02; Fig. 1A, B). With respect to functional parameters, TAPSE, S’, A’, TR velocity, PASP, RV wall stress and RV free wall strain were not significantly different pre- to post-exercise (P > 0.05, Table 2). However, RV global strain (− 21.2 ± 3.5 vs − 23.8 ± 2.3, P = 0.02) and E’ (13.8 ± 2.5 vs 17.1 ± 3.4, P = 0.02) were significantly reduced post-exercise versus baseline (Fig. 1C, D).
Discussion
This study investigated the factors contributing to reduced RV function after endurance exercise, using echocardiographic assessment of RV function in athletes before, during, and after a 6-h cycling bout. Contrary to our hypothesis that increased PAP and RV afterload would occur during exercise and precede a reduction in RV function, we measured no PAP or afterload changes during exercise, despite evidence of RV dilation and reduced systolic and diastolic function post-exercise.
RV dilation and dysfunction post-exercise
A dilation of the RV and reduction in systolic and diastolic function after ultra-endurance exercise has been reported by several groups using a range of echocardiographic techniques and indices [8, 15, 16, 26, 30]. Increased RV size, reduced RV lateral wall myocardial annular velocities, and lower RV strain suggest reduction in myocardial relaxation and contraction post-exercise. These changes are generally transient, with most parameters returning to baseline levels within days [15, 16]. There is some evidence that RV strain rate remains reduced 6–11 days after the end of the exercise stimulus [15], although the time to recovery remains unclear.
The commonly accepted potential mechanism responsible for these RV changes centers on an elevated PASP during exercise resulting in a disproportionate afterload for the RV during exercise [17, 30]. Increased PAP in endurance exercise has been demonstrated by both echocardiographic [28] and direct right heart catheterisation [4] methods. Indeed, two meta-analyses have supported the notion that PAP often exceeds 30 mmHg during exercise and is dependent, in part, on age and exercise intensity [9, 13]. Moreover, trained athletes have a greater PAP both at rest [7] and during exercise compared to untrained individuals [6, 9, 19, 36], likely secondary to an increased RV stroke volume and inability of the pulmonary vasculature to vasodilate to the same degree as the systemic vasculature. Reduced RV function with a concurrent increase in PASP was reported by Neilan et al. but not by Buchan et al., although this discrepancy could be attributed to the much shorter exercise stimulus duration used in the latter study. Others have previously shown a decline in RV function with a reduction in PASP [15], whilst we previously found no change in PASP [22]. This variability could result from the measurements being taken after the exercise stimulus had finished, with the participant supine, and from the variable relative exercise intensity that participants exercised at. Thus, we expected that the current data would demonstrate detectable increases in PASP and RV afterload during exercise. Interestingly, although a non-significant 50% increase in PASP was evident 6-h into exercise, RV wall stress (as a surrogate of afterload) was not elevated at 2-, 4- or 6-h into the 6-h exercise bout. Despite this, a post-exercise dilation of the RV alongside a reduction in both systolic and diastolic function was evident. Thus, post-exercise RV dysfunction occurred in the setting of detectable increases in PASP but not RV afterload during exercise, raising the possibility that elevated PAP may partially explain RV dysfunction after 6-h of prolonged cycling. Alternative mechanisms may therefore contribute to some degree of RV dysfunction, or our non-invasive surrogate of RV afterload may not be sensitive enough to detect elevations during exercise.
Downregulation and/or desensitisation of the cardiac beta-adrenergic receptors secondary to prolonged catecholamine exposure has been proposed as a mechanism for exercise-induced cardiac fatigue in the right and left ventricle. In support of this, human studies have consistently demonstrated that the cardiovascular response to a beta-adrenergic agonist (dobutamine) is reduced following a period of endurance exercise [2, 10, 12, 37], even under parasympathetic blockade [12]. As such, exercise-induced reductions in beta-adrenergic receptor activity may explain the decline in RV function following endurance activities. However, it has also been consistently demonstrated that endurance-exercise induced fatigue affects the right ventricle more (or sooner) than the left ventricle. In studies assessing the endurance-exercise response of both ventricles, left ventricular function remains normal whilst right ventricular function has declined [5, 15, 30]. It is unclear why beta-adrenergic desensitisation/downregulation would affect the RV more than the LV, unless receptor expression or density differs between ventricles. Human right and left ventricles (albeit donated by patients receiving a transplant following severe cardiomyopathy) were shown to contain a similar number of beta-adrenergic receptors and similar distribution of beta-1 and beta-2 subtypes [3]. As such, a beta-adrenergic mechanism may not underlie RV dysfunction following endurance exercise.
Alternatively, an overload-induced inflammatory response has also been suggested as a potential mechanism for RV dysfunction. The increase in certain inflammatory markers (TNF-alpha, IL-12, IL-1 beta) after endurance exercise was correlated with indices of cardiac damage (troponin, B-type natriuretic peptide) and was greater in participants showing RV dysfunction versus those that did not [18]. However, these data do not demonstrate causation, and further work is required to establish that endurance exercise does not simply drive both the inflammatory response and RV dysfunction via separate mechanisms.
RV function during exercise
The lack of observable change in RV function during exercise in the current study is intriguing, given that we found reduced RV function in the post-exercise data and that others report altered RV function following exercise durations much shorter than 6-h [28, 29, 31]. Cycling was chosen as the exercise mode for the current study given its practical advantages for in-exercise echocardiography, although it has significantly lower energy demands than running, rowing and triathlon [27] and this may explain the maintenance of RV structure and function during exercise. However, in-exercise indices of RV work (TAPSE, S’, A’) increased as expected and in line with previous reports in athletic populations [14, 23, 34]. Thus, the current cohort did not show a lower-than-expected response to endurance exercise. Pre-event training is another factor that could explain the lack of in-exercise alteration to RV function. The magnitude of RV dysfunction after endurance exercise is inversely related to the amount of pre-endurance-event training, such that RV dysfunction was greater in those completing less training [28]. As such, a high level of pre-study training relative to the study exercise stimulus could have prevented observable changes to RV function in the current cohort. However, the participants were completing a comparable level of training as in other athletic cohorts and none had competed in an endurance event for 2 weeks prior to the study. Alternatively, participant position during echocardiographic assessment completed whilst cycling may impact measurement of RV function. Few studies have assessed RV structure, function, or PAP during exercise in an upright position and the effect of gravity on these parameters remains to be determined. Indeed, the previous studies estimating PAP during exercise have done so with participants in a supine or semi-supine position, and the effect of modifying body position when obtaining the tricuspid regurgitant signal during exercise is unknown. Assessment of PASP is more accurate using agitated saline and further work using this technique is required to establish the response of the pulmonary circulation across a range of exercise modes, intensities, and durations to determine the relative afterload placed on the RV during exercise and the consequent acute structural and functional adaptations. Furthermore, studies using echocardiography to investigate RV exercise-induced cardiac fatigue have assessed participants prior to and on completion of exercise in a supine position and not considered the effect of body position on cardiac structure and function. Most exercise is undertaken in an upright position and to truly understand the effects of exercise on cardiac structure and function, it is pertinent for assessments to be undertaken in the exercising body position to ensure that loading conditions are relevant for in-exercise assessments.
Limitations
The small sample sized included in the current study likely influences statistical power and may, in part, explain the lack of statistical change evident in the in-exercise data. The use of a semi-supine cycle ergometer may improve image quality and afford the use of speckle tracking to assess athletes during exercise and allow the assessment of RV and LV function using a superior technique and in multiple planes. Repeated assessments of PAP during exercise would confirm whether PAP is elevated during exercise when assessed using non-invasive TR velocity-based measures. The use of 3D echo would improve structural assessment; however the frame rates are not sufficient to allow valid assessment of function especially during exercise at higher heart rates. Finally, the study did not assess LV function during or after exercise, limiting the interpretation of LV-RV dynamics.
Conclusion
A 6-h cycling exercise bout at 75% maximum heart rate results in RV dilation and reduced RV function, however this was only evident post-exercise, with normal RV structure and function maintained during exercise. There was no evidence of increased PAP during exercise, suggesting that the RV is not placed under a higher afterload during prolonged cycling. As such, endurance exercise-induced RV dysfunction and dilation does not appear to be driven by an elevated RV afterload. Further work is needed to determine the mechanisms underlying RV dysfunction after endurance cycling.
Availability of data and materials
Datasets generated in the study are not publicly available to protect participant privacy but are available from the corresponding author upon reasonable request.
Abbreviations
- HR:
-
Heart rate
- PAP:
-
Pulmonary artery pressure
- PASP:
-
Pulmonary artery systolic pressure
- PLAX:
-
Parasternal long axis view
- RV:
-
Right ventricle
- RV A’:
-
Right ventricular late diastolic myocardial tissue velocity
- RV E’:
-
Right ventricular early diastolic myocardial tissue velocity
- RV S’:
-
Right ventricular systolic myocardial tissue velocity
- RVAd:
-
Right ventricular diastolic area
- RVAs:
-
Right ventricular systolic area
- RVD:
-
Right ventricular dimension
- RVFAC:
-
Right ventricular fractional area change
- RVOT:
-
Right ventricular outflow tract
- RVSp:
-
Right ventricular systolic pressure
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TDI:
-
Tissue Doppler imaging
- VO2 max:
-
Maximal oxygen consumption rate
References
Badesch DB, Champion HC, Gomez Sanchez MA, Hoeper MM, Loyd JE, Manes A, Mcgoon M, Naeije R, Olschewski H, Oudiz RJ, Torbicki A. Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol. 2009;54:S55–66.
Banks L, Sasson Z, Busato M, Goodman JM. Impaired left and right ventricular function following prolonged exercise in young athletes: influence of exercise intensity and responses to dobutamine. J Appl Physiol. 2010;108:112–9.
Brodde OE, Schuler S, Kretsch R, Brinkmann M, Borst HG, Hetzer R, Reidemeister JC, Warnecke H, Zerkowski HR. Regional distribution of beta-adrenoceptors in the human-heart: coexistence of functional beta-1-adrenoceptor and beta-2-adrenoceptor in both atria and ventricles in severe congestive cardiomyopathy. J Cardiovasc Pharmacol. 1986;8:1235–42.
Buchan TA, Wright SP, Esfandiari S, Fuchs FC, Gray T, Currie KD, Sasson S, Sasson Z, Mak S, Goodman JM. Pulmonary hemodynamic and right ventricular responses to brief and prolonged exercise in middle-aged endurance athletes. Am J Physiol-Heart Circ Physiol. 2019;316:H326–34.
Claessen G, Claus P, Ghysels S, Vermeersch P, Dymarkowski S, La Gerche A, Heidbuchel H. Right ventricular fatigue developing during endurance exercise: a real-time exercise cardiac magnetic resonance imaging study. Acta Cardiol. 2014;69:72–72.
Claeys M, Claessen G, Claus P, De Bosscher R, Dausin C, Voigt J-U, Willems R, Heidbuchel H, La Gerche A. Right ventricular strain rate during exercise accurately identifies male athletes with right ventricular arrhythmias. Eur Heart J Cardiovasc Imaging. 2019;21:282–90.
D’andrea A, Riegler L, Golia E, Cocchia R, Scarafile R, Salerno G, Pezzullo E, Nunziata L, Citro R, Cuomo S, Caso P, Di Salvo G, Cittadini A, Russo MG, Calabrò R, Bossone E. Range of right heart measurements in top-level athletes: the training impact. Int J Cardiol. 2013;164:48–57.
Dávila-Román VG, Guest TM, Tuteur PG, Rowe WJ, Ladenson JH, Jaffe AS. Transient right but not left ventricular dysfunction after strenuous exercise at high altitude. J Am Coll Cardiol. 1997;30(2):468–73. https://doi.org/10.1016/s0735-1097(97)00179-4.
Dawkins TG, Curry BA, Wright SP, Meah VL, Yousef Z, Eves ND, Shave RE, Stembridge M. Right ventricular function and region-specific adaptation in athletes engaged in high-dynamic sports: a meta-analysis. Circ Cardiovasc Imaging. 2021;14:E012315.
Eysmann SB, Gervino E, Vatner DE, Katz SE, Decker L, Douglas PS. prolonged exercise alters beta-adrenergic responsiveness in healthy sedentary humans. J Appl Physiol. 1996;80:616–22.
Goebel B, Arnold R, Koletzki E, Ulmer HE, Eichhorn J, Borggrefe M, Figulla HR, Poerner TC. Exercise tissue Doppler echocardiography with strain rate imaging in healthy young individuals: feasibility, normal values and reproducibility. Int J Cardiovasc Imaging. 2007;23(2):149–55. https://doi.org/10.1007/s10554-006-9130-7. Erratum in: Int J Cardiovasc Imaging. 2007;23(2):157.
Hart E, Dawson E, Rasmussen P, George K, Secher NH, Whyte G, Shave R. Beta-adrenergic receptor desensitization in man: insight into post-exercise attenuation of cardiac function. J Physiol. 2006;577:717–25.
Kovacs G, Berghold A, Scheidl S, Olschewski H. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J. 2009;34:888–94.
La Gerche A, Burns AT, D’hooge J, Macisaac AI, Heidbüchel H, Prior DL. Exercise strain rate imaging demonstrates normal right ventricular contractile reserve and clarifies ambiguous resting measures in endurance athletes. J Am Soc Echocardiogr. 2012;25:253-262.E1.
La Gerche A, Burns AT, Mooney DJ, Inder WJ, Taylor AJ, Bogaert J, Macisaac AI, Heidbuchel H, Prior DL. Exercise-induced right ventricular dysfunction and structural remodelling in endurance athletes. Eur Heart J. 2012;33:998–1006.
La Gerche A, Connelly KA, Mooney DJ, Maclsaac AI, Prior DL. Biochemical and functional abnormalities of left and right ventricular function after ultra-endurance exercise. Heart. 2008;94:860–6.
La Gerche A, Heidbuchel H, Burns AT, Mooney DJ, Taylor AJ, Pfluger HB, Inder WJ, Macisaac AI, Prior DL. Disproportionate exercise load and remodeling of the athlete’s right ventricle. Med Sci Sports Exerc. 2011;43:974–81.
La Gerche A, Inder WJ, Roberts TJ, Brosnan MJ, Heidbuchel H, Prior DL. Relationship between inflammatory cytokines and indices of cardiac dysfunction following intense endurance exercise. PLoS ONE. 2015;10:E0130031.
La Gerche A, Macisaac AI, Burns AT, Mooney DJ, Inder WJ, Voigt JU, Heidbüchel H, Prior DL. Pulmonary transit of agitated contrast is associated with enhanced pulmonary vascular reserve and right ventricular function during exercise. J Appl Physiol. 2010;109:1307–17.
Lopes LR, Loureiro MJ, Miranda R, Almeida S, Almeida AR, Cordeiro A, Cotrim C, Carrageta M. The usefulness of contrast during exercise echocardiography for the assessment of systolic pulmonary pressure. Cardiovasc Ultrasound. 2008;6:51.
Lord R, Oxborough D, Somauroo J, George K. Echocardiographic evidence of the cardiac stress of competing in ultra-endurance exercise. Deutsche Zeitschrift Für Sportmedizin. 2014;65:93–101.
Lord R, Somauroo J, Stembridge M, Jain N, Hoffman MD, George K, Jones H, Shave R, Haddad F, Ashley E, Oxborough D. The right ventricle following ultra-endurance exercise: insights from novel echocardiography and 12-lead electrocardiography. Eur J Appl Physiol. 2015;115:71–80.
Lord RN, George K, Jones H, Somauroo J, Oxborough D. Reproducibility and feasibility of right ventricular strain and strain rate (Sr) as determined by myocardial speckle tracking during high-intensity upright exercise: a comparison with tissue Doppler-derived strain and Sr in healthy human hearts. Echo Res Pract. 2014;1:31–41.
Marcus JT, Gan CTJ, Zwanenburg JJM, Boonstra A, Allaart CP, Gbtte MJW, Vonk-Noordegraaf A. Interventricular mechanical asynchrony in pulmonary arterial hypertension. J Am Coll Cardiol. 2008;51:750–7.
Martinez V, Sanz-De La Garza M, Grazioli G, Bijnens BH, Trape J, Garcia G, Corzan P, Clemente A, Gonzalez B, Sitges M. Cardiac performance after an endurance open water swimming race. Eur J Appl Physiol. 2019;119:961–70.
McKechnie JK, Leary WP, Noakes TD, Kallmeyer JC, MacSearraigh ET, Olivier LR. Acute pulmonary oedema in two athletes during a 90-km running race. S Afr Med J. 1979;56(7):261–5.
Millet G, Vleck VE, Bentley DJ. Physiological differences between cycling and running. Sports Med. 2009;39:179–206.
Neilan TG, Yoerger DM, Douglas PS, Marshall JE, Halpern EF, Lawlor D, Picard MH, Wood MJ. Persistent and reversible cardiac dysfunction among amateur marathon runners. Eur Heart J. 2006;27:1079–84.
Oxborough D, Shave R, Middleton N, Whyte G, Forster J, George K. The impact of marathon running upon ventricular function as assessed by 2d, Doppler, and tissue-Doppler echocardiography. Echocardiography. 2006;23:635–41.
Oxborough D, Shave R, Warburton D, Williams K, Oxborough A, Charlesworth S, Foulds H, Hoffman MD, Birch K, George K. Dilatation and dysfunction of the right ventricle immediately after ultraendurance exercise: exploratory insights from conventional two-dimensional and speckle tracking echocardiography. Circ Cardiovasc Imaging. 2011;4:253–63.
Poh KK, Ton-Nu TT, Neilan TG, Tournoux FB, Picard MH, Wood MJ. Myocardial adaptation and efficiency in response to intensive physical training in elite speedskaters. Int J Cardiol. 2008;126:346–51.
Stewart GM, Chan J, Yamada A, Kavanagh JJ, Haseler LJ, Shiino K, Sabapathy S. Impact Of high-intensity endurance exercise on regional left and right ventricular myocardial mechanics. Eur Heart J-Cardiovascr Imaging. 2017;18:688–96.
Stewart GM, Yamada A, Haseler LJ, Kavanagh JJ, Chan J, Koerbin G, Wood C, Sabapathy S. Influence Of exercise intensity and duration on functional and biochemical perturbations in the human heart. J Physiol-Lond. 2016;594:3031–44.
Stoylen A, Wisloff U, Slordahl S. Left ventricular mechanics during exercise: a Doppler and tissue Doppler study. Eur J Echocardiogr. 2005;4:286–91.
Tan YT, Wenzelburger F, Lee E, Heatlie G, Leyva F, Patel K, Frenneaux M, Sanderson JE. The pathophysiology of heart failure with normal ejection fraction: exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. J Am Coll Cardiol. 2009;54(1):36–46. https://doi.org/10.1016/j.jacc.2009.03.037.
Tran M, Kwon A, Holt D, Kierle R, Fitzgerald B, Scalia I, Scalia W, Holt G, Scalia G. Echocardiographic pulmonary to left atrial ratio (Eplar): a comparison study between ironman athletes, age matched controls and a general community cohort. J Clin Med. 2019;8:1756.
Welsh RC, Warburton DE, Humen DP, Taylor DA, Mcgavock J, Haykowsky MJ. Prolonged strenuous exercise alters the cardiovascular response to dobutamine stimulation in male athletes. J Physiol. 2005;569:325–30.
Zaidi A, Knight DS, Augustine DX, Harkness A, Oxborough D, Pearce K, Ring L, Robinson S, Stout M, Willis J, Sharma V. Echocardiographic assessment of the right heart in adults: a practical guideline from the British Society of Echocardiography. Echo Res Pract. 2020;7:G19–41.
Acknowledgements
We would like to thank the participants for dedicating their time to taking part in this study.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
RL, JS, and DO collected the data. RL, KG, JS, HJ, and DO designed the study. RL and ZA drafted the manuscript. All authors interpreted the data and revised the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was reviewed by and received ethical approval from the Liverpool John Moores University Ethics Committee. All participants gave written informed consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lord, R.N., Adams, Z.H., George, K. et al. Exploratory assessment of right ventricular structure and function during prolonged endurance cycling exercise. Echo Res Pract 10, 22 (2023). https://doi.org/10.1186/s44156-023-00035-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44156-023-00035-8