Abstract
Background
Lung cancer remains the most common cause of cancer-related deaths in the USA. Successful implementation of lung cancer screening programs has led to increased detection of peripheral pulmonary lesions (PPL). Robotic-assisted bronchoscopy (RB) is a relatively novel tool used to safely diagnose PPN. Additionally, with the developing precision of personalized medicine and targeted therapy, obtaining adequate tissue for next-generation sequencing (NGS) has become critical to optimizing the medical management of lung cancer. Our aim is to assess the diagnostic yield of RB, identify patient and procedure characteristics associated with performing a diagnostic biopsy, and evaluate the adequacy of tumor cellularity for biomarker identification.
Results
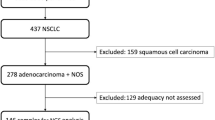
We performed a retrospective observational study consecutively enrolling 54 adult patients who underwent RB between January 2022 and March 2023. Records were reviewed for medical comorbidities and smoking status. PPL characteristics included size, location, presence of a bronchus sign on mapping computed tomography (CT) scans, distance from airway and pleura on CT, and days between obtaining CT and the bronchoscopy. Procedural factors included the radial endobronchial ultrasound (r-EBUS) view obtained and the sampling method(s) with which a diagnosis was achieved. Records were reviewed for final pathology and the need for further procedures to establish a diagnosis. Samples that yielded non-small cell lung cancer (NSCLC) were sent for an NGS panel if deemed adequate. The panels were reviewed to identify potentially actionable mutations. Multivariable logistic regression was performed to assess patients and lesions characteristics associated with a diagnostic biopsy. We sampled 56 lesions, 45 (80.4%) were from current or former smokers. The overall diagnostic yield was 73.2% and 68.9% for nodules less than 3 cm. Lesions size ranged from 8 mm nodules to 70 mm masses, with an average size 20.3 mm. Mean nodule size from diagnostic procedures was 21.5 mm and 16.9 mm from non-diagnostic ones (p = 0.04). Logistic regression analysis showed that the presence of a bronchus sign was associated with a diagnostic procedure (OR 19.4, p = 0.023), while lack of a r-EBUS view predicted a non-diagnostic bronchoscopy (OR 0.02, p = 0.013). 28 diagnostic biopsies (68.3%) yielded NSCLC and of the 25 cases that we followed, 22 samples (88%) were adequate for NGS.
Conclusions
The presence of a bronchus sign on CT and obtaining r-EBUS view during RB were associated with a higher diagnostic yield. RB successfully sampled PPL with adequate tumor cellularity for NGS.
Similar content being viewed by others
Background
Lung cancer is the most common cause of cancer-related death, responsible for more deaths in 2020 than breast, colorectal, and prostate cancers combined [1]. The five-year survival in lung cancer varies greatly based on the stage of the disease at diagnosis, with early detection being critical to reducing the mortality surrounding this disease [2]. The crux of early detection is robust screening with low-dose computed tomography (LDCT), which has demonstrated a 20% relative risk reduction in lung cancer mortality in high-risk current or former tobacco smokers [3]. As a result, there has been an increase in the performance of LDCT scans for lung cancer screening, resulting in the detection of many pulmonary lesions.
With an increase in nodules detected, tissue biopsy has become paramount to the timely diagnosis, staging, and genomic evaluation of lung cancers [4]. Further, targeted therapies have revolutionized the treatment of lung cancer, so that both diagnosis and adequate tumor cellularity for immunohistochemistry (IHC) and next-generation sequencing (NGS) are required [5]. Bronchoscopic biopsy is a preferred approach as it allows both staging via endobronchial ultrasound (EBUS) and diagnosis in a single procedure accompanied by a favorable safety profile [6]. Despite recent technological advances in peripheral bronchoscopy, the diagnostic yield of peripheral pulmonary lesion (PPL) biopsy remains highly variable [7]. Multiple studies have evaluated the diagnostic yield of the different bronchoscopic modalities, including some of the factors associated with impacting yield [8, 9].
Robotic-assisted bronchoscopy (RB) is a novel tool shown to be able to navigate to even the most peripheral portions of the lung while maintaining a good safety profile [10,11,12]. Multiple registry and retrospective studies have evaluated the diagnostic ‘yield’ of RB, which has shown promise in comparison to the standard of practice [13, 14]. However, these studies should be interpreted with caution given the lack of a uniformly accepted criteria for diagnosis, differences in pre-test probabilities for malignancy, and the conundrum of how to interpret a ‘non-diagnostic’ nodule or potential benign disease [15].
At the University of Illinois Hospital (UIH) in Chicago, IL, we care for a high-risk patient population that has a cancer rate more than twice that of the National Lung Screening Trial (NLST) [16]. Using the Ion RB platform, we collected prospective data on our first year of performing cases to continuously evaluate the performance of the technology. The aims of this study are to (1) identify factors associated with our diagnostic procedures compared to the non-diagnostic procedures and (2) evaluate RB adequacy for a commercial NGS panel to improve time to targeted therapy.
Methods
Patients
We enrolled consecutive patients referred for PPL evaluation and who underwent diagnostic RB in a new program at UIH between January 2022 and January 2023. The medical records of the patients were reviewed upon enrollment and retrospectively upon follow-up, to be included in the analysis. Institutional Review Board (IRB) approval was obtained from the University of Illinois at Chicago (protocol # 2022–0096).
Inclusion and exclusion criteria
We included patients who were aged 18 or older, were appropriate for elective RB under general anesthesia, and had one of the following presentations: pulmonary lesion(s) suspected to be primary lung cancer, known history of lung cancer now presenting with new or growing lung lesions requiring tissue diagnosis to confirm recurrence or progression of disease, known extrathoracic malignancy with pulmonary lesions requiring tissue diagnosis, or pulmonary lesions suspected of being due to mycobacterial or fungal infection and requiring tissue diagnosis prior to initiating antimicrobial therapies. Patients who were evaluated for PPL but did not undergo RB biopsies were excluded from the study.
Endpoints
-
➢ Primary endpoint–diagnostic yield
Procedures were considered diagnostic if the pathology revealed a final diagnosis, including confirmed malignancy or granuloma in the setting of the suspected infectious or inflammatory process; inflammatory tissue, fibrosis, and atypia were treated as non-diagnostic on initial biopsy. Non-diagnostic procedures did not reveal a final diagnosis. Patients with non-diagnostic procedures were considered for another diagnostic procedure (repeat bronchoscopy, CT-guided biopsy, or surgical biopsy) or CT surveillance per established guidelines [17].
-
➢ Secondary endpoints
-
◦ Patient characteristics: sex, age, body mass index (BMI), smoking status, history of thoracic or extrathoracic malignancy, American Society of Anesthesiologists (ASA) score [18], pulmonary function tests, and days since undergoing mapping CT scan before RB procedure.
-
◦ Lesion characteristics: size, location and lung centrality, distance from airway and pleura on mapping CT scan, airway generations traveled, radial endobronchial ultrasound (r-EBUS) view obtained, availability of rapid on-site evaluation (ROSE), and biopsy tool(s) with which diagnosis was achieved.
-
◦ NGS: Once a patient was diagnosed with non-small cell lung cancer (NSCLC), evaluation of adequate tumor cellularity for NGS panel and if an actionable mutation was identified.
-
◦ Complications: all adverse events related to the bronchoscopy and/or biopsy that occurred during the procedure or after its completion including pneumothorax (even if asymptomatic and/or did not require tube thoracostomy), clinically significant bleeding, and respiratory failure requiring ventilatory support beyond the planned general anesthesia.
-
Study design
Single-center, retrospective, observational.
Procedure
-
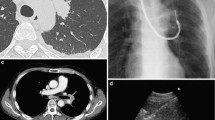
➢ Planning: patients underwent dedicated planning CT scans up to the day of their procedure. These are integrated into the Ion PlanPoint software, which creates a virtual airway tree and a pathway to the predetermined lung lesion, that is uploaded onto the robotic device.
-
➢ Procedure: all patients underwent general anesthesia and were mechanically ventilated via 8.0 mm (or bigger) endotracheal tube. Airways inspection and clearance were typically performed with a therapeutic bronchoscope (BF-1TH190; Olympus). All procedures were performed using the Ion endoluminal system (Intuitive Surgical, Sunnyvale, CA, USA) with a robotic catheter (3.5 mm outer diameter and a 2.0-mm working channel). The robotic catheter is designed to maintain the catheter position and correct unwanted tip deflection. A flexible peripheral needle (Flexision Biopsy needle; Intuitive Surgical, Sunnyvale, CA, USA) was used for needle aspiration, which was performed throughout the breathing cycle without a breath hold. Needles were available in 19, 21, and 23-gauge sizes. A r-EBUS probe (UM-S20-17s; Olympus) and a fluoroscopy C-arm (Artis zeego SW VD11C; Siemens, Inc.) were used to assist localization. Tissue biopsy was done with a 2.0-mm biopsy forceps.
-
➢ Specimen Collection and Processing: samples were obtained by transbronchial needle aspiration (TBNA) with a 19, 21, or 23-gauge needle and/or by transbronchial forceps biopsy (TBBx). For cases requiring ROSE by cytopathology staff, TBNA specimen from the first pass into the targeted lesion was used to prepare two smear slides. One slide was immediately placed in alcohol to preserve the specimen for definitive pap staining, and the second slide was air-dried for rapid Diff-Quik staining for real-time screening. Material remaining in the needle was rinsed into a labeled tube of formalin for cell block preparation. Screening was repeated if needed, at the discretion of the operator. Otherwise, the subsequent passes were all collected in formalin. For cases not requiring ROSE, all passes from a targeted lesion were rinsed into a labeled tube of formalin for cell block preparation. The number of passes per target was at the discretion of the bronchoscopist. TBBx specimens were placed directly into a formalin container for histopathology. Formalin-fixed paraffin-embedded (FFPE) blocks were made from the cell block and biopsy specimens, and H + E stained slides were then prepared for diagnostic evaluation. IHC was performed if needed to confirm a diagnosis of malignancy, subtype a malignancy, or determine the origin of the malignancy (i.e. primary vs metastatic).
-
➢ Next-generation sequencing: For all confirmed cases of NSCLC, Tempus xT genomic profiling was requested by the medical oncology service for the purpose of identifying targetable mutations. Programmed death-ligand 1 (PD-L1) testing by IHC was also requested to determine eligibility for immunotherapy. The Tempus xT is a tumor-targeted panel of 648 genes selected for actual or potential clinical relevance. PD-L1 IHC testing is an added option. For this study, specimens were considered ‘adequate’ for NGS if a full report was generated on the tumor tissue. Specimens were considered ‘inadequate’ if there was insufficient tissue to send, or if tissue was sent but was deemed insufficient for testing at Tempus. If the tumor from a patient in this study had one or more of these mutations, regardless of whether the approved targeted therapy was offered, that case was considered as having an actionable mutation.
Statistical analysis
Mean and standard deviations are reported for continuous variables; categorical variables are reported as percentage and counts. Welch’s t test or Mann–Whitney testing was used to compare the mean and median values of continuous variables as appropriate. Multivariable logistic regression was performed to assess patients’ and lesions’ characteristics associated with a diagnostic procedure. Two-tailed p-values of less than 0.05 indicated statistical significance for all comparisons. All statistical analysis was performed using Stata v14.2 (StatCorp, College Station, TX, USA).
Results
Baseline demographics
Fifty-four patients (56 lesions) were prospectively enrolled in the study. Demographic information is listed in Table 1. The mean age of the patients was 66.6 years old, 26 (46.4%) were female and the mean BMI was 26.3. Forty-five (80.3%) were current or former smokers and 11 (19.6%) were never smokers. Thirty-nine patients had an ASA score of 2 (69.6%).
Lesions
A total of 56 lesions were planned for peripheral biopsy with a median lesion size of 20.3mm, a minimum of 8mm, and a maximum of 70 mm and is represented in Table 2. Of the 56 lesions targeted, a diagnosis was achieved in 41 (73.2%), with 15 being non-diagnostic procedures. The mean lesion size in diagnostic procedures was 21.5 mm, non-diagnostic 16.9 mm (p value 0.04). Diagnoses at different lesion sizes are outlined in Table 3. The individual diagnoses are listed in Table 4. The majority of diagnoses were malignant (34/41; 82.9%) and the majority (28/34; 82.4%) were NSCLC. Sampling methods used to achieve diagnosis were TBNA (31/41; 75.6%), TBBx (35/41; 85.3%), and bronchoalveolar lavage (1/43; 2.3%). Tissue adequacy for TEMPUS-NGS in NSCLC was achieved in 22 out of 25 (88%) samples sent from peripheral bronchoscopy. Notably, 3 NSCLC cases that were diagnosed at UIH did not ultimately have NGS sent by our facility due to them following up with an oncologist outside our system. Of the 22 cases of NSCLC that were sufficient for NGS testing, 13 panels (59.1%) had an actionable mutation detected on the panel.
Statistical analysis
When further comparing characteristics of a diagnostic versus a non-diagnostic lesion, we evaluated multiple variables (sample mean diagnostic vs sample mean non-diagnostic; p value to detect the difference), and these are listed in Table 5. There were no significant differences between age (66.9 vs 65.9; 0.36), BMI (25.2 vs 29.1; 0.09), FEV1% predicted (80.8% vs 79.2%; 0.43), days from CT scan used for procedural planning until the procedure was performed (4.5 vs 8.6; 0.16), distance (mm) that the Ion Planpoint software predicted from the airway to the edge of the nodule (7.2 vs 8.6; 0.16), ROSE use in the procedure (29.3% vs 20%; 0.24) and an eccentric r-EBUS view (51.2% vs 46.7%; 0.385). However, we did see a significant difference in the following variables: bronchus sign present (56.1% vs 13.3%; 0.0005), number of airway generations traveled on planning software mapping (5.9 vs 6.6; 0.03), distance from the closest edge of the lesion to the pleura in mm (15.5 vs 8.5; 0.017), having a concentric r-EBUS view (46.3% vs 6.7%; 0.0002), and having no r-EBUS view (2.4% vs 46.7%; 0.003).
We subsequently took the variables having the most significant p values and did a logistic regression to determine what the most important factor(s) were in diagnosis, which is shown in Table 6. Lesion size (OR 0.9, 95% CI 0.85–1.03; p = 0.187) and having a concentric r-EBUS view (OR 8.1, 95% CI 0.66–100.5; p = 0.102) ultimately did not have an odds ratio that was significantly associated with a diagnostic procedure. However, the presence of a bronchus sign (OR 19.4, 95% CI 1.49–251.5; p = 0.023) and lack of r-EBUS view (OR 0.02; 95% CI 0.001–0.45; p = 0.021) were significant predictors on whether one would achieve a diagnosis.
In the evaluation of all 56 lesions, only three procedures (5.5%) were complicated by a pneumothorax post-RB. Of note, two of these still resulted in a diagnosis.
Discussion
Current clinical practice guidelines recommend guided bronchoscopy for the diagnosis of PPL when lung cancer is suspected [19]. As lung cancer screening programs expand and identify more pulmonary nodules requiring tissue sampling, the need for efficacious and safe diagnostic tools is critical [20]. The traditional yield of peripheral bronchoscopy has remained relatively stagnant for years, despite improvements in technology [13]. Enter RB in 2019, with early data suggesting excellent access to the peripheral lung [21] and improved diagnostic yield [8, 22, 23]. While early results suggest diagnostic yield may be improved with this technology, different models for defining diagnostic yields have been proposed [24]. Interpretation of diagnostic yield across multiple registry studies should be made with caution, as the different tools/technologies and definitions of ‘diagnostic biopsy’ are not standardized. The goal of this current study was to determine our success rate of not only obtaining a diagnosis but if malignant, assessing adequacy on a full NGS panel in order to provide oncologists with actionable results needed to treat their patient, from a single procedure.
This study primarily evaluated the diagnostic yield of a new RB program at a tertiary academic center. We believe this adds to the growing literature base on the efficacy of RB. We achieved a final diagnosis in 73.2% of all sampled lesions, which is comparable with the diagnostic yield (69.1–81.2%) to other established data [4, 8, 9, 21,22,23]. Of note, the yield was 68.9% in lung nodules smaller than 3 cm.
We obtained ‘atypical cells’ on four procedures, and controversy in the literature exists on whether this is a ‘diagnostic’ procedure. We did not consider atypia as diagnostic as oncologists cannot make treatment decisions with that pathologic finding. If we accepted atypia, our diagnostic yield would have increased from 73.2 to 80.4%. Again, this highlights the importance of determining a unified definition of ‘diagnostic yield’ to create uniformity of claimed results. The patients with atypia were either referred for another biopsy or will be followed clinically for nodule change. There was insufficient elapsed time to determine if some of the inflammatory or fibrotic tissue that were considered non-diagnostic were in fact determined benign with monitoring, which could have further increased diagnostic accuracy.
In the majority of the cases performed at UIH, both TBNA (various gauges) and TBBx (simple forceps) were used, and we saw increased efficacy with the forceps biopsy (85 vs 75%). This is similar to the established data but deviates a little from the AQuIRE registry which saw an increased yield with TBNA [13]. As obtaining adequate amounts of peripheral tissue becomes the standard by which we judge procedures, further study of peripheral bronchoscopy biopsies tools like forceps and transbronchial cryobiopsy will need to be undertaken.
Although diagnostic yield remains an important reportable statistic, we sought to evaluate the different patient and nodule characteristics associated with diagnostic outcomes, to better inform our colleagues and patients on what they can expect from their procedure. Consistent with the literature, having a bronchus sign was predictive of a diagnostic procedure in both univariate and multivariate analyses [8, 25]. Similarly, the ability to obtain a r-EBUS view appears to correlate with the likelihood of performing a diagnostic procedure. Following our logistic regression, the lack of a r-EBUS view was statistically significant with regard to non-diagnostic outcomes. Agrawal et al. showed different diagnostic accuracy correlating with the different types of r-EBUS views (absent had 38% while concentric and eccentric had 85% and 84%, respectively) [8]. Further, the size of the lesion appears to be significant, with our mean diagnostic lesion size being 4.6 mm larger than in non-diagnostic procedures. However, we were able to obtain a diagnosis in 67% of the nodules that were 10 mm and under, suggesting that there are other more important factors at play. This was suggested by our logistic regression, showing that r-EBUS view and bronchus sign are better predictors of success or lack thereof than simply the size of a lesion. There is a growing literature base that our study adds to, evaluating predictors of diagnostic outcomes, with nodule size, bronchus sign, and r-EBUS view consistently showing significance. Most of these data do not use tool-in-lesion confirmation with RB, so this is subject to scrutiny as those technologies become more prevalent. However, our data aids bronchoscopists as they select the appropriate diagnostic test.
Most of our diagnosed lesions were malignant, with the majority being NSCLC (82.3%), consistent with the knowledge that our population is at high risk for cancer [16]. Targeted therapies are substantially changing the management of lung cancers, with new drugs targeting driver mutations and various cancer-promoting molecules [5]. This personalized medicine approach has led to the improved survival of patients with NSCLC [26]. One of the aims of this study, and perhaps its most valuable contribution to the literature base, was to assess the RB adequacy in collecting samples not only for diagnosis but also for NGS and IHC for actionable mutations. Of the 25 NSCLC samples that were sent for NGS testing, 22 (88%) were adequate for full NGS testing, which is consistent with the only other study to have looked at this outcome [27]. Along with the study by Connolly et al., we sought to highlight the ability of RB to yield high tumor content from small PPL. It was also encouraging to see that of the NGS panels that were evaluated, over half of the samples discovered a potentially actionable mutation that can personalize those patients’ therapies and improve their outcomes.
We recognize the many significant limitations inherent to a single tertiary center model. First, our study has a small sample size that may skew some of our numbers. However using logistic regression, we believe we were able to mitigate some of the biases associated with a small sample size. Additionally, our patient population has a higher lung cancer rate than the national average and therefore a higher pretest probability for our RB to yield a malignant diagnosis [16], which may not be broadly applicable. Further, our lack of 2-year follow-up for the non-malignant lesions that yielded fibrotic changes or nonspecific inflammation were treated as non-diagnostic but may ultimately be benign. We also did not have access to some of the technologies that are being adopted for proof of tool-in-lesion (Cone-Beam CT, augmented fluoroscopy) so our results may not be representative of sites that do possess them. Further, these technologies may provide a way to overcome CT-to-body divergence (CTBD), which is a significant problem in synchronizing the patient in real-time with their pre-determined plan [28]. While our interventional pulmonologists are credentialed in RB, this is early data from a new program and only one bronchoscopist had performed a significant amount of cases prior to this study, which may also have impacted yields. Lastly, we do not consistently use ROSE at UIH due to various logistics limitations, and hence, no concrete conclusions can be drawn about it from this study.
Conclusion
As the literature around RB continues to expand and incorporate adjunct technology, we need well-designed studies comparing the different FDA-approved platforms currently available. It will be a focus of ours at UIH to design and perform well-structured multi-center trials in conjunction with the newly formed Interventional Pulmonary Outcomes Group (IPOG). In essence, RB likely does help with diagnostic yield, that obtaining adequate tissue for NGS is feasible, and that bronchus sign, r-EBUS view, and nodule size may all play a role in tissue acquisition. For patient impact, the combination of making a diagnosis, staging, and having adequate material for the determination of actionable mutations in a single procedure is most significant.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PPL:
-
Peripheral pulmonary lesion
- RB:
-
Robotic-assisted bronchoscopy
- NGS:
-
Next-generation sequencing
- CT:
-
Computed tomography
- LDCT:
-
Low dose computed tomography
- IHC:
-
Immunohistochemistry
- EBUS:
-
Endobronchial ultrasound
- r-EBUS:
-
Radial endobronchial ultrasound
- UIH:
-
University of Illinois Health
- NLST:
-
National Lung Screening Trial
- IRB:
-
Institutional Review Board
- BMI:
-
Body mass index
- ASA:
-
American Society of Anesthesiologists
- ROSE:
-
Rapid on-site evaluation
- FFPE:
-
Formalin-fixed paraffin embedded
- PD-L1:
-
Programed death ligand 1
- NSCLC:
-
Non-small cell lung cancer
- TBNA:
-
Transbronchial needle aspiration
- TBBx:
-
Transbronchial biopsy
- CTBD:
-
Computed tomography-to-body divergence
- IPOG:
-
Interventional pulmonary outcomes group
References
American Cancer Society (2023) Cancer facts and figures. Available at: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html
American Lung Association. Lung cancer fact sheet. Available at: https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancer-fact-sheet
National Lung Screening Trial Research Team, Aberle DR, Adams AM et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 365:395–409
Agrawal A, Hogarth DK, Murgu S (2020) Robotic bronchoscopy for pulmonary lesions: a review of existing technologies and clinical data. J Thorac Dis 12:3279–3286
Hirsch FR, Suda K, Wiens J, Bunn PA Jr (2016) New and emerging targeted treatments in advanced non-small-cell lung cancer. Lancet 388(10048):1012–1024
Callister MEJ, Baldwin DR, Akram AR on behalf of the British Thoracic Society Standards of Care Committe et al (2015) British Thoracic Society guidelines for the investigation and management of pulmonary nodules: accredited by NICE. Thorax. 70:ii1–ii54
Yarmus L, Akulian J, Wahidi M et al (2020) A prospective randomized comparative study of three guided bronchoscopic approaches for investigating pulmonary nodules: the PRECISION-1 study. Chest 157:694–701
Agrawal A, Ho E, Chaddha U et al (2022) Factors associated with diagnostic accuracy of robotic bronchoscopy with 12-month follow-up. Ann Thorac Surg S0003–4975(22):00042–X
Thiboutot J, Argento AC, Akulian J et al (2022) Accuracy of pulmonary nodule sampling using robotic assisted bronchoscopy with shape sensing, Fluoroscopy, and Radial Endobronchial Ultrasound (The ACCURACY Study). Respiration 101(5):485–493
Kumar A, Caceres JD, Vaithilingam S et al (2021) Robotic bronchoscopy for peripheral pulmonary lesion biopsy: evidence-based review of the two platforms. Diagnostics (Basel) 11:1479
Naaman R, Kapp C (2022) Innovations in bronchoscopy: robotic-assisted bronchoscopy. TouchREVIEWS Respir Pulm Dis 7(2):41–3
Chen A, Gillespie CT (2018) Robotic endoscopic airway challenge: REACH assessment. Ann Thorac Surg 106:293–297
Ost DE, Ernst A, Lei X et al (2016) AQuIRE bronchoscopy registry. Diagnostic yield and complications of bronchoscopy for peripheral lung lesions. Results of the AQuIRE registry. Am J Respir Crit Care Med. 193(1):68–77
Chen AC, Pastis NJ, Machuzak MS et al (2020) Accuracy of a robotic endoscopic system in cadaver models with simulated tumor targets: ACCESS study. Respiration 99(1):56–61
Vachani A, Maldonado F, Laxmanan B et al (2022) The impact of alternative approaches to diagnostic yield calculation in studies of bronchoscopy. Chest 161(5):1426–1428
Pasquinelli MM, Kovitz KL, Koshy M et al (2018) Outcomes from a minority-based lung cancer screening program vs the national lung screening trial. JAMA Oncol 4(9):1291–1293
MacMahon H, Naidich DP, Goo JM et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology 284(1):228–243
Doyle DJ, Hendrix JM, Garmon EH (2022) American Society of Anesthesiologists Classification. StatPearls. StatPearls Publishing, Treasure Island. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441940. [Updated 2022 Dec 4]
Rivera MP, Mehta AC, Wahidi MM (2013) Establishing the diagnosis of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143(5 Suppl):e142S-e165S
US Preventive Services Task Force (2021) Screening for lung cancer: US Preventive Services Task Force Recommendation Statement. JAMA 325(10):962–970
Chen AC, Pastis NJ Jr, Mahajan AK et al (2021) Robotic bronchoscopy for peripheral pulmonary lesions: a multicenter pilot and feasibility study (BENEFIT). Chest 159(2):845–852
Chaddha U, Kovacs SP, Manley C et al (2019) Robot-assisted bronchoscopy for pulmonary lesion diagnosis: results from the initial multicenter experience. BMC Pulm Med 19(1):243
Kalchiem-Dekel O, Connolly JG, Lin IH et al (2022) Shape-sensing robotic-assisted bronchoscopy in the diagnosis of pulmonary parenchymal lesions. Chest 161(2):572–582
Vachani A, Maldonado F, Laxmanan B et al (2022) The impact of alternative approaches to diagnostic yield calculation in studies of bronchoscopy. Chest 161(5):1426–1428
Seijo LM, de Torres JP, Lozano MD et al (2010) Diagnostic yield of electromagnetic navigation bronchoscopy is highly dependent on the presence of a Bronchus sign on CT imaging: results from a prospective study. Chest 138(6):1316–1321
Howlader N, Forjaz G, Mooradian MJ et al (2020) The effect of advances in lung-cancer treatment on population mortality. N Engl J Med 383(7):640–649
Connolly JG, Kalchiem-Dekel O, Tan KS et al (2022) Feasibility of shape-sensing robotic-assisted bronchoscopy for biomarker identification in patients with thoracic malignancies [published online ahead of print, 2022 Nov 25]. J Thorac Cardiovasc Surg S0022–5223(22):01258–2
Pritchett MA, Bhadra K, Calcutt M, Folch E (2020) Virtual or reality: divergence between preprocedural computed tomography scans and lung anatomy during guided bronchoscopy [published correction appears in J Thorac Dis. 2020 Aug;12(8):4593–4595. J Thorac Dis 12(4):1595–1611
Acknowledgements
Not applicable.
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Contributions
RN and CK were major contributors in collecting and analyzing data, as well as writing the manuscript. KH designed the study and performed many of the procedures studied. OD performed the histologic examination of the biopsy samples and contributed to writing the manuscript. BA and KK collected the data and contributed to writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The collection of human subjects data in this study was approved by the University of Illinois at Chicago (UIC) Institutional Review Board (IRB)–protocol # 2022–0096. All patients provided written consent to access their medical records.
All contributing authors underwent Ethics training within the Collaborative Institutional Training Initiative (CITI) program.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Naaman, R., Kapp, C.M., David, O. et al. Assessing the early returns of robotic-assisted bronchoscopy in a patient population at high risk for cancer: factors associated with a diagnostic procedure and pathologic outcomes. Egypt J Bronchol 17, 62 (2023). https://doi.org/10.1186/s43168-023-00238-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00238-x