Abstract
Background
Acute phase reactants (APR) are markers of inflammation that could be applied for the assessment of community-acquired pneumonia (CAP) severity in association with various pneumonia severity scores. So, the aim of the study was to assess levels of APR such as total leucocytic count (TLC), platelets, neutrophils, neutrophils-to-lymphocyte ratio (NLR), CRP, D-dimer, ferritin, and ESR in patients with CAP and to correlate between their values and disease severity.
Methodology
The study included 51 patients diagnosed as non-COVID-19 (CAP). Patients were classified into two groups group A (pneumonia only) and group B (pneumonia complicated with empyema/complicated para-pneumonic effusion). All patients underwent clinical evaluation, CURB65, radiological assessment, and blood sampling to measure APR.
Results
The mean age of patients was 47 ± 17 years. The main symptoms were productive cough (90.2%) and Fever (92.2%).TLC, platelets, neutrophils, CRP, D-dimer, ferritin, and ESR were elevated than normal values. Significant positive correlations were found between the duration of fever and CRP, D-dimer, and ferritin with p values = 0.024, 0.012, and 0.034 respectively. Significant positive correlations were found between CURB65 and both CRP and ferritin with p values = 0.007 and 0.020. A significant increase in platelet count and ESR values was found in group B than in group A.
Conclusion
APR are important markers that can be used in the assessment of CAP in collaboration with clinical evaluation and severity scores. CRP, D-dimer, and ferritin were positively correlated with CURB65, while ESR and platelets could be considered predictors of the development of complications.
Trial registration
Retrospectively registered, registration number NCT05926089, date of registration is 06/29/2023.
Similar content being viewed by others
Background
Community-acquired pneumonia (CAP) is the most prevalent respiratory infectious disease. It is defined as an acute infection of the lung parenchyma that is acquired outside the hospital [1, 2].
CAP is associated with increased morbidity and mortality, Especially in the elderly population, patients with chronic debilitating diseases, smoking, and alcohol consumption [3]
Acute phase reactants (APR) are inflammatory mediators that show significant alternations in serum levels in response to inflammation, these markers are responsible for some adverse effects such as anorexia, fever, fatigue, and anemia of chronic illness [4]. APR can be applied for the assessment of disease severity in CAP in collaboration with clinical evaluation and pneumonia severity scores [5].
The most common APR are leucocytic count, CRP, and ESR, changes in the level of these indices can be used in the diagnosis and prognosis of inflammatory and infectious diseases [6].
NLR is a rapid, simple, and cheap maker of the systemic inflammatory process, it is calculated as the ratio between neutrophil count to lymphocyte count from peripheral blood sample. Numerous researches have assessed the role of NLR in many infectious diseases such as sepsis, bacteremia, and septic shock, in addition, it can predict the severity and outcome of CAP [7].
So, the aim of the current study was to assess levels of APR such as total leucocytic count (TLC), platelets, neutrophils, neutrophils-to-lymphocyte ratio (NLR), CRP, D-dimer, Ferritin, and ESR in patients with CAP (as a primary outcome) and to correlate between their measured values and disease severity (as a secondary outcome).
Methodology
A cross-section prospective study was carried out in the Chest Department, Faculty of Medicine, Cairo University, during the period between October 2020 to April 2021. The research ethical committee at the Faculty of Medicine, Cairo University had approved the study (code: MS-358–2020) before patient enrollment.
The study included 51 patients diagnosed with non-COVID-19 community-acquired pneumonia (CAP). Diagnosis of CAP was considered if there were new radiological infiltrates in the presence of symptoms compatible with pneumonia (e.g., cough, sputum production, fever, dyspnea, and chest pain) [8].
Inclusion criteria
All patients above 18 years old, both sexes, fulfilling diagnosis of CAP with 2 PCR negative swabs for COVID-19 at least 1 day apart (based on Egyptian Ministry of Health recommendations).
Exclusion criteria
COVID-19 infection, non-pulmonary infections, HIV infection, recent pulmonary embolism, liver, renal, and cardiac diseases.
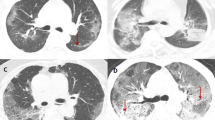
Data were collected from all patients with special emphasis on symptoms of pneumonia, risk factors (smoking, COPD, diabetes mellitus, and malignancy), clinical evaluation with assessment of disease severity using CURB-65 which is a score for triage decisions, length of stay, and risk stratification in cases of pneumonia. It gives one point for each of the following (confusion, urea > 7 mmol/L, respiratory rate ≥ 30 breaths/min, blood pressure < 90 mmHg (systolic) or ≤ 60 mmHg (diastolic), age ≥ 65 years). Score 0–1; suitable for home treatment, low mortality (1.5%), score 2; consider hospital treatment, intermediate mortality (9.2%) and score ≥ 3; assess the need for ICU admission, high mortality (22%) [9]. Chest X-ray and/or computed tomography (CT) of the chest was performed to confirm pneumonia diagnosis and to assess the site, number of the affected lobes, associated signs like cavitations, bronchiolar dilatation, site, and amount of pleural effusion if present. Multilobar pneumonia was defined as chest-radiograph infiltrates involving ≥ 2 lobes; bilateral when the involved lobes were in both the right and left lungs, and localized when only one pulmonary lobe was involved [10].
Aspiration of pleural fluid was performed in some cases, diagnosis of empyema was confirmed by the presence of frank pus or bacteria by gram stain or culture in the pleural fluid [11]. Complicated parapneumonic effusion was defined if there is a low glucose level, pleural fluid PH is below 7.20, and cultures from fluid are negative [12]. Patients were classified into two groups group A (pneumonia only) and group B (pneumonia complicated with empyema /complicated para-pneumonic effusion).
Sputum Gram stain and/or culture was not performed routinely in CAP cases managed at home, reserved for cases admitted to the hospital especially if classified as severe pneumonia or when MRSA or pseudomonas aeruginosa were suspected [8].
Venous blood samples for complete blood picture, differential leucocytic count, and platelets count which was done by the newly developed automated hematology analyzer XN (Sysmex, Kobe, Japan) enumerates and classifies blood cells by a combination of direct current detection and flow cytometry [13]. Normal value of total leucocytic count (TLC) is (4–7)103/μl. Normal neutrophils range is (2.5–7) 103/μl normal lymphocytes range is (1–4.8) 103/μl and normal platelets count is (150–450)103/μl [14]. The neutrophil-to-lymphocyte ratio (NLR) is easily obtained by dividing the absolute neutrophil count by the absolute lymphocyte count from peripheral complete blood counts. The normal range of NLR is in the range of 1–2 (0.8–2.2). The values above 3.0 and below 0.7 in adults are pathological [15]. C-reactive protein (CRP) is determined by photometric measurement of the latex agglutination reaction, the normal value of CRP is less than 6 mg/L [16]. D-dimer was done using Sysmex CS-5100 System is a fully automated, computer-interfaced coagulation analyzer intended for in vitro diagnostic use, and the normal value of D-dimer is less than 0.5 ng/ml [17]. Ferritin was performed using a standard auto-analyzer. Cobas c501 biochemistry human-driven ferritin shows agglutination with latex particles covered with anti-ferritin antibodies [18]. The normal value of ferritin is 10–291 ng/ml. Examination of erythrocyte sedimentation rate (ESR) was performed manually using the Westergren reference method. The normal value of ESR is the first-hour mm/h up to 10 and the second hour up to 20 [19]. All samples were taken within 24–48 h of the onset of the symptoms.
Statistical methods
Data were coded and entered using the statistical package for the Social Sciences (SPSS) version 28 (IBM Corp., Armonk, NY, USA). Data was summarized using mean, standard deviation, median, minimum, and maximum in quantitative data and using frequency (count) and relative frequency (percentage) for categorical data. Comparisons between quantitative variables were done using the non-parametric Mann–Whitney test [20]. For comparing categorical data, a chi-square (χ2) test was performed. An exact test was used instead when the expected frequency was less than 5 [21]. Correlations between quantitative variables were done using the Spearman correlation coefficient [22]. P values less than 0.05 were considered statistically significant.
Results
The current study was a cross-section prospective study that included 51 patients diagnosed with non-COVID-19 community-acquired pneumonia (CAP). The mean age of studied patients was 47 (SD ± 17) years, more than half of them were males (56.9%) and smokers (54.9%). About (45.1%) suffered from DM and (39.2%) were known COPD. The main presenting symptoms were productive cough (90.2%) and fever (92.2%) with a mean duration of fever of 4.67 (SD ± 4.38) days. Other symptoms included Dyspnea (39.2%) and Chest pain (43.1%). Forty-four (86.3%) of patients were admitted and managed at a hospital and 7 (13.7%) were treated in as outpatients setting. The mean values of TLC, platelets, neutrophils, CRP, D-dimer, Ferritin, and ESR were elevated than normal values in the studied patients. The range of NLR was (1.3–4.7) with a mean value 2.3 ± 0.72. Risk stratification of patients was done using CURB65 score (2.58 ± 0.9). The study group was classified into 2 groups; pneumonia only (Group A) included 33 patients (64.7%) and pneumonia + empyema or complicated para-penumonic effusion (group B) consisted of 18 patients (35.3%) (Tables 1 and 2).
The most common radiological findings were lobar consolidation (i.e., one lobe affected) in 42 patients (82.3%), bilateral consolidation and/or multi-lobar affection in 9 patients (17.7%), pleural effusion 18 patients (35.3%), cavitations and bronchiolar dilations in 4 (7.8%) and 2 (3.9%) patients respectively.
Significant positive correlations were found between the duration of fever and the following markers; CRP, D-dimer, and ferritin with p values = 0.024, 0.012, and 0.034 respectively (Table 3). Statistically significant positive correlations were found between CURB65 and both CRP and ferritin with p values = 0.007 and 0.020 as described in (Table 4).
Considering the age of patients, group B was significantly older than group A, P = 0.03 (Table 5). Moreover, DM was predominant in Group B, but with an insignificant p value = 0.06. However, other risk factors and sex had a non-significant impact between both groups.
ESR levels in the 1st, 2nd h, and platelets count were significantly higher in group B than in group A, P = 0.001, < 0.001, and 0.023 respectively. However, other markers did not show a significant difference between both groups (Table 5).
Discussion
Community-acquired pneumonia (CAP) is one of the most common disorders faced in clinical practice [1], and the most common cause of mortality among infectious diseases [3].
The present study included 51 patients diagnosed with non-COVID-19 community-acquired pneumonia, and the mean age of patients was 47 (SD ± 17) years, males represented (56.9%) of the study group, risk factors for pneumonia were smoking (54.9%), DM (45.1%), and COPD (39.2%).
It is well known that the incidence of pneumonia increases with age and the risk of CAP seems to be higher in males than females and in patients with chronic respiratory diseases, DM, smoking, alcohol consumption, and immune-compromising conditions [23,24,25].
In the current study, the chief complaints were productive cough (90.2%) and fever (92.2%) with a mean duration of fever of 4.67 (SD ± 4.38) days. This was matched with previous studies in which the mean fever duration was 5.5 ± 1.1 days and productive cough among pneumonia cases ranged from 86 to 100% [26, 27].
Acute inflammatory response triggered by infection of the lower respiratory tract as in pneumonia is considered a complex interaction between the immune system and inflammatory cytokines in order to regulate the inflammatory process [28].
APR are biomarkers of inflammation, their levels show significant changes during active inflammation. They are categorized as positive or negative based on their serum level during the inflammatory process [29].
The present study reported an increase in the mean values of TLC, platelets, and neutrophils than normal values, with an NLR range was 1.3–4.7 and a mean value of 2.3 ± 0.72.
This was matched with previous studies that reported elevated TLC and neutrophils in CAP and emphasized their role in diagnosis and follow-up of treatment response [30, 31].
NLR is a useful and simple marker, one study demonstrated that NLR can perform better than conventional biomarkers in the assessment of severity and predicting mortality in elderly patients with CAP [32], these findings were not matched with our results this may be related to differences in the age, co-morbid diseases and number of enrolled patients in their study.
On the other hand, another study confirmed that NLR is not analogous to traditional biomarkers such as CRP and procalcitonin in the diagnosis and evaluation of the severity of pneumonia [33] which is matched with our findings.
Recent meta-analysis concluded that NLR is a promising marker in predicting the prognosis of pneumonia either alone or in a combination of other biomarkers or scoring systems; however, further studies are needed to confirm these findings [34].
Platelets are crucial inflammatory cells that release a lot of inflammatory mediators in response to infection hence considered as acute phase reactant. It has been reported that changes in platelet count might be used as diagnostic and prognostic markers of various inflammatory disorders [35].
Although little is known about the role of platelets in CAP, a previous study reported that changes in platelets may be considered a better marker than leucocytic abnormalities in children with pneumonia [6].
In our study, platelet count was significantly higher in pneumonia cases complicated with empyema/para-pneumonic effusion (group B) than in group A, p value = 0.023 (Table 5). This was consistence with another study that described the role of platelet count as a predictor of CAP complications [36].
We found that mean values of CRP, D-dimer, and ferritin were elevated in the study population than normal values. Positive significant correlations were found between the duration of fever and the following markers; CRP, D-dimer, and ferritin with p values = 0.024, 0.012, and 0.034 respectively, when correlating pneumonia severity using CURB65 with APR, positive significant correlation was noticed between CURB65 and both CRP and ferritin only with p values = 0.007 and 0.020.
CRP is one of the positive acute-phase proteins produced by hepatocytes in response to infection or inflammation [37].
Previous studies described elevated CRP in pneumonia and found a proportional relation between its level and pneumonia severity as assessed by the APACHE II scores [33, 38].
D-dimer is a product of fibrin degradation by plasmin, high levels of D-dimer were observed in conditions associated with fibrin synthesis and catabolism such as deep venous thrombosis (DVT), pulmonary embolism (PE), post-operative state, trauma, severe infections and disseminated intravascular coagulopathy (DIC) [39]. Previous studies have suggested that elevated levels of D-dimer in CAP are directly related to intra- and extra-vascular coagulation triggered by acute damage of lung parenchyma during the infectious process [40].
Some studies reported a positive correlation between D-dimer level and pneumonia severity using the pneumonia severity index (PSI) and the extent of radiological involvement [41, 42]. In the current study, we assessed pneumonia severity using the CURB65 score but it was not significantly correlated to D-dimer.
Ferritin is a protein produced by liver cells, kupffer cells, and macrophages, it is considered one of the acute phase reactant as its level increases in response to infectious and various inflammatory conditions [43].
One study reported a marked elevation of ferritin concentration in 10% of CAP patients admitted to the ICU [43]. Another one found higher levels of ferritin in patients with CAP who developed sepsis [44] suggesting that higher ferritin levels may be associated with pneumonia severity which is matched with our results.
ESR is a non-specific inflammatory marker, any condition that affects red blood cells or fibrinogen levels can affect ESR values.
It was found that ESR was elevated than normal values in the study population and levels in the 1st and 2nd h were significantly higher in group B than group A, P = 0.001 and < 0.001 respectively. So, we can assume that elevated ESR may be used as a predictor of complications in CAP but further studies on larger populations are needed.
Our results were matched with previous research which reported high ESR values in CAP [27, 32].
Another study found significantly high values of ESR in young children with lobar pneumonia, but it confirmed that procalcitonin can perform better than ESR in the prediction of CAP in children [45].
Limitations
This study has several limitations:
-
(1) Single-center study with small numbers of patients.
-
2) We did not exclude patients on prior use of antibiotics, this may affect the level of APR.
-
3) Follow-up levels of APR and assessment of the response to treatment were not included in the study.
-
4) We did not correlate between APR and mortality.
Conclusions
In patients with non-COVID-19 community-acquired pneumonia markers such as TLC, neutrophils, platelets, CRP, D-dimer, ferritin, and ESR were elevated than normal reference values. Significant positive correlations were found between the duration of fever and CRP, D-dimer, and ferritin. Assessment of pneumonia severity was done using CURB65 score which was positively correlated with CRP and ferritin. It was found that Platelets and ESR values were significantly elevated in the CAP group complicated with empyema or complicated para-pneumonic effusion assuming that both markers could be used as predictors of complications in CAP; however, further researches are needed to emphasize or decline this assumption.
Availability of data and materials
Data from the current study are available from the corresponding author upon re upon reasonable request.
Abbreviations
- APR:
-
Acute phase reactant
- CAP:
-
Community-acquired pneumonia
- COVID-19:
-
Coronavirus infection of 2019
- CURB65:
-
Confusion, urea, respiratory rate, blood pressure, and age above 65
- NLR:
-
Neutrophils-to-lymphocyte ratio
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- PCR:
-
Polymerase chain reaction
- HIV:
-
Human immune deficiency virus
- ICU:
-
Intensive care unit
- CT:
-
Computed tomography
- DM:
-
Diabetes mellitus
- COPD:
-
Chronic obstructive pulmonary disease
- APACHE:
-
Acute physiology and chronic health evaluation
- DVT:
-
Deep venous thrombosis
- PE:
-
Pulmonary embolism
- DIC:
-
Disseminated intravascular coagulation
- PSI:
-
Pneumonia severity index
References
Musher DM, Thorner AR (2014) Community-acquired pneumonia. N Engl J Med 371:1619
Murdoch DR, Howie SRJ (2018) The global burden of lower respiratory infections: making progress, but we need to do better. Lancet Infect Dis 18:1162–1163
Ramirez JA, Wiemken TL, Peyrani P et al (2017) Adults Hospitalized With Pneumonia in the United States: Incidence, Epidemiology, and Mortality. Clin Infect Dis 65:1806
Gruys E, Toussaint MJ, Niewold TA, Koopmans SJ (2005) Acute phase reaction and acute phase proteins. J Zhejiang Univ Sci B 6(11):1045–1056
Kruger S, Welte T (2012) Biomarkers in community-acquired pneumonia. Expert Rev Respir Med 6:203–214
Sabina Janciauskiene, Tobias Welte, Ravi Mahadeva. Acute phase proteins: structure and function relationship. In: Acute Phase Proteins – Regulationand Functions of Acute Phase Proteins. 2011. p. 25–60. https://doi.org/10.5772/18121.
de Jager CP, Wever PC, Gemen EF, Kusters R, van Gageldonk-Lafeber AB, van der Poll T, Laheij RJ (2012) The neutrophil-lymphocyte count ratio in patients with community-acquired pneumonia. PLoS One. 7(10):e46561
Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K ,et al., Diagnosis and treatment of adults with community-acquired pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-e67. https://doi.org/10.1164/rccm.201908-1581ST. PMID: 31573350; PMCID: PMC6812437.
Lim WS, van der Eerden MM, Laing R et al (2003) Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 58:377–382
Liapikou A, Cillóniz C, Gabarrús A, Amaro R, De la Bellacasa JP, Mensa J, Sánchez M, Niederman M, Torres A (2016) Multilobar bilateral and unilateral chest radiograph involvement: implications for prognosis in hospitalised community-acquired pneumonia. Eur Respir J 48(1):257–261. https://doi.org/10.1183/13993003.00191-2016. (Epub 2016 Apr 21 PMID: 27103390)
Corcoran JP, Wrightson JM, Belcher E, De Camp MM, Feller-Kopman D, Rahman NM (2015) Pleural infection: past, present, and future directions. Lancet Respir Med. 3:563e77
Light RW (2006) Parapneumonic effusions and empyema. Proc Am Thorac Soc 3(1):75–80
Daves M, Zagler EM, Cemin R et al (2015) Sample stability for complete blood cell count using the Sysmex XN haematological analyser. Blood Transfus 13(4):576
Tanaka Y, Tanaka Y, Gondo K et al (2014) Performance evaluation of platelet counting by novel fluorescent dye staining in the XN-series automated hematology analyzers. J Clin Lab Anal 28:341–348
Holub M, Beran O, Kaspříková N, Chalupa P (2012) Neutrophil to lymphocyte count ratio as a biomarker of bacterial infections Central. Eur J Med 7(2):258
Scharnhorst V, Noordzij PG, Lutz A et al (2019) A multicenter evaluation of a point of care CRP. TEST 71:38–45
Flieder T, Gripp T, Knabbe C et al (2016) The Sysmex CS-5100 coagulation analyzer offers comparable analytical performance and excellent throughput capabilities. Pract Lab Med 6:38–47
Ayan D, Soylemez S (2020) Measuring plasma ferritin levels with two different methods: a comparison of Roche Cobas e601 versus Roche Cobas c501 (integrated modular system Roche Cobas 6000). Journal of medical biochemistry 39(1):13
Dewi MMW, Herawati S, Mulyantari NK et al (2019) The comparison of erythrocyte sedimentation rate (ESR) modify Westergren Caretium Xc-A30 and Westergren Manual in Clinical Pathology Laboratory. Sanglah General Hospital, Denpasar, Bali 8:396–399
Chan YH (2003) Biostatistics102: Quantitative Data – Parametric & Non-parametric Tests. Singapore Med J 44(8):391–396
Chan YH (2003) Biostatistics 103: Qualitative data –tests of independence. Singapore Med J 44(10):498–503
Chan YH (2003) Biostatistics 104: correlational analysis. Singapore Med J 44(12):614–619
Almirall J, Bolíbar I, Balanzó X, González CA (1999) Risk factors for community-acquired pneumonia in adults: a population-based case-control study. Eur Respir J 13:349
-Torres A, Peetermans WE, Viegi G, et al. Risk factors for community-acquired pneumonia in adults in Europe: a literaturereview. Thorax 2013; 68: 1057e65. Available at: https://thorax.bmj.com/content/68/11/1057
Bello S, Menéndez R, Antoni T et al (2014) Tobacco smoking increases the risk for death from pneumococcal pneumonia. Chest 146:1029
Tao LL, Hu BJ, He LX, Wei L, Xie HM, Wang BQ, Li HY, Chen XH, Zhou CM, Deng WW (2012) Etiology and antimicrobial resistance of community-acquired pneumonia in adult patients in China. Chin Med J (Engl) 125(17):2967–2972 (PMID: 22932165)
- Alfeky, H., sedky, M., Soliman, A. Comparison between acute phase reactant in COVID-19 pneumonia and bacterial pneumonia. Al-Azhar International Medical Journal, 2022; 3(11): 125–129. https://doi.org/10.21608/aimj.2022.141638.1960.
Yormaz B, Ergun D, Tulek B, Ergun R, Korez KM, Suerdem M (2020) The evaluation of prognostic value of acute phase reactants in the COVID-19. Bratisl Lek Listy. 121:628–33
Gulhar R, Ashraf MA, Jialal I (2018) Physiology, acute phase reactants.
Ning J, Sha X, Ma Y, Lv D (2016) Valuable hematological indicator for the diagnosis and severity assessment of Chinese children with communityaccquiredpneumonia prealbumin. Medicine 95(47):e5452
Motamed H, Bashiri H, Yari F, Bozorgomid A, Rostamian M, Azarakhsh Y et al (2021) Association between community-acquired pneumonia and platelet indices: A case-control study. J Acute Dis 10(1):23–27
Cataudella E, Giraffa CM, Di Marca S et al (2017) Neutrophil -to- lymphocyte ratio: an emerging marker predicting prognosis in elderly adults with community-acquired pneumonia. J Am Geriatr Soc 65(8):1796–1801
Zheng N, Zhu D, Han Y (2020) Procalcitonin and C-reactive protein perform better than the neutrophil/lymphocyte count ratio in evaluating hospital acquired pneumonia. BMC Pulm Med 20(1):166. https://doi.org/10.1186/s12890-020-01207-6.PMID:32527243;PMCID:PMC7289235
Kuikel S, Pathak N, Poudel S et al (2022) Neutrophil–lymphocyte ratio as a predictor of adverse outcome in patients with community-acquired pneumonia: a systematic review. Health Sci Rep 5:e630. https://doi.org/10.1002/hsr2.630
Cros A, Ollivier V, Ho-Tin-Noe B (2015) Platelets in inflammation: regulation of leukocyte activities and vascular repair. Front Immunol 5:678
Sahin M, Duru NS, Elevli M, Civilibal M (2017) Assessment of platelet parameters in children with pneumonia. J Pediatr Infect 11(3):e106–e112
Kazerani M, Moghadamnia F (2016) Survey of relationship between platelet count and complications community acquired pneumonia in teaching hospitals of Mashhad Islamic Azad University (2014). Med J Mashhad Uni Med Sci 59(5):300–308
Liu GB, Cui XQ, Wang ZB, Wen L, Duan HL (2018) Detection of serum procalcitonin and hypersensitive C-reactive protein in patients with pneumonia and sepsis. J Biol Regul Homeost Agents 32(5):1165–9
Freyburger G, Trillaud H, Labrouche S, Gauther P, Javorschi S, Bernard P et al (1998) D-dimer strategy in thrombosis exclusion–a gold standard study in 100 patients suspected of deep venous thrombosis or pulmonary embolism: 8 DD methods compared. Thromb Haemost 79:32–37
Günther A, Mosavi P, Heinemann S, Ruppert C, Muth H, Markart P (2000) Alveolar fibrin formation caused by enhanced procoagulant and depressed fibrinolytic capacities in severe pneumonia. Am J Respir Crit Care Med 161:454–462
Shilon Y, Shitrit ABG, Rudensky B, Yınnon M, Margalit M, Sulkes J et al (2003) A rapid quantitative D-dimer assay at admission correlates with the severity of community acquired pneumonia. Blood Coag Fibrinol 14:745–748
Arslan S, Ugurlu S, Bulut G, Akkurt I (2010) The association between plasma d-dimer levels and community-acquired pneumonia. Clinics 65(6):593–597
Brands X, de Vries FMC, Uhel F et al (2021) Plasma ferritin as marker of macrophage activation-like syndrome in critically ill patients with community-acquired pneumonia. Crit Care Med 49:1901–1911
Brands X, van Engelen TSR, de Vries FMC, Haak BW, Klarenbeek AM, Kanglie MMNP et al (2022) Association of hyperferritinemia with distinct host response aberrations in patients with community-acquired pneumonia. J Infect Dis 225(11):2023–2032. https://doi.org/10.1093/infdis/jiac013. (PMID:35100411;PMCID:PMC9312861)
Markanday A. Acute Phase Reactants in Infections: Evidence-Based Review and a Guide for Clinicians. Open Forum Infect Dis. 2015;2(3):ofv098. https://doi.org/10.1093/ofid/ofv098.
Acknowledgements
Not applicable.
Funding
No.
Author information
Authors and Affiliations
Contributions
Yosri Akl was responsible for the acquisition of data, analysis, drafting of the article, and final approval. Ahmed Elkomy was responsible for the acquisition of data, analysis, drafting of the article, and final approval. Eman Kamal Ibrahim was responsible for the conception and design, revising, writing, and final approval of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried in accordance with relevant regulations and guidelines, informed consent was obtained from all participants and/or their legal guardians, and the study was approved by the research ethical committee, Cairo University with code (MS-358–2020).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akl, Y., Elkomy, A. & Ibrahim, E.K. Acute phase reactants in non-COVID-19 community-acquired pneumonia. Egypt J Bronchol 17, 57 (2023). https://doi.org/10.1186/s43168-023-00234-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00234-1