Abstract
Extracorporeal membrane oxygenation (ECMO) is an adapted form of the heart–lung machine that provides cardiopulmonary bypass life support for critically ill patients with acute cardiac and/or respiratory failure who are unresponsive to standard medical and surgical therapies. Although ECMO therapy has advanced significantly, complications like thrombosis and bleeding continue to be substantial, necessitating rapid transport of patients to the radiology suite to reveal crucial findings for further treatment plans or care. Even though the low flow rate for veno-arterial ECMO (VA-ECMO) support during contrast-enhanced CT is well known, the flow rate for veno-venous ECMO support during CT, especially computed tomography pulmonary angiography, is not well understood. Our case emphasizes that CTPA can be performed safely in trauma patients with ECMO runs and any suspected complications during ECMO runs may delay or worsen the clinical prognosis therefore immediate radiological verdicts may reveal significant findings to plan the treatment accordingly. Also, there were no complications associated with our examinations or transport. Our case highlights that VV-ECMO like VA-ECMO induces flow-dependent alterations in the patient’s circulation due to contrast injections, which might lead to an incorrect interpretation of CTPA. However, CTPA is safe, and bringing down the VV-ECMO flow rate of zero with vigilant monitoring of vitals and ventilation support helps radiologists to predict and interpret the contrast flow based on injection and cannula sites in the diagnosing and evaluation of pulmonary embolism patients with acute respiratory failure during ECMO.
Similar content being viewed by others
Introduction
Polytrauma is the most common fatality in Saudi Arabia, accounting for 80 to 85% of all traumas [1] and statistically the leading cause of adult trauma mortality in the USA and globally [2]. Polytrauma injuries can often be more severe, with a higher mortality of 18.7%, frequent ICU admissions, and extended hospital and ICU stay. Early mortality after trauma is caused mainly by traumatic brain damage and hemorrhage. On the other hand, late fatalities are primarily the result of multisystem failure, respiratory failure, and acute respiratory distress syndrome (ARDS) [3, 4]. ARDS affects 10 to 15% of patients hospitalized in intensive care units and up to 23% of mechanically ventilated patients. Several previous works of the literature concluded ARDS mortality rate was 43%. However, the mortality rate of ARDS increases based on disease severity such as mild (27%), moderate (32%), and severe (45%) illness, respectively [5]. Throughout the previous two decades, medical advances have increased the survival rate of ARDS patients. The ARDS net trial study in the year 2000 with lower tidal volumes and PEEP titration scales found that lower tidal volumes and PEEP titration scales reduced mortality relative to traditional mechanically ventilated high-tidal volume [6]. Current research indicates that neuromuscular inhibition and prone improve mortality in ARDS patients. Inhaled prostacyclin and other hybrid kinds of ventilation, such as bilevel ventilation, are also available as supplements. Despite these breakthroughs in rescue medicines, some patients continue to decline and require venovenous extracorporeal membrane oxygenation (VV ECMO) as salvage therapy [7]. In this clinical context, individuals who survive the first 24 h following trauma are at significant risk of developing pulmonary embolisms (P.E.), the third leading cause of mortality. Furthermore, post-traumatic pulmonary embolism typically occurs at least 5 days after trauma, particularly in patients with lower limb or pelvic fractures with a higher embolic risk, similar to severe head or spine traumas [8, 9]. Trauma patients are also exposed to additional risk factors such as sepsis, vasopressor use, pharmacologic sedation, mechanical ventilation, central venous catheters, renal failure, and ECMO [10]. Imaging in polytrauma patients is crucially important for providing critical clinical care. Unfortunately, CT scanning is designated for clinical settings that are relatively sophisticated and difficult. However, computer tomography pulmonary angiography (CTPA) has replaced the ventilation-perfusion scan and traditional invasive pulmonary angiography as the gold standard for diagnosing P.E. in ICU patients [11]. Despite the challenge of interpreting P.E., its literature on the use of CT in patients on ECMO is limited. To our knowledge, there is a paucity of complete published information addressing the indications, procedure, safety, and efficacy of IHT on patients supported with ECMO. This case report discusses the challenges, potential benefits, safety measures, and techniques for obtaining the best CT images to diagnose P.E. and eliminate the fear of intra-hospital transfer in post-traumatic patients who may require a diagnostic procedure to confirm P.E. in the CT room. Any such delay may hinder optimal patient management and result in a disastrous outcome. In addition, this report details the severe dangers associated with transporting critically sick patients who are on mechanical ventilators and ECMO support with multiple cannulas implanted in major blood veins, as well as several infusion pumps requiring multiple extended tubings.
Case report
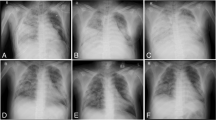
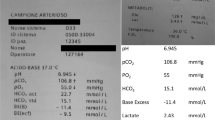
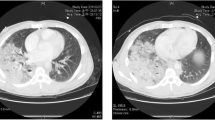
A 31-year-old male patient, a medically free polytrauma victim, arrived at our institute. Our emergency physicians’ primary trauma survey revealed left-side hemopneumothorax clinically, and to relieve severe respiratory distress, a left intercostal drainage tube (Fig. 1) was inserted as a life-saving measure. Following secondary trauma surveys, computer tomography (CT) showed free abdomen and brain injuries associated with life-threatening chest trauma with bilateral pulmonary contusions, multiple left-side rib fractures, left-side hemopneumothorax, and bilateral humerus fractures. A few hours after arrival, the patient was intubated electively due to severe hypoxemia, and arterial blood gas analysis shows Ph: 7.34, pco2: 34, pao2: 63, and Hco3:17. Despite the protective lung ventilation strategy, his oxygen and PEEP requirements rose. On his third day after admission to the ICU, the CXR revealed significant bilateral infiltration attributable to lung contusions. His FiO2 requirement was 1.0, with a PEEP of 12 and a tidal volume of 450 ml. The Bedside echocardiography evaluation showed normal left and right ventricular size and function, with no indications of any cardiac dysfunction. However, there were no signs of improvement from severe hypoxia, and ABG shows PH:7.20 pco2:56, pao2: 45, and Hco3: 21. Therefore, the intensive care team decided to initiate ECMO service to the patient, uneventful venovenous cannulation of the right femoral vein and right internal jugular vein with drainage cannula of 25 Fr, 55 cm, and return cannula of 21 Fr, 18 cm inserted. Once after cannulation, the ultraprotective lung ventilation with the following parameters: FiO2 = 0.4, PEEP = 8, T.V. = 250 mL, and respiratory rate = 10/min started. The VV-ECMO flow rate was 4–4.5 L/min. Hence, orthopedics team determined that he was not suitable for definitive fixation of bilateral humerus fractures (Fig. 2). In addition, the patient experienced continuous paroxysmal atrial fibrillation, for which precise tests were done, which included bedside echocardiography, but no evident cause was ruled out. Although our institute is a central hospital that has been providing ECMO service for the last 5 years, we do not have experience performing CT pulmonary angiography on VV-ECMO patients. However, our team chose CT pulmonary angiography as the best procedure to rule out pulmonary embolism. We shifted the patient to the radiology suite with all precautionary measures with experienced team members. Nevertheless, we faced challenges in such a radiologic investigation since there are no established protocols for doing an angiographic test in ECMO-supported patients. Although the contrast was injected via the left forearm 18 G peripheral cannula, no contrast was noticed in the pulmonary angiography. Therefore, we decided to try again by maximizing the ventilator settings to FiO2 1.0 Peep 15, RR. 25, VT 450 after lowering the ECMO flow to 1 L/min. Once the patient’s vitals and oxygenation were satisfactory, the contrast was injected again via the left forearm 18 G peripheral cannula resulting in a faint opacification of the pulmonary artery. Then, we decided to keep the ECMO flow at zero with the same maximal ventilator settings. Not to forget that during the ECMO, the patient was on continuous heparin infusion utilizing the recommended ELSO guidelines, keeping the APTT ratio between 1.5 and 2 times the reference level. Once the radiology technician was ready, we stopped the ECMO flow, and the contrast study was completed satisfactorily, with good opacification of the pulmonary arteries, confirming the pulmonary embolism (Fig. 3a, b). The patient was stable, and no complications developed and was shifted to the ICU. Pulmonary embolism was managed and treated successfully by continuous heparin infusion following the same protocol suggested by ELSO, but we increased the APTT target to be 2–2.5 times the reference range, followed by rivaroxaban (anticoagulants). On the 7th day, the patient was mobilized to the OR for bilateral fixation of the humerus, and on the 10th day, gradual weaning and discontinued ECMO safely with uneventful complications. The patient was discharged home by walking on the 25th day following intensive rehabilitation.
Discussion
Post-traumatic PE is a life-threatening complication following trauma with an overall prevalence of 18% and this post-traumatic PE can significantly enhance the possibility of venous thromboembolism (VTE) incidents [8]. Our case supports the notion that early CTPA diagnosis and management of posttraumatic PE in ECMO patients result in favorable outcomes. Generally, PEs have been presumed to occur most frequently between days 5 and 7 following a traumatic injury that supports the theory that post-traumatic PE is caused by deep venous thrombosis of the lower limbs and pelvis [12]. In our case, PE happened on the fifth day. ECMO is most well-known for its use in neonatal respiratory failure; To date, the use of ECMO has been also well-recognized in adult respiratory failure patients. The CESAR (conventional ventilatory support versus ECMO for severe adult respiratory failure) 2009 trial is the only multi-center, randomized, controlled trial to investigate the use of modern VV ECMO techniques in adult patients with respiratory failure. It shows a better survival and quality-adjusted life outcome in adult patients with severe respiratory failure referred for ECMO compared to conventional treatment [13]. However, since the first description of ARDS by Asbaugh et al. in 1967 and following 5 decades of extensive research on ARDS pathogenesis has expanded a little bit of its clinical knowledge and management. In a recent international study involving 29,144 patients, 10% of all patients admitted to the intensive care unit (ICU) and 23% of mechanically ventilated patients had ARDS. Mortality in the subgroup of patients with severe ARDS was 46% without ECMO [14]. Friedrichson reports a significant decline in in-hospital mortality rates for patients with acute respiratory distress syndrome (ARDS) who underwent venovenous extracorporeal membrane oxygenation (VV ECMO) treatment. The mortality rate decreased from 70.4% in 2007 to 53.9% in 2018 [15]. Acute respiratory distress syndrome (ARDS) is a recognized complication of major trauma, with a prevalence ranging from 8 to 82% of selected patients. These selected populations include patients with pulmonary contusions, severe trauma (Injury Severity Score, > 25), head injury, notable base deficit, notable blood transfusion requirement, and notable orthopedic injuries such as long bone and pelvic fractures. The presence of ARDS is associated with a significant increase in morbidity, increased use of hospital resources, and a 4.3-fold increase in mortality [16, 17]. Most centers associate ECMO with conventional treatment as a last-rescue therapy in ARDS. In this context, studying the disease progress or identifying any complications during ECMO running requires frequent imaging studies. Imaging ECMO patients most commonly involves portable chest radiography, bedside ultrasound, and CT. Generally, on a chest radiograph, a diffuse opacification of the lung fields develops soon after the initiation of ECMO. This diffuse opacification phenomenon can cause unclear soft-tissue landmarks, making it difficult to assess disease progression, ECMO cannula, ET tube, and other line positions [18]. Literature on the use of CT in patients with ECMO is limited, in particular CT PA. Therefore contrast-enhanced CT imaging of ECMO patients poses unique technical and diagnostic challenges. Several factors must be considered to ensure that contrast-enhanced CT scans on ECMO patients are effective and safe. The type of ECMO employed, the examination required, and the patient’s stability all contribute to the investigation’s challenges. Transfer times from the ward to CT and return can take up to 80 min due to the complexities of the logistics and examinations. Lee et al. proposed ways to improve CT pulmonary angiography for VA ECMO patients. Prior to administering intravenous contrast, the ECMO flow rate is 500 ml/min for 15 to 25 s, and the bolus-tracking ROI is positioned above the main pulmonary artery [19, 20]. Despite the fact that these concepts have not been studied as effective techniques in VV-ECMO CT pulmonary angiography, Lidegran et al. developed three novel procedures for reducing flow-related CT artifacts in VA ECMO. (1) Injecting contrast into the arterial cannula following the membrane oxygenator. However, there is a high risk of air embolism, which can result in ischemic stroke: (2) reducing pump flow after the contrast injection also helps decrease artifacts and (3) delaying the CT scan time after the contrast induction to accommodate for the varying densities [21]. To our knowledge, there is no definitive protocol for contrast-enhanced CTPA for VV-ECMO patients. Although Liu KL et al. stated that patients on VV-ECMO typically have respiratory failure with normal cardiac function, contrast-enhanced CT imaging is similar to non-ECMO patients, and any filling defects or dissection flaps in the thoracic aorta will be associated with the true aortic syndrome [22]. However, studies on CTPA in VV-ECMO patients are scarce. Our report emphasizes that once the patient’s vitals and oxygenation were satisfactory in the CT room suite, decrease the ECMO flow to 0 L/min and maximize the mechanical ventilator settings. A short drop in ECMO flow for seconds will not increase the risk of circuit clotting especially if the patient was on target therapeutic heparin infusion. Once the radiology technician was ready, inject the contrast via a large-bore peripheral cannula, and the study was completed satisfactorily, with good opacification of the pulmonary arteries within 80 s, confirming the pulmonary embolism.
Conclusion
CT pulmonary angiography can be done while patients are on VV-ECMO, but physicians need to be aware of the appropriate process and be prepared in case of unexpected complications.
Availability of data and materials
The data analyzed during the current study are available from the corresponding author upon request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- PE:
-
Pulmonary embolism
- VV-ECMO:
-
Veno-veno extracorporeal membrane oxygenation
- CTPA:
-
Computed tomography pulmonary angiogram
- ICU:
-
Intensive care unit
- PEEP:
-
Positive end-expiratory pressure
- IHT:
-
Intra-hospital transfer
References
Al-Naami MY, Arafah MA, Al-Ibrahim FS (2010) Trauma care systems in Saudi Arabia: an agenda for action. Ann Saudi Med 30(1):50–58. https://doi.org/10.4103/0256-4947.59374. (PMID:20103958;PMCID:PMC2850182)
Rhee P, Joseph B, Pandit V, Aziz H, Vercruysse G, Kulvatunyou N, Friese RS (2014) Increasing trauma deaths in the United States. Ann Surg 260(1):13–21. https://doi.org/10.1097/SLA.0000000000000600. (PMID: 24651132)
Rau CS, Wu SC, Kuo PJ, Chen YC, Chien PC, Hsieh HY, Hsieh CH (2017) Polytrauma Defined by the New Berlin Definition: A Validation Test Based on Propensity-Score Matching Approach. Int J Environ Res Public Health 14(9):1045. https://doi.org/10.3390/ijerph14091045. (PMID:28891977;PMCID:PMC5615582)
van Breugel JMM, Niemeyer MJS, Houwert RM, Groenwold RHH, Leenen LPH, van Wessem KJP (2020) Global changes in mortality rates in polytrauma patients admitted to the ICU-a systematic review. World J Emerg Surg 15(1):55. https://doi.org/10.1186/s13017-020-00330-3. (PMID:32998744;PMCID:PMC7526208)
Diamond M, Peniston HL, Sanghavi D, et al (2023) Acute Respiratory Distress Syndrome. [Updated 2023 Feb 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436002/
Acute Respiratory Distress Syndrome Network; Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342(18):1301–8. https://doi.org/10.1056/NEJM200005043421801. PMID: 10793162
Menaker J, Tesoriero RB, Tabatabai A, Rabinowitz RP, Cornachione C, Lonergan T, Dolly K, Rector R, O’Connor JV, Stein DM, Scalea TM (2018) Veno-Venous Extracorporeal Membrane Oxygenation (VV ECMO) for Acute Respiratory Failure Following Injury: Outcomes in a High-Volume Adult Trauma Center with a Dedicated Unit for VV ECMO. World J Surg 42(8):2398–2403. https://doi.org/10.1007/s00268-018-4480-6. (PMID: 29340723)
Bahloul M, Dlela M, Bouchaala K, Triki A, Chelly H, Hamida CB, Haddar S, Bouaziz M (2020) Early post-traumatic pulmonary embolism in intensive care unit: incidence, risks factors, and impact outcome. Am J Cardiovasc Dis 10(3):207–218. PMID: 32923103; PMCID: PMC7486531
Reiff DA, Haricharan RN, Bullington NM, Griffin RL, McGwin G Jr, Rue LW 3rd (2009) Traumatic brain injury is associated with the development of deep vein thrombosis independent of pharmacological prophylaxis. J Trauma 66:1436–1440
Husain-Syed F, Ricci Z, Brodie D et al (2018) Extracorporeal organ support (ECOS) in critical illness and acute kidney injury: from native to artificial organ crosstalk. Intensive Care Med 44:1447–1459. https://doi.org/10.1007/s00134-018-5329-z
Moore AJE, Wachsmann J, Chamarthy MR, Panjikaran L, Tanabe Y, Rajiah P (2018) Imaging of acute pulmonary embolism: an update. Cardiovasc Diagn Ther 8(3):225–243. https://doi.org/10.21037/cdt.2017.12.01. PMID: 30057872; PMCID: PMC6039809
Bahloul M, Dlela M, Bouchaala K, Kallel H, Ben Hamida C, Chelly H, Bouaziz M (2020) Post-traumatic pulmonary embolism: incidence, physiopathology, risk factors of early occurrence, and impact outcome. A narrative review. Am J Cardiovasc Dis 10(4):432–443. PMID: 33224594; PMCID: PMC7675152
Sidebotham D (2011) Extracorporeal membrane oxygenation--understanding the evidence: CESAR and beyond. J Extra Corpor Technol 43(1):P23–6. PMID: 21449236; PMCID: PMC4680093
Bellani G et al (2016) Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 315:788–800. https://doi.org/10.1001/jama.2016.0291
Friedrichson B, Mutlak H, Zacharowski K et al (2021) Insight into ECMO, mortality and ARDS: a nationwide analysis of 45,647 ECMO runs. Crit Care 25:38. https://doi.org/10.1186/s13054-021-03463-2
Thompson BT, Chambers RC, Liu KD (2017) Acute Respiratory Distress Syndrome. N Engl J Med 377:562–72. https://doi.org/10.1056/NEJMra1608077
Salim A, Martin M, Constantinou C et al (2006) Acute Respiratory Distress Syndrome in the Trauma Intensive Care Unit: Morbid but Not Mortal. Arch Surg 141(7):655–658. https://doi.org/10.1001/archsurg.141.7.655
Jepson SL, Harvey C, Entwisle JJ, Peek GJ (2010) Management benefits and safety of computed tomography in patients undergoing extracorporeal membrane oxygenation therapy: experience of a single centre. Clin Radiol 65:881e886. https://doi.org/10.1016/j.crad.2010.05.007
Lee S, Chaturvedi A (2014) Imaging adults on extracorporeal membrane oxygenation (ECMO). Insights Imaging 5:731–742. https://doi.org/10.1007/s13244-014-0357-x
Wittram C (2007) How I do it: CT pulmonary angiography. AJR Am J Roentgenol 188:1255–1261. https://doi.org/10.2214/AJR.06.1104
Lidegran MK, Frenckner BP, Mosskin M et al (2006) MRI of the brain and thorax during extracorporeal membrane oxygenation: preliminary report from a pig model. ASAIO J 52:104–109. https://doi.org/10.1097/01.mat.0000194058.62228.56
Liu KL, Wang YF, Chang YC et al (2014) Multislice CT scans in patients on extracorporeal membrane oxygenation: emphasis on hemodynamic changes and imaging pitfalls. Korean J Radiol 15:322–329. https://doi.org/10.3348/kjr.2014.15.3.322
Acknowledgements
We thank all the critical care staff of Aseer Central Hospital, Abha, Aseer region, Kingdom of Saudi Arabia.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
OP: Literature search, manuscript editing, writing, and final revision. AB: concept, design, literature search, and manuscript preparation. SP: writing and editing. NM: report collection, data analysis, and manuscript preparation. HH: report collection, data analysis, and manuscript preparation. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The written informed consent was obtained from the father of the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al Bshabshe, A., Purushothaman, S., Alwadai, N.M. et al. Computed tomography pulmonary angiogram in a poly-trauma patient undergoing veno venous extracorporeal membrane oxygenation: our experience in diagnosing pulmonary embolism. Egypt J Bronchol 17, 50 (2023). https://doi.org/10.1186/s43168-023-00227-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00227-0