Abstract
Background
Bronchial asthma may mimic different diseases regarding their similar clinical presentations, so accurate assessment is required to exclude other possible diagnosis before confirming the diagnosis of bronchial asthma. The aim of the study was to identify the percentage of patients in whom the diagnosis of current asthma was confirmed or ruled out after clinical, spirometric assessment, and utilizing all the possible investigations.
Methods
A cohort study of newly diagnosed bronchial asthma in adults aged ≥ 18 years were recruited from chest outpatient clinic and chest department. History taking, clinical examination, chest X-ray, and spirometry were done for all patients, while chest high-resolution computed tomography (HRCT), CT pulmonary angiography, or different endoscopies were done when indicated.
Results
Two hundred recently clinically diagnosed asthmatic patients were recruited with a mean age of 43.2 and 53.4 years in the asthma group and asthma rule out group, respectively. About 55.5% of the studied patients were ruled out to have bronchial asthma after serial assessments of symptoms and spirometric function. There was increased chest wheeze as a respiratory symptom among asthma patients than the other group (p ˂ 0.001), while hemoptysis was significantly a more presenting symptom among patient group whose asthma diagnosis is ruled out (p = 0.009). About 87.6% of asthma confirmed group showed predominant reversible airway obstructive. The sputum cytology analysis of the bronchial asthma group of patients was 42.7% eosinophilic, 24.7% neutrophilic, and 32.6% mixed cellularity. After consuming all the available investigational tools, the most common diseases found among asthma rule out group were cardiac disorders, chronic obstructive pulmonary disease, psychological disorders, rhinitis, and gastro-esophageal reflux disease with percent of 11.5%, 9%, 8.5%, 8%, and 6%, respectively.
Conclusions
Utilizing all the available investigational tools in the present study allowed to exclude bronchial asthma and diagnose critical diseases that need specific and urgent therapies as heart diseases, subglottic stenosis, pulmonary hypertension, and interstitial lung diseases.
Trial registration
ClinicalTrials.gov NCT05776537. Retrospectively registered on 6 March 2023.
Similar content being viewed by others
Background
The diagnosis of bronchial asthma relies on the existence of characteristic respiratory symptoms which are reversible and variable (diurnal and seasonal) with variable airflow limitation. Unfortunately, bronchial asthma may mimic different pulmonary and non-pulmonary diseases regarding their similar clinical presentations so accurate assessment is required to exclude other possible diagnosis before confirming the diagnosis of bronchial asthma [1].
There are various phenotypes of asthma such as atopic, non-atopic, and late-onset asthma, which may not be easily diagnosed in the community. Also, asthma may show intermittent versus a relapsing/remitting course, so it is difficult to be diagnosed by a single physician visit. Different studies have found that patients with bronchial asthma were treated empirically without full assessment either to ensure or exclude the asthma diagnosis [2].
Some symptoms as chest wheezes and breathlessness may be presented commonly in bronchial asthma and other mimic diseases such as chronic obstructive pulmonary disease, bronchiectasis, congestive heart failure, vocal cord disorders, hypersensitivity pneumonitis, endobronchial tumors, pulmonary embolism, aspiration syndromes, tracheal compression by a mediastinal mass, and tracheomalacia. So, different physicians should put in mind those asthma mimics to be differentiated from asthmatic patients specially whose asthma symptoms are poorly controlled by anti-asthmatic medications [3].
The aim of the study was to identify the percentage of patients in whom the diagnosis of current asthma was confirmed or ruled out after clinical, spirometric assessment and utilizing all the possible investigations with a 6-month follow-up period for both groups.
Methods
Study design and setting
This cohort study was conducted on 200 recently clinically diagnosed asthma patients in the period between December 2020 to June 2022. It was carried out in chest outpatient clinic and inpatient wards, Zagazig University Hospitals, Egypt. This study was approved by Zagazig University Institutional review board (ZU-IRB # 6576/6-12-2020).
Patient selection
Inclusion criteria: (1) patients aged ≥ 18 years who had newly clinically diagnosed bronchial asthma (the diagnosis was achieved in the previous one year, to allow us to get the previous diagnostic reports) whether the diagnosis of asthma was initially made based on clinical assessment alone or both clinical and spirometric assessment. (2) Both sexes were included.
Exclusion criteria: (1) Patients who were using long-term oral steroids that may mask the diagnosis, (2) unable to do spirometry or contra-indicated, (3) pregnancy, and (4) definite diagnosis of other chest diseases.
Informed consent was taken from all patients included in the study.
Patients’ work-up
-
A.
Full-history taking which included age, sex, smoking history, occupation, duration of illness, different clinical symptoms, drug history, and family history of bronchial asthma or other atopic diseases.
-
B.
History of how patients were diagnosed as asthma whether the diagnosis of asthma was initially made based on clinical assessment alone or based on symptoms, physical findings, and diagnostic tests such as spirometry, reversibility test, and peak expiratory flows.
-
C.
Comprehensive clinical examination: general and local chest examination.
-
D.
The Asthma Control Questionnaire (ACQ-6) (for all patients) [4]:
ACQ-6 score has been shown to correlate with a measure of control based on the 2020 GINA guidelines [5]. Patients are asked to remember what happened to them in the previous week and to answer the 6 questions (night-time waking, symptoms on waking, activity limitation, shortness of breath, wheeze and rescue short-acting β2-agonist use) on a 6-point scale (0=no impairment; 6=maximum impairment). The ACQ score ranges between 0 (well controlled) and 6 (extremely poorly controlled). Scores of <0.75 = well controlled; 0.75–1.5 = not well controlled; >1.5 = uncontrolled.
-
E.
Spirometry (done for all patients):
Spirometry (pre- and post-bronchodilator) is the preferred test for objective diagnosis of variable and reversible airflow obstruction. Bronchial asthma (variable airflow obstruction) is diagnosed when: A 12% or greater improvement in forced expiratory volume in the first second of expiration (FEV1) and improvement > 200 ml from baseline 15 mins later after inhalation of 400 μg of an inhaled short-acting beta2 agonist (Salbutamol) [6]. A computerized pulmonary function apparatus (ZAN 100 spirometer; ZAN Messgeraete GmbH Company; Germany, 1999) was used.
-
F.
Sputum smear cytologic analysis (done for all patients), predominant eosinophilic sputum was considered (if sputum eosinophils ≥ 2% of sputum cells) [7].
-
G.
Chest X-ray was done for excluding any abnormal findings which may suggest other diagnosis than asthma or additional complications.
-
H.
Electrocardiogram (ECG) and echocardiography (ECHO) for confirmation of any cardiac problems.
-
I.
Chest-computed tomography (chest CT) either with intravenous contrast (to detect any suspect lung mass or lymphadenopathy), CT pulmonary angiography (for any pulmonary vascular abnormalities), or chest high resolution CT (chest HRCT) (can detect interstitial lung diseases and bronchiectasis).
-
J.
Fibreoptic bronchoscopy with bronchial aspirate, lavage, or biopsy if needed.
-
K.
Upper gastrointestinal (GI) endoscopy and esophageal motility assessment, whenever required.
-
L.
Ear, nose, and throat (ENT) consultation and laryngoscopy
-
M.
Psychiatric consultation and psychotherapy, if indicated
-
After completing all the previous clinical, functional, radiologic, and endoscopic assessment, the patients were classified into two groups: Group (1) (89 patients) whose diagnosis confirmed to be bronchial asthma and group (2) (111 patients) with diagnoses other than bronchial asthma.
-
A 6-month follow-up period for both groups, regarding bronchial asthma group (to confirm the diagnosis of asthma especially those with normal spirometry and typical asthma symptoms and to assess the patient’s adherence to treatment). While the other group with asthma rule out (all the asthma medications were stopped, while patients were treated individually according to their new diagnosis)
-
Statistical analysis
The analysis of data was done using the Statistical Program for Social Science (SPSS version 16) as follows: the description of quantitative variables as mean, standard deviation (SD), minimum, and maximum. The description of qualitative variables is done using number and percentage. The test which was used to compare qualitative variables between groups was chi-square. Independent sample t test was used to compare two groups regarding quantitative variable in parametric data. Paired sample t test was used to compare two related groups regarding quantitative variable in parametric data. A P value of more than 0.05 is insignificant, P less than 0.05 is significant, and P less than 0.01 is highly significant.
Results
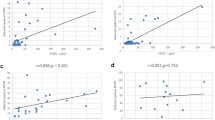
The patients were classified into two groups: group (1) (89 patients) whose diagnosis confirmed to be bronchial asthma (44.5% of all patients) and group (2) (111 patients) with diagnoses other than bronchial asthma (55.5% of all patients). Figure 1 illustrated the percentage of different diseases finally diagnosed among all the 200 patients: bronchial asthma were 44.5% and other mimic diseases were 55.5% including rhinitis (allergic and non-allergic) (8%), 6% were gastroesophageal reflux disease (GERD), 11.5% were cardiac patients, 9% were chronic obstructive pulmonary disease (COPD), bronchiectasis was diagnosed in 4% of patients, 3.5% (7 patients) had interstitial lung diseases (3 hypersensitivity pneumonitis, 2 rheumatoid arthritis and 2 idiopathic pulmonary fibrosis), 8.5% of the patients had psychological disorders, 1.5% had vocal cord dysfunction, and each of the following diseases was detected in 1% of the patients (subglottic stenosis, sarcoidosis, and primary pulmonary hypertension). Lastly, only one patient had trachea-bronchomalacia. Table 1 demonstrated that bronchial asthma was initially diagnosed by pulmonologist (77.5%) followed by internist (9%), cardiologist (7.9%), and lastly general practitioner (5.6%). Regarding the initial diagnosis of bronchial asthma, both clinical and spirometric assessment had the ability to diagnose about 70.8% of bronchial asthma patients with very high significant difference in comparison with the clinical assessment only which diagnosed 29.2% of bronchial asthma (P < 0.001) (Table 2). Regarding the baseline patient characteristics, Table 3 shows a statistically significant younger age among asthma patients than the other group (P 0.001), with statistically significant more smokers among the patients with diagnosis other than asthma (P 0.04), while they were matched in other general characters with no significant difference. Table 4 shows statistically significant increased wheeze as a complaint among asthma patients than the other group, and less presented with hemoptysis, while they were matched in other symptoms with no significant difference. Table 5 shows a high statistically significant difference among both groups regarding spirometry results as 87.6% of asthma patients presented with reversible obstructive spirometry (P < 0.001), while the other patient group demonstrated (normal, irreversible obstructive, restrictive, and mixed spirometric results in (65.8%, 18%, 9%, and 7.2% of patients), respectively. Table 6 shows a high statistically significant difference among both groups regarding sputum cytology results with predominant eosinophilic (if sputum eosinophils ≥ 2% of sputum cells) and mixed cellularity in asthma group (P value was <0.001).
Discussion
The overall asthma prevalence among the adult population over 18 years of age in some Middle East countries is 6.4%, ranging from 4.4% in Turkey to 6.7% in Egypt and 7.6% in the Gulf Cluster. Its clinical presentation has a wide differential diagnosis and may be associated with normal chest examination. There is no definite gold standard for asthma diagnosis, and the objective tests that can help in the diagnosis are often poorly available to primary care physicians [8].
Asthma misdiagnosis is largely widespread. It needs a clinical diagnosis, functional tests, and treatment trials. The hazards of overtreatment, negligence of alternative critical illnesses, and the financial cost of long-term undesired medications make overdiagnosis an important problem. Overdiagnosis can be avoided by the routine use of objective tests of airflow obstruction or bronchial hyperreactivity before starting any treatment [9].
In the current study, 111 adult patients (55.5%) who had been diagnosed with asthma in the previous year had no evidence of current asthma when they were prospectively evaluated with serial assessments of symptoms and spirometric function without using asthma medications for 6 months follow-up duration (Fig. 1). This is considered a high incidence of overdiagnosis of bronchial asthma at the initial diagnosis of those patients when compared with other similar studies: Luks et al. [10] about 30% of patients previously diagnosed as asthma by a physician were excluded as asthma after objective assessment using serial spirometry, bronchial challenge test, and tapering of asthma medications. No further investigations were done to confirm the diagnosis of other asthma mimic diseases. As asthma might be falsely over diagnosed in some patients. There are other non-asthmatic causes of bronchial hyperresponsiveness as (smoking history with normal spirometry, allergic rhinitis, or recent viral infection). Aaron et al. [2] excluded bronchial asthma in nearly 33.1% of their studied patients. The discrepancy with the current study results was because Aaron et al. [2] study was a larger multicenter Canadian study with longer 12-month follow-up period that allowed the exclusion of any asthma remission followed by a flare-up. Also, Heffler et al. [11] and Looijmans-van den Akker et al. [12] have suggested that over diagnosis of asthma may be detected among adults and children.
The causes of overdiagnosis in the present study were (1) about 89 patients (80.2%) of the patients group whose asthma diagnosis was ruled out and were diagnosed initially by clinical diagnosis only without any objective tests to confirm the asthma diagnosis. (2) The remaining 19.8% of the patients whose asthma diagnosis was ruled out were diagnosed clinically and functionally by spirometry, which was normal, but further investigations to rule out asthma were not done initially (Table 2).
Most of the currently studied patients were obese female with poorly controlled respiratory symptoms (ACQ > 1.5) with no significant difference between both groups regarding these patients’ characteristics (Table 3). This result was in consistent with other studies of late onset asthma as Aaron et al. [2] demonstrated that about 64.9% of their asthma confirmed patients’ group were females and overweighed. In the USA, adult-onset asthma is the predominant phenotype among females over 40 years age [13]. Factors predisposing to adult-onset asthma include female sex, obesity, occupational exposure, rhinitis, respiratory infections, smoking, and stressful life events suggesting that adult-onset asthma may be caused by different mechanisms [14].
After puberty, females may be more susceptible to develop asthma which also, may be severe disease [15]. This can be explained by a smaller airway diameter. Also, estrogen hormone inhibits the cortisol production and function, so it may cause severe uncontrolled asthma [16].
The mean age of the currently studied patients was 43.2 and 53.4 years in both patient groups, respectively (Table 3), with statistically significant older age in the asthma rule out group which mainly included diseases which are more prevalent above 50 years old (COPD, chronic heart diseases, rheumatoid arthritis, and idiopathic pulmonary fibrosis). This result agreed with Torén et al. [17] who found that the mean age of the adult-onset asthma population was 43.5 years, while COPD mainly occurs after 50 years of age. An overall incidence rate of asthma among adults around 2/1000 in the age group 20–50 years [18].
The present study detected more frequent chest wheeze as a respiratory symptom among asthma patients than the other group with very high statistical significance (p ˂ 0.001) (Table 4). This result was in concordant with Aaron et al. [2] as also both history of wheezing and dyspnoea were significantly associated with confirmed asthma diagnosis (p ˂ 0.001 and 0.04), respectively, while hemoptysis was significantly a more presenting symptom among patient group whose asthma diagnosis was ruled out (p = 0.009) (Table 4), the causes of hemoptysis in this group were one chronic heart disease, 7 bronchiectasis, one pulmonary hypertension, and 2 sarcoidosis patients.
There was highly statistically significant difference between both patients’ groups regarding spirometric results in the present study, as asthma confirmed group showed predominant reversible airway obstructive pattern (87.6% of patients), while bronchial asthma was excluded from about 16.2% of the second group (9% of patients showed restrictive spirometry and 7.2% of patients were mixed restrictive and obstructive pattern) (Table 5). Asthma misdiagnosis may occur during the initial assessment due to lack of use of objective tests for diagnosis of asthma as they may be unavailable in all primary care centres specially in the developing countries. The drawbacks of misdiagnosis are delay in the diagnosis and treatment of some critical diseases as heart diseases, pulmonary hypertension, and interstitial lung diseases and undesired use of chronic asthma medications with their side effects which may harm the non-asthmatics.
Aaron et al. [2] identified only 2.0% of studied patients, with severe untreated cardiac and pulmonary diseases which were initially misdiagnosed as asthma due to failure to perform objective tests. The advantages of the later study were included as follows: It was a multicenter cohort study where 461 patients were collected randomly from the community with follow-up over 12 weeks using objective tests by pulmonologists to confirm or rule out current asthma. So, some objective tests better to be requested by the physicians at the initial diagnosis of asthma (pre- and post-bronchodilator spirometry, serial peak flow measuring, or bronchial challenge tests).
About 35% of the patients whose asthma was excluded and were regularly adherent to asthma controller medications, were at high risk for side effects and cost and with little benefit [19]. Also, Pakhale et al. [20] suggested that ruling out asthma among asthmatic patients previously diagnosed by a physician is considered cost-effective.
Asthma is a chronic airway inflammation with different phenotypes. Each phenotype has its characteristic immunopathological mechanism, clinical features, disease severity, and response to treatment. These phenotypes were eosinophilic, neutrophilic, mixed granulocytic, and pauci-granulocytic asthma [21].
Regarding the current bronchial asthma group of patients, the sputum cytology analysis was 42.7% eosinophilic, 24.7% neutrophilic, and 32.6% mixed cellularity (Table 6). These results were in concordance with Al-Jahdali et al. [22] who studied severe asthmatic patients with mean age of 48.7 years, and they found that 45% of patients had the eosinophilic phenotype which was defined only based on a blood eosinophil count of ≥ 300 cells/mm3. Also, the prevalence of the eosinophilic asthma phenotype among severe asthma patients studied by Hiles et al. [23], Nagasaki et al. [24], and van Veen et al. [25] were 44%, 34%, and 44%, respectively. The prevalence of eosinophilia was mostly underestimated because conditions associated with eosinophilia such as nasal polyposis, adult-onset asthma, and chronic oral corticosteroid intake were not considered during the above different studies [26].
Dente et al. [27] observed that in uncontrolled asthmatic patients, despite a high level of medications with follow-up for 3 years, sputum eosinophilia (≥ 3%) was present in 87% of all sputum samples. Persistent sputum eosinophilia is a characteristic of severe uncontrolled asthma.
In the present study, the percent of asthmatic patients who had sputum neutrophilia was lower than those with sputum eosinophilia (24.7% versus 42.7%) (Table 6), this can be explained as the current asthmatic group was recently diagnosed with asthma, mostly non-smokers (53.9%), and their chest complaints were present for 1-year duration or slightly longer, and also 87.6% of this group had reversible airway obstruction. Ray and Kolls [28] stated that increased neutrophils in sputum have been detected with severe persistent asthma, adult onset, with a duration of asthma about 20 years or more and fixed airway obstruction.
While neutrophilic sputum was detected in 27.9% of the non-asthmatic group pf patients (COPD, bronchiectasis, and some ILD). Similarly, Gernez et al. [29] reported that chronic airway neutrophilic inflammation can be detected in different respiratory diseases, like severe asthma, chronic obstructive pulmonary disease (COPD), bronchiectasis, and infiltrative pulmonary diseases. This inflammatory type causes severe diseases which are resistant to different medications and hence considered as an economic and public health burden worldwide.
In the current study, after consuming all the available investigational tools, bronchial asthma was excluded in 55.5% of all the studied patients and other diagnoses were replaced, the most common diseases found were cardiac disorders, COPD, psychological disorders, rhinitis, and GERD with percent of 11.5%, 9%, 8.5%, 8%, and 6%, respectively (Fig. 1). The most frequently diagnosed diseases by Aaron et al. [2] after ruling out asthma were allergic or nonallergic rhinitis 25.3%, GERD 8.5%, anxiety 3.8%, obesity 3.3%, eosinophilic bronchitis 2.8%, ischemic heart disease 1.9%, and COPD 1.9%. The differences between the current study and Aaron et al. [2] study might be due to the fllowing: (1) we did not exclude a smoking history more than 10 pack-years from the current study, so the prevalence of COPD and cardiac diseases were more common than the later study; (2) Aaron et al. [2] assessed their patients by serial bronchial challenge tests, and those in whom asthma diagnosis was ruled out were followed up over 1 year by repeated bronchial challenge tests.
Conclusions
Utilizing all the available investigational tools in the present study allowed to exclude bronchial asthma and diagnose critical diseases that need specific and urgent therapies as heart diseases, subglottic stenosis, pulmonary hypertension, and interstitial lung diseases.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ILD:
-
Interstitial lung diseases
- HTN:
-
Hypertension
- GERD:
-
Gastro-esophageal reflux disease
- DM:
-
Diabetes miletus
- ECG:
-
Electrocardiogram
- COPD:
-
Chronic obstructive lung disease
- ACQ:
-
Asthma control questionnaire
- GINA:
-
Global Initiative for Asthma
- HRCT:
-
High-resolution computed tomography
- ENT:
-
Ear, nose, and throat
- GIT:
-
Gastrointestinal tract
- ZU-IRB:
-
Zagazig University—Institutional Review Board
References
Blakey JD, Zaidi S, Shaw DE (2014) Defining and managing risk in asthma. Clin Exp Allergy 44:1023–1032
Aaron SD, Vandemheen KL, FitzGerald JM et al (2017) Re-evaluation of diagnosis in adults with physician-diagnosed asthma. JAMA 317(3):269–279
Bacellar P, Silva M, Tinoco N, Costa F (2008) Oesophagus achalasia: differential diagnosis of asthma. Rev Port Pneumol 14:309–313
Khusial RJ, Honkoop PJ, van der Meer V et al (2020) Validation of online asthma control questionnaire and asthma quality of life questionnaire. ERJ Open Res 6:00289–02019. https://doi.org/10.1183/23120541.00289-2019
Global strategy for asthma management and prevention 2020. https://ginasthma.org/ [last Accessed 21 Nov 2020]
Graham BL, Steenbruggen I, Miller MR, et al. (2019) standardization of spirometry 2019 update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care, 200(8): e70-e88. https://doi.org/10.1164/rccm.201908-1590ST. PMID: 31613151; PMCID: PMC6794117
de Groot JC, Ten Brinke A, Bel EH (2015) Management of the patient with eosinophilic asthma: a new era begins. ERJ Open Res 1(1):00024–02015. https://doi.org/10.1183/23120541.00024-2015
Tarraf H, Aydin O, Mungan D et al (2018) Prevalence of asthma among the adult general population of five Middle Eastern countries: results of the SNAPSHOT program. BMC Pulm Med 18(1):68
Kavanagh J, Jackson DJ, Kent BD (2019) Over- and under-diagnosis in asthma. Breathe 15:e20–e27
Luks VP, Vandemheen KL, Aaron SD (2010) Confirmation of asthma in an era of overdiagnosis. Eur Respir J 36(2):255–260
Heffler E, Pizzimenti S, Guida G et al (2015) Prevalence of over-/misdiagnosis of asthma in patients referred to an allergy clinic. J Asthma 52(9):931–934
Looijmans-van den Akker I, van Luijn K, Verheij T (2016) Overdiagnosis of asthma in children in primary care: a retrospective analysis. Br J Gen Pract 66(644):152–157
Sood A, Qualls C, Schuyler M et al (2013) Adult-onset asthma becomes the dominant phenotype among women by age 40 years. The longitudinal CARDIA study. Ann Am Thoracic Soc 10(3):188–197
Jamrozik E, Knuiman MW, James A et al (2009) Risk factors for adult-onset asthma: a 14-year longitudinal study. Respirology 14(6):814–821
Tam A, Morrish D, Wadsworth S, Dorscheid D, Man SF, Sin DD (2011) The role of female hormones on lung function in chronic lung diseases. BMC Womens Health 11:24. https://doi.org/10.1186/1472-6874-11-24
Jamieson PM, Nyirenda MJ, Walker BR, Chapman KE, Seckl JR (1999) Interactions between oestradiol and glucocorticoid regulatory effects on liver-specific glucocorticoid inducible genes: possible evidence for a role of hepatic 11β- hydroxysteroid dehydrogenase type 1. J Endocrinol 160(1):103–109
Torén K, Ekerljung L, Kim JL et al (2011) Adult onset asthma in west Sweden–incidence, sex differences and impact of occupational exposures. Respir Med 105(11):1622–1628
Torén K, Gislason T, Omenaas E et al (2004) Incidence of asthma in relation to age, sex and respiratory symptoms e a prospective longitudinal study from Northern Europe (RHINE-study). Eur Respir J 24:942–946
Lucas AEM, Smeenk FWJM, Smeele IJ, van Schayck CP (2008) Overtreatment with inhaled corticosteroids and diagnostic problems in primary care patients, an exploratory study. FamPract 25(2):86–91
Pakhale S, Sumner A, Coyle D et al (2011) (Correcting) misdiagnoses of asthma: a cost effectiveness analysis. BMC Pulm Med 11(1):27
Simpson JL, Scott R, Boyle MJ, Gibson PG (2006) Inflammatory subtypes in asthma: assessment and identification using induced sputum. Respirology 11:54–61
Al-Jahdali H, Wali S, Albanna AS et al (2022) Prevalence of eosinophilic, atopic, and overlap phenotypes among patients with severe asthma in Saudi Arabia: a cross-sectional study. BMC Pulm Med 22:67
Hiles SA, Gibson PG, McDonald VM (2021) Disease burden of eosinophilic airway disease: comparing severe asthma, COPD, and asthma-COPD overlap. Respirology 26:52–61
Nagasaki T, Sato K, Kume N, Oguma T, Sunadome H, Ito I et al (2019) The prevalence and disease burden of severe eosinophilic asthma in Japan. J Asthma 56:1147–1158
van Veen IH, Ten Brinke A, Gauw SA, Sterk PJ, Rabe KF, Bel EH (2009) Consistency of sputum eosinophilia in difficult-to-treat asthma: a 5-year follow-up study. J Allergy Clin Immunol 124:615–617
Jackson D, Busby J, Heaney LG, Menzies-Gow A, Pfeffer P, Perez-de-Llano L et al (2020) A global survey of blood eosinophil distribution in severe asthma patients: data from the International Severe Asthma Registry (ISAR). Am J Respir Crit Care 201:A4522. https://doi.org/10.1164/ajrccm-conference.2020.201.1_MeetingAbstracts.A4522
Dente F, L, Latorre M, Novelli F, et al (2015) Can sputum eosinophilia be a constant feature in severe refractory asthmatics? A 3-year longitudinal study. Int Arch Allergy Immunol 166:287–290
Ray A, Kolls JK (2017) Neutrophilic inflammation in asthma is associated with disease severity. Trends Immunol 38:942–954
Gernez Y, Tirouvanziam R, Chanez P (2010) Neutrophils in chronic inflammatory airway diseases: can we target them and how? Eur Respir J 35(3):467–469
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SMS designed the study, literature search, and manuscript preparation. AE collected the patients and followed up the data analysis. EMM edited, reviewed, and published the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Zagazig University Institutional review board (ZU-IRB # 6576/6-12-2020). Written informed consent was obtained from all patients prior to their initial study participation.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shehata, S.M., Mahmoud, E.M. & Elhawary, A. Assessment of asthma mimics among newly diagnosed bronchial asthma patients in Zagazig University Hospitals. Egypt J Bronchol 17, 33 (2023). https://doi.org/10.1186/s43168-023-00194-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00194-6