Abstract
Background
Biphasic positive airway pressure, also known as BIPAP, is a type of pressure-controlled ventilation that permits unrestricted spontaneous breathing at any time during the ventilatory cycle. Our study’s objective was to compare BIPAP’s effects on ARDS patients with those of the synchronized intermittent mandatory ventilation with pressure control (SIMV-PC) mode.
Results
The present observational, cross-sectional study was conducted on 40 ARDS patients of both sex. These patients were admitted to the intensive care unit, at Qena University Hospital, from April 2019 to November 2021. They were categorized into two groups at random, with group (A) patients receiving BIPAP mode and group (B) patients receiving (SIMV-PC) mode. Changes in arterial blood gases, hemodynamics, and lung mechanics (mean airway pressure, minute volume, tidal volume, compliance, and pressure limit) were compared in both groups after 24 h. There were no differences in the baseline clinical data, demographic, hemodynamic, arterial blood gases, and mortality between the two groups. Follow-up data after 24 h showed that BIPAP was associated with better hemodynamics, oxygenation, and lung mechanics (mean airway pressure, minute volume, and tidal volume). Fewer days of sedation requirements and mechanical ventilation in BIPAP compared to SIMV PC during the duration of the study.
Conclusions
In ARDS patients, BIPAP can improve oxygenation, hemodynamics, lung mechanics, decrease sedation use, and decrease duration of mechanical ventilation.
Trial registration
BIPAP in the Management of Acute Respiratory Distress Syndrome, ID: NCT05483959 Retrospectivelyregistered,https://register.clinicaltrials.gov/prs/app/template/EditRecord.vm?epmode=View&listmode=Edit&uid=U0003OBB&ts=12&sid=S00078AY&cx=9n7oml. Registered on 1 August 2022.
Similar content being viewed by others
Background
Acute respiratory distress syndrome is a severe form of acute lung injury (ALI) which is marked by bilateral pulmonary infiltrates and severe hypoxemia in the absence of cardiogenic pulmonary edema. Mortality and morbidity rates for ARDS remain high. The cornerstone of patient care continues to be mechanical ventilation [1]. Lung protective strategies (LPS) were one of the most effective strategies in patients with ARDS [2]. However, low tidal volumes during LPS may reduce lung inflation and increase the tendency of atelectasis and hypoxemia [3, 4].
Biphasic mode (BIPAP) is firstly used in clinical practice in the late 1980s. Biphasic positive airway pressure (BIPAP) is a system that permits unrestricted spontaneous breathing at any time during the ventilatory cycle. It is also known as pressure controlled mode of ventilation [5]. BIPAP offers several advantages over traditional strategies to improve the pathophysiology in these patients, including gas exchange, cardiovascular function, and reducing the need for sedation. This is because BIPAP allows spontaneous breathing throughout the ventilatory cycle [6]. In our study, we aimed to compare the efficacy of biphasic positive airway pressure mode of ventilation to traditional mode (SIMV PC) in ARDS patients.
Methods
Study design
This is an observational cross-sectional study registered (ClinicalTrials.gov ID: NCT05483959). The study was performed in the intensive care unit in Qena University Hospital from April 2019 to November 2021. The study design was approved by the Scientific Ethics Committee of the Faculty of Medicine of South Valley University. After meeting the inclusion criteria, informed consent is obtained from the patient.
Patient selection
The study was carried out on forty (40) ARDS patients categorized based on the patient’s degree of ARDS severity as being severe and diagnosed according to Berlin criteria [7]. The patients were intubated and mechanically ventilated via Puritan Bennett 840 ventilator system.
Inclusion criteria
All intubated adult patients diagnosed with ARDS are recruited in our study. ARDS is diagnosed according to Berlin criteria 2012 [7].
Exclusion criteria
Exclusion criteria included age <18, cardiac or respiratory arrest on admission, morbid obesity with BMI > 40, acute exacerbation of IPF, cerebrovascular or neuromuscular disorder, diabetic ketoacidosis, hepatic or renal disease, and cardiac disease.
Baseline data
All selected patients in the study were subjected to the following:
-
1-
A detailed history was taken
-
2-
Clinical examination, including both local and general examinations
-
3-
Arterial blood gases (ABG)
-
4-
Chest X-ray
-
5-
Laboratory assessment:
-
A-
Renal function test including, blood urea, and creatinine
-
B-
Complete blood picture
-
C-
Liver function tests including liver enzymes, total bilirubin, and serum albumin
-
A-
Method
-
We used a dormicum in all patients with a maintenance dose 0.1–0.2 mg/kg/h via iv infusion, and we used a prone position in some patients and used glucocorticoids for some patients with refractory hypoxemia despite ventilator management and antibiotic regimen. Patients with ARDS were randomly assigned to one of two protocol groups, and each of them received the same standard general care and two distinct ventilatory strategies:
-
BIPAP group (group A): This group of 20 patients underwent BIPAP ventilation.
-
SIMV PC group (group B): There were 20 patients in this group that used SIMV PC for ventilation.
The following settings were adjusted for Group A:
-
PLow: from 0:5 cm H2O
-
PHigh: the pressure that is adjusted from 25:30 cm H2O to promote lung protection and does not exceed 30 cm H2O
-
THigh: was adjusted in 4–6 s to promote a high inversed ratio
-
The mean airway pressure on BIPAP was calculated according to the formula:
$$\left(\textrm{Phigh}\ast \textrm{Thigh}\ \right)+\left(\textrm{Plow}\right)/\textrm{Thigh}$$
The following settings were adjusted for group B:
-
Inspiratory pressure was adjusted to obtain a tidal volume of 6 mL/kg IBW and SO2 >90 %.
-
Pressure support was adjusted in ARDS on 5–10 cm H2O.
-
PEEP was started at 10 cm H2O according to PVC (pressure-volume curve) and increased in increments 2 cm H2O and to be above the lower inflection point by 2 cm H2O.
-
FiO2 was adjusted to target a peripheral saturation SO2 >90%.
-
RR was adjusted at 16–20 breaths/minute targeting minute volume = 4 × the body surface area.
Statistical analysis
Data was collected, coded, and analyzed using SPSS (Statistical Package for the Social Science, version 20. For the qualitative data, it was presented as numbers and percentages. For the quantitative data with a parametric distribution, it was resented as mean, standard deviations, and ranges, and for the quantitative data with a non-parametric distribution, the median with interquartile range (IQR) is used. Chi-square test was used in the comparison between two groups with qualitative data, and the Fisher’s exact test was applied in its place when the predicted count in any cell was less than 5. When comparing two groups with quantitative data and a parametric distribution, an independent t test was employed, and when comparing two groups with quantitative data and a non-parametric distribution, a Mann-Whitney test was used. The level of confidence was kept at 95%, and hence, the P value was considered significant if < 0.05.
Results
There were no statistically significant differences between groups regarding age, gender, and baseline clinical parameters (respiratory rate, mean arterial blood pressure, heart rate). They were presented in Table 1.
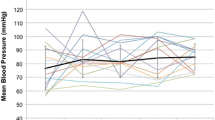
The follow-up of clinical parameters of both groups in Figs. 1 and 2 documented that HR and RR were significantly (P<0.01) decreased, while Fig. 3 showed that MAP (mean arterial blood pressure) was significantly (P<0.01) increased after 24 h in both groups, with a significant (P<0.01) decrease in SIMV PC and significant (P<0.01) increase in BIPAP.
Arterial blood gases are demonstrated in Figs. 4, 5, and 6, and the follow-up of acid-base status documented that PaCO2 (Fig. 4) significantly (P<0.05) increased after 24 h in both groups and the follow-up of oxygenation status was presented in (Figs. 5 and 6) and showed that SO2 and PaO2/FIO2 were significantly (P<0.05) higher in BIPAP versus SIMV PC.
Lung mechanics among groups A and B were presented in Table 2 and showed that VT, minute volume, and mean airway pressure were significantly (P<0.05) higher in BIPAP while other parameters were not significant.
The duration of mechanical ventilation among both groups was presented in Table 3 and showed a statistically significant (P<0.01) decrease in BIPAP versus SIMV PC, and also, the duration of anesthesia in days was presented in Table 3 and showed a statistically significant (P<0.001) decrease in BIPAP versus SIMV PC. Both groups in (Fig. 7) showed no statistically significant differences regarding the outcome (P>0.05).
Discussion
In the ARDS group, our study aims to compare BIPAP’s effects on hemodynamics (heart rate, mean blood pressure, and respiratory rate), ABG (pH, PaCO2, PaO2, and hypoxic index), lung mechanics (tidal volume, compliance, pressure limit, minute volume, and mean airway pressure), the need for sedation, the duration of mechanical ventilation, and the outcome in ARDS in comparison to SIMV PC.
Between the studied groups, there were no significant variations in baseline clinical variables or demographic data. There were no significant differences between the studied groups in measuring respiratory rate, heart rate, and mean arterial blood pressure. The results of our study support those of Varpula et al., Dart et al., Yoshida et al., Varpula et al., and Mohammed et al.—they found no variations in mean blood pressure and heart rate between traditional ventilator modes and APRV/BIPAP mode [8,9,10,11,12].
Further, follow-up clinical parameters including HR, RR, and MAP showed improvement 24 h after ventilation, with no significant differences between groups. It was believed that during BIPAP, elevated intrathoracic, and mean airway pressure could reduce venous return and cardiac output. However, it has been demonstrated that BIPAP does not negatively impact hemodynamics and may even improve them due to the ability of spontaneous breathing. Our study’s findings are consistent with several studies of Li et al., Hussein et al., Kamath et al., Putensen et al., Song et al., and Calzia et al. are in agreement with our study [13,14,15,16,17,18].
Numerous researches, including Kallet RH and Putensen C et al. demonstrated spontaneous breathing role in improving hemodynamics in mechanically ventilated ARDS patients [19, 20].
Acid-base balance showed no statistically significant difference between both groups. The findings of the present study are consistent with those of Mohammed et al., Gonzalez et al., Varpula et al., Yoshida et al., and Walkey et al., they found that pH and serum bicarbonate levels have no differences between conventional ventilator modes and BIPAP mode in ARDS patients [8, 10, 12, 21, 22].
As according to Varpula et al., Putensen et al., Walkey et al., Dart et al., Mohammed et al., and Gonzalez et al. research results from earlier clinical studies found that partial pressure of carbon dioxide level measurements showed no differences between conventional ventilator modes and BIPAP mode in ARDS patients which agree with our results. As regards baseline hypoxic index, no statistically significant difference between both groups while there was a highly statistically significant increase at 24 h. Hypoxic index was significantly improved with BIPAP when compared to SIMV PC [9, 11, 12, 17, 21, 22].
Varpula et al. and Li et al. also supported these findings [9, 13]. Walkey and colleagues reported that the criteria for pulmonary contusion were met by patients who required mechanical breathing for more than 48 h. They discovered that, when compared to conventional ventilation, hypoxic index was greater during APRV/BIPAP. BIPAP is expected to have a conceptual advantage due to its significant higher mean airway pressure and preservation of spontaneous breathing, whereas various studies have demonstrated that BIPAP without spontaneous ventilation was similar to conventional pressure-controlled MV and did not affect gas exchange [22]. In BIPAP, patients are able to control the frequency and length of spontaneous inspiration and expiration, which is a special mechanism that enables them to maintain a sinusoidal flow pattern similar to natural spontaneous breathing and to produce a diaphragmatic contraction. Patients can breathe spontaneously during any phase of the procedure.
Myers and MacIntyre in their study, data from many clinical crossover studies showed that APRV/BIPAP produced better oxygenation than conventional ventilation modes probably due to mean pressure produced by the prolonged inflating period and the improved distribution during spontaneous breathing [23].
On evaluating lung mechanics of both groups, There was a high statistically significant increase of the Mean airway pressure, minute volume, and tidal volume in the BIPAP group, while pressure limit and compliance showed no statistically significant difference between both groups.
Furthermore, Yoshida et al. performed a retrospective investigation to ascertain which modality, pressure support ventilation (PSV) or APRV/BIPAP, lessens atelectasis in patients with acute lung injury and acute respiratory distress syndrome (ARDS). There were no obvious changes between the ventilatory modes over the research periods, and it was discovered that mean airway pressure and peak pressure in both groups were moderate (p = 0.391 in Paw mean and p = 0.334 in Paw peak). Since the airway pressures in both groups were similar and moderate, they concluded that the advantage of BIPAP appeared to result from the preservation of spontaneous breathing rather than from a large mean airway pressure. The fact that APRV/BIPAP is a pressure-control mode of breathing is probably responsible for a decrease in peak airway pressure significantly. This may help to explain the difference between APRV/BIPAP and pressure support ventilation that Yoshida and colleagues found (PSV) [10].
On evaluating the duration of sedation requirements of both groups, when compared to the SIMV PC group, the BIPAP group experienced a significantly shorter duration of sedation needs. This dramatic reduction in sedation needs is attributable to the BIPAP patient’s ability to breathe spontaneously throughout the ventilator cycle, which improves patient-ventilator synchrony.
On evaluating the mechanical ventilation duration, there was a high statistically significant difference between both groups. Duration of mechanical ventilation was much lower in the BIPAP group versus the SIMV PC group. These results are similar to the study done by Abo et al., Mohammed et al., and Zhou et al. [12, 24, 25].
In a retrospective research (2004) involving more than 600 cardiac surgery patients, it was discovered that allowing patients to breathe spontaneously from the start with APRV/BIPAP led to a reduction in the need for analgesics and sedatives. According to preliminary data, the amount of analgesics and sedatives used by patients with multiple trauma who utilize APRV/BIPAP to sustain spontaneous breathing throughout an observation period of more than 10 days is much lower than that of patients who use controlled ventilation for 72 h before weaning [26].
In a unique research study, ARDS patients who had already been sedated and paralyzed with inverse-ratio ventilation were switched to APRV/BIPAP. To maintain a constant stimulated bispectral index (BIS) value of 70, approximately 70% less neuromuscular blockade and 30% less sedation (benzodiazepines) were needed [27].
In a cohort trial, Marik et al. employed APRV/BIPAP with low-level pressure support (PS) to assess the effects on oxygenation and ventilation parameters in patients with severe ARDS. During the trial period, oxygenation and ventilation data, as well as the administration of sedative and vasopressor drugs, were reported for patients with severe ARDS who were converted to APRV/BIPAP from low tidal volume assist-controlled (AC) ventilation. Surprisingly, they discovered that patients tolerate APRV/BIPAP very well, allowing many patients to stop using sedatives. After 24 h of APRV/BIPAP, the daily dosage of sedatives and vasopressors was reduced by 46% [28].
In the present study, both groups showed no statistically significant difference in relation to the outcome. Numerous studies concur with us that APRV/BIPAP did not reduce ARDS patient death, but it was linked to a shorter stay in the critical care unit (ICU) [14, 17, 29].
In contrast to what we found, Liu et al. discovered that ICU mortality was significantly lower in the APRV group compared to the SIMV group and that APRV and SIMV were associated with equivalent lengths of mechanical ventilation and ICU stays. The results may have been greatly impacted by the severity of ARDS among the patient participants in the study [30].
All of the aforementioned research indicates that BIPAP considerably lessens the requirement for sedation and neuromuscular blockade. This is a crucial concern since more frequent sedation has been linked to longer periods of mechanical ventilation, higher rates of ventilator-associated pneumonia, delirium, and higher mortality [31].
Conclusion
-
In ARDS BIPAP with a longer Thigh of high pressure is superior to conventional SIMV PC with better recruitment and oxygenation with less hemodynamic compromise and a shorter duration of mechanical ventilation.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BIPAP:
-
Biphasic positive airway pressure
- ARDS:
-
Acute respiratory distress syndrome
- SIMV PC:
-
Synchronized intermittent mandatory ventilation pressure control
- ALI:
-
Acute lung injury
- LPS:
-
Lung protective strategies
- ABG:
-
Arterial blood gases
- PHigh:
-
Pressure high
- PLow:
-
Pressure low
- Thigh:
-
Time high
- VT:
-
Tidal volume
- PEEP:
-
Positive end-expiratory pressure
- PVC:
-
Pressure volume curve
- MAP:
-
Mean arterial pressure
References
Fan E, Needham DM, Stewart TE (2005) Ventilatory management of acute lung injury and acute respiratory distress syndrome. JAMA 294(22):2889–2896
Villagra, A N A Ochagavia, A N A Vatua, Sara Murias, Gaston DEL MAR FERNÁNDEZ, MARIA Aguilar, Josefina Lopez Fernández, Rafael Blanch, Lluiset al (2002) Recruitment maneuvers during lung protective ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med 165(2):165–170
Richard J-C, Maggiore SM, Jonson B, Mancebo J, Lemaire F, Brochard L (2001) Influence of tidal volume on alveolar recruitment: respective role of PEEP and a recruitment maneuver. Am J Respir Crit Care Med 163(7):1609–1613
Network ARDS (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342(18):1301–1308
Hörmann C, Baum M, Putensen CH, Mutz NJ, Benzer H (1994) Biphasic positive airway pressure (BIPAP)--a new mode of ventilatory support. Eur J Anaesthesiol 11(1):37–42
Borges JB, Okamoto VN, Matos GFJ, Caramez MPR, Arantes PR, Barros F et al (2006) Reversibility of lung collapse and hypoxemia in early acute respiratory distress syndrome. Am J Respir Crit Care Med 174(3):268–278
Rubenfeld GD, Thompson T, Ferguson ND, Caldwell E, Fan E, Camporota L et al (2012) Acute respiratory distress syndrome. The Berlin definition. JAMA 307(23):2526–2533
Varpula T, Jousela I, Niemi R, Takkunen O, Pettilä V (2003) Combined effects of prone positioning and airway pressure release ventilation on gas exchange in patients with acute lung injury. Acta Anaesthesiol Scand 47(5):516–524
Dart BW IV, Maxwell RA, Richart CM, Brooks DK, Ciraulo DL, Barker DE et al (2005) Preliminary experience with airway pressure release ventilation in a trauma/surgical intensive care unit. J Trauma Acute Care Surg 59(1):71–76
Yoshida T, Rinka H, Kaji A, Yoshimoto A, Arimoto H, Miyaichi T et al (2009) The impact of spontaneous ventilation on distribution of lung aeration in patients with acute respiratory distress syndrome: airway pressure release ventilation versus pressure support ventilation. Anesth Analg 109(6):1892–1900
Varpula T, Valta P, Niemi R, Takkunen O, Hynynen M, Pettilä V (2004) Airway pressure release ventilation as a primary ventilatory mode in acute respiratory distress syndrome. Acta Anaesthesiol Scand 48(6):722–731
Sharaf M, El-Hantery M, Noaman M, Abel-Salam Y (2012) Biphasic intermittent positive airway pressure ventilation versus conventional ventilation in acute respiratory distress syndrome and acute lung injury. Trends Med Res 7:43–52
Li JQ, Li N, Han GJ, Pan CG, Zhang YH, Shi XZ et al (2016) Clinical research about airway pressure release ventilation for moderate to severe acute respiratory distress syndrome. Eur Rev Med Pharmacol Sci 20(12):2634–2641
Hussein K, Mohamed S, Ahmed Y (2015) Airway pressure release ventilation in management of acute respiratory distress syndrome: a 2-years experience from upper Egypt. Med Sci 4:11–17
Kamath SS, Super DM, Mhanna MJ (2010) Effects of airway pressure release ventilation on blood pressure and urine output in children. Pediatr Pulmonol 45(1):48–54
Song S, Tian H, Yang X, Hu Z (2016) The clinical effect of airway pressure release ventilation for acute lung injury/acute respiratory distress syndrome. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 28(1):15–21
Putensen C, Zech S, Wrigge H, Zinserling J, Stuber F, Von Spiegel T et al (2001) Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med 164(1):43–49
Calzia E, Pradermacher P (1997) Airway pressure release ventilation and biphasic positive airway pressure. A 10-year literature review. Clin Intensive Care 8(6):296–301
Kallet RH (2011) Patient-ventilator interaction during acute lung injury, and the role of spontaneous breathing: part 1: respiratory muscle function during critical illness. Respir Care 56(2):181–189
Putensen C, Mutz NJ, Putensen-Himmer G, Zinserling J (1999) Spontaneous breathing during ventilatory support improves ventilation--perfusion distributions in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 159(4):1241–1248
González M, Arroliga AC, Frutos-Vivar F, Raymondos K, Esteban A, Putensen C et al (2010) Airway pressure release ventilation versus assist-control ventilation: a comparative propensity score and international cohort study. Intensive Care Med 36(5):817–827
Walkey AJ, Nair S, Papadopoulos S, Agarwal S, Reardon CC (2011) Use of airway pressure release ventilation is associated with a reduced incidence of ventilator-associated pneumonia in patients with pulmonary contusion. J Trauma Acute Care Surg 70(3):E42–E47
Myers TR, Macintyre NR (2007) Does airway pressure release ventilation offer important new advantages in mechanical ventilator support? Respir Care 52(4):452–460
El-Asmar ABH, Awad TAE, El-Didamony AA (2019) Comparative study between airway pressure release ventilation and synchronized intermittent mandatory ventilation in treatment of acute respiratory distress syndrome. Egypt J Hosp Med 76(1):3329–3334
Zhou Y, Jin X, Lv Y, Wang P, Yang Y, Liang G et al (2017) Early application of airway pressure release ventilation may reduce the duration of mechanical ventilation in acute respiratory distress syndrome. Intensive Care Med 43(11):1648–1659
Grasso S, Fanelli V, Cafarelli A, Dalfino L, Ingenito G, Ancona G et al (2004) Patient ventilator interaction during PSV at different levels of sedation in ALI patients. Intensive Care Med 30(Suppl 1):S13
Kaplan LJ, Bailey H, Formosa V (2001) Airway pressure release ventilation increases cardiac performance in patients with acute lung injury/adult respiratory distress syndrome. Crit Care 5(4):1–6
Marik PE, Delgado EM, Baram M, Gradwell G, Romeo S, Dutill B (2009) Effect of airway pressure release ventilation (APRV) with pressure support (PS) on indices of oxygenation and ventilation in patients with severe ARDS: a cohort study. Crit Care Shock 12:43–48
Lim J, Litton E, Robinson H, Das GM (2016) Characteristics and outcomes of patients treated with airway pressure release ventilation for acute respiratory distress syndrome: a retrospective observational study. J Crit Care 34:154–159
Liu L, Tanigawa K, Ota K, Tamura T, Yamaga S, Kida Y et al (2009) Practical use of airway pressure release ventilation for severe ARDS—a preliminary report in comparison with a conventional ventilatory support. Hiroshima J Med Sci 58(4):83–88
Pandharipande P, Shintani A, Peterson J, Pun BT, Wilkinson GR, Dittus RS et al (2006) Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. J Am Soc Anesthesiol 104(1):21–26
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All the authors participated in the conception and design. SSS and KH collected the data and samples. KH, MSB, AR, GSG, and SSS were responsible for the analysis and interpretation of data. KH and AR were responsible for drafting the article. KH, MSB, and AR revised it critically for final approval of the version to be published. The authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Local Ethics Committee of the Qena University Hospital, the committee’s reference number IRB no: QMEC342019 and was conducted in accordance with the provisions of the Declaration of Helsinki. Written informed consent was obtained from all the participants before enrollment.
Consent for publication
All the authors approved the manuscript for publication. Identifying images or other personal or clinical details of participants is “not applicable.” Consent for publication from the participants is “not applicable.”
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salem, S.S., Hussein, K., Badawy, M.S. et al. Biphasic positive airway pressure in the management of acute respiratory distress syndrome: a comparative study. Egypt J Bronchol 17, 23 (2023). https://doi.org/10.1186/s43168-023-00188-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00188-4