Abstract
Background
Periodic limb movements during sleep (PLMS) and obstructive sleep apnea syndrome (OSAS) are two frequent coincident sleep disorders. The association of PLMS with OSAS severity and predictors of PLMS in OSAS patients were investigated.
Material and method
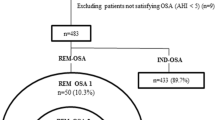
This is a retrospective study that enrolled adult patients ≥ 16 years old who visited the sleep unit at Mouwasat Hospital, Saudi Arabia, between January 2021 and October 2021. All were subjected to full medical history, clinical examination, Epworth Sleepiness (ESS), STOP-Bang questionnaires, and standard overnight polysomnography. Subjects were subdivided into two groups based on PSG findings: group I, OSA patients (153). Patients were classified into mild n = 57 (AHI ≥ 5 and < 15), moderate n = 35 (AHI ≥ 15 and < 30), and severe n = 61 (AHI ≥ 30). Group II, control group included 100 subjects.
Result
There was a higher frequency of PLMS in OSA patients vs control group (with a statistically significant value). The study showed a statistically significantly positive correlation between PLMI and each of AHI, hypopnea index, desaturation index, and PLMs with arousal index, in contrast; it had a statistically significantly negative correlation with BMI among the OSA group. By performing multivariate logistic regression to predict the possible factors associated with the existence of PLMS among the OSA group, it was showed that the apnea index and desaturation index were statistically significant predictors.
Conclusion
The present study showed that OSA patients with PLM were older; had greater AHI, hypopnea index, desaturation index, and PLMs with arousal index; and had lower BMI. Further studies are needed for better understanding this complex relationship.
Similar content being viewed by others
Background
The recent third international classification of sleep disorders (ICSD-3) categorizes sleep disorders into six main groups, with sleep breathing disorders (SBD) and sleep movement disorders (SMD) in the second and sixth groups of this classification respectively [1].
Periodic limb movement disorder during sleep (PLMs) is the most common alteration in the SMD group, which appears in polysomnograms as frequent episodes of muscle contractions each lasting 0.5 s and no longer than 10 s, separated by an interval of 5–90 s. PLMS at the rate of 15 or more/hour of sleep is considered abnormal and is supportive for diagnosis of PLMD if associated with hypersomnia/insomnia, which could not be explained by other current sleep disorders or other disorders [2].
Obstructive sleep apnea–hypopnea syndrome (OSAHS) is the most frequent in the SBD group, characterized by frequent episodes of upper airway obstruction during sleep causing repetitive arousals and sleep disruption [3].
Although both PLMS and OSAHS may be associated with cortical awakening or autonomic activation, it is important to differentiate between them. As some body movements may be found during or behind apnea events with difficulty in their identification by clinicians, furthermore the association of upper airway resistance syndrome (UARS), the component event being respiratory effort-related arousal (RERA), with PLMS is found in certain patients [4].
Since both PLMS and OSAS are two common sleep disorders, the present study aimed to assess the prevalence of PLMS in different OSAS severity and detect predictors of PLMS in OSAS patients.
Material and methods
This is a retrospective study that enrolled adult patients ≥ 16 years old who visited the sleep unit at Mouwasat Hospital, Saudi Arabia, between January 2021 and October 2021.
The protocol of the study was approved by the hospital research ethical committee, and written informed consent was obtained from every participant.
High risk for OSA was according to STOP-BANG Score ≥ 3 [5]; ESS score ≥ 11 [6] was included in the study.
We considered two groups in this work based on PSG findings: group I OSA: 153 patients with AHI ≥ 5 events/h with further classification into mild n = 57 (AHI ≥ 5 and < 15), moderate n = 35 (AHI ≥ 15 and < 30), and severe n = 61 (AHI ≥ 30), and group II control group: n = 100 patients with AHI < 5 events/h.
Patients with other sleep disorders as restless leg syndrome, narcolepsy, and rapid eye movement sleep behavior disorders were excluded. Patients with a history of Parkinson’s disease, kidney disease, pregnancy, multiple sclerosis, or medications, e.g., lithium, some antidepressants, and dopamine-receptor antagonist that might induce PLMS, were also excluded. Those with mood disorders, alcoholism, congestive heart failure, and dysrhythmias were not included in the study.
Methods
Prior to PSG, all subjects underwent full medical history taking, clinical examination, and completion of both questionnaires: Epworth Sleepiness (ESS) and Stop Bang scales.
We performed standard attended overnight polysomnography (PSG) at the sleep laboratory using the PSG device SOMNOscreen™ plusTM.
In standard PSG, electroencephalogram, electrooculogram, electrocardiogram, chin electromyogram (EMG), oronasal airflow, oxygen saturation by finger pulse oximetry, thoraco-abdominal and leg movements, and a digital microphone for snoring detection were all recorded.
Data obtained from PSG included in this study
Total time in bed, total sleep time, sleep efficiency, and oxyhemoglobin saturation.
Apnea (complete cessation of airflow breathing at nostrils and mouth for at least 10 s or more), hypopnea (decrease in rate and depth of breathing by 50% for 10 s or longer).
Indices and oxygenation
Apnea–hypopnea index (AHI): to grade OSA, the average number of apnea and hypopnea per hour of sleep [7].
-
1-
Respiratory disturbance index (RDI): measures not only apneas and hypopneas, but also respiratory event-related arousals (RERAS) that measure disruptions in sleep other than apneas or hypopneas.
-
2-
Oxygen desaturation index (ODI): average number of desaturation episodes per hour of sleep. A decrease in the mean oxygen saturation of ≥ 4% over the last 120 s, that lasts for at least 10 s considered a desaturation episode [8].
-
3-
Periodic limb movement index (PLMI), PLM-arousal index: total number of sleep-related PLMs per hour of sleep associated with an EEG arousal.
-
4-
Other indices: wake and arrhythmia indices also included.
Statistical analysis
Data analysis was performed using the Statistical Package of Social Science (SPSS) software version 22 in windows 7 (SPSS Inc., Chicago, IL, USA). Simple descriptive analysis was done in the form of numbers and percentages of qualitative data, and arithmetic means as central tendency measurement, and standard deviations as a measure of the dispersion of quantitative parametric data. Independent samples t test and the Mann–Whitney test were used to compare two independent groups. One-way ANOVA test and the Kruskal–Wallis test were used to compare quantitative measures between more than two independent groups of quantitative data. Chi-square test was used to compare two and more than two qualitative groups. The MC-Nemar test was used for paired dependent qualitative data. Bivariate Pearson correlation test was used to test the association between variables. Multiple linear regressions were used to test the association between quantitative dependent and independent variables and detection of risk factors. The P-value < 0.05 was considered statistically significant.
Results
We considered two groups in this work based on PSG findings: group I OSA patients (n = 153): 98 males (64.1%) and 55 females (35.9%), their age ranged from 16 to 83 years old with mean ± SD of 49.6 ± 13.1, their body mass index (BMI) ranged from 20 to 60.4 kg/m2 with mean ± SD 30.05 ± 8.9, STOP-Bang score mean ± SD 5.2 ± 1.1, ESS score with mean ± SD 17.4 ± 1.4. They were further subdivided according to AHI into mild OSA n = 57/153 (37.2%), moderate OSA n = 35/153 (22.9%), and severe OSA n = 61/153 (39.9%). While in group II non-OSA as the control group (n = 100): 66 males (66%) and 34 females (34%), their age ranged from 16 to 68 years old with mean ± SD 38.7 ± 10.2, their BMI ranged from 20.08 to 53.8 kg/m2 with mean ± SD 36.3 ± 8.7, STOP-Bang score mean ± SD 4.7 ± 1, ESS score mean ± SD 16.7 ± 1.1.
Regarding the comparison between OSA and control groups, OSA group showed a statistically significantly higher mean of age, STOP-Bang, ESS score, RDI, AHI, desaturation index, arrhythmia index, PLMI, wake index in addition to a significantly lower mean of total sleep time, sleep efficiency, minimal SpO2, and average SpO2. On the other hand, there was no statistically significant difference between the two groups regarding sex, BMI, total time in bed, baseline O2 saturation, and PLMs with arousal index.
There was a statistically significantly higher frequency of PLMS in the OSA vs control group (35.9% vs 14%).
Further comparison of study parameters in different AHI severity among OSA group (n = 153), severe group (n = 61) showed a statistically significantly higher mean of ESS score, RDI, and desaturation index while lower mean minimal SPO2 than mild and moderate groups.
When comparing the study parameters, there was a statistically significantly positive correlation between PLMI and each of OSA severity (AHI, hypopnea index), desaturation index, and PLMs with arousal index. In contrast, there was a statistically significantly negative correlation with BMI.
Multivariate logistic regression analyses were performed to predict the possible factors associated with the existence of PLMS among OSA; it was showed that apnea index and desaturation index were statistically significant predictors (Tables 1, 2, 3, 4, and 5).
Discussion
PLMS is usually coincidentally noted with OSA in PSG; however, few studies were conducted in this context.
The present study aimed to assess the prevalence of PLMS in different severity of OSAS and further detection of predictors of PLMS in OSA patients.
Previously by using PLMI ≥ 5 as clinically significant [9], studies showed that the prevalence of PLMS was 4–11% in adults [10]. Other studies showed a higher prevalence of PLMS in OSA (48%) in Canada [11] and (33%) in the USA [12], while Huang and Yu [13] showed a lower prevalence of PLMS in OSA (7.1%).
While the present study used PLMI cutoff of ≥ 15 as the PLMD criterion [2], it showed a statistically significantly higher frequency of PLM in the OSA group (n = 55/153) than in the control group (n = 14/100) (35.9% vs 14% respectively). Another study showed PLMS prevalence was 20.1% in OSA patients (n = 364) in China [14]. Similarly, a study done by Murase et al. [15] found a significantly higher prevalence of PLMS in the OSA-positive cohort (n = 46/254) than the OSA negative cohort (n = 8/88) (18.15 vs 9.1% respectively). In contrast, a study done by Huang and Yu [13] showed a lower prevalence of PLMS in OSA 0.8% (n = 3/378).
Different hypothesis to understand the association between PLMS and OSA, one possible hypothesis is through obesity as a risk factor for OSA and dysfunction of the dopaminergic pathway which is involved in the genesis of PLMS [16, 17]. This hypothesis is against our present study as it showed a statistically significantly negative correlation between PLMI and BMI among the OSA group. Similarly, a study done by Murase et al. [15] found that PLMS and OSA patients had lower BMI than those with OSA only.
Another hypothesis demonstrated that PLMS may occur together with subtle hypopneic events and episodes of increased upper airway resistance that might be identified by esophageal manometry as measuring respiratory effort-related arousals [4]. The present study in agreement with this hypothesis. Since esophageal manometry is impractical in our sleep center, we used RDI instead; it showed that OSA patients with PLM had non-significant higher mean RDI than non-PLM (37.2 ± 26.7 vs 33.3 ± 19.9 respectively). Also, the present study showed a statistically significantly positive correlation between PLMI and hypopnea index.
The present study found that OSAS patients with PLMS were older than OSAS patients without PLMS (non-statistically significant) (mean ± SD 50.5 ± 11.9 vs 49.1 ± 13.7 respectively).
This is agreed with facts that PLMS can be found normally in people over 40 years old [18]; others also found that the typical interval of PLMS changes with age; before the age of 55 and after age 65 years old, the interval was 24–28 s and 14–16 s respectively [19].
Similarly, other studies found that both age and PLMS were positively associated [20, 21].
Regarding gender, the present study found that sex was not considered a risk factor of PLMS among OSA patients similar to a study done by Zhou et al. [22].
While some researchers considered PLMS as PSG findings without functional significance [23], the present study pointed out that there was a statistically significantly positive correlation between PLMI and each of AHI, hypopnea index, desaturation index, and PLMs with arousal index. Also when multivariate logistic regression analyses were performed to predict the possible factors associated with the existence of PLMS among OSA, it was found that apnea index and desaturation index were statistically significant predictors.
Similar to our study, authors found that increase in PLMI was positively correlated with greater AHI [22, 24], while another study [25] proved the hypothesis that sleep apnea and PLMS are not generated by a common central generator and that the periodicity of PLMS was unlike that of OSA.
The present study found that nocturnal hypoxemia may be involved in the pathophysiology of PLMS. Similarly, a study performed by Ucar et al. [26] proved the hypothesis that hypoxia can also prompt PLMs in addition to other factors, e.g., anemia, chronic uremia, other metabolic disorders, and medications, although overnight lactate level has no effect on the occurrence of PLMS.
Regarding the kind of relationship between PLMS, arousal, and sympathetic over-activity, whether PLMS is part of the arousal process or causative of it is unclear. The present study found a statistically significantly positive correlation between PLMI and PLMs with arousal index, and when multivariate logistic regression analyses were performed PLMs with arousal index was considered as a predictor of the existence of PLM among OSA. The present study was in agreement with a different hypothesis: PLMS induces arousal and that PLMS may be considered one of the manifestations of generalized arousal during sleep [27].
A study done by Sforza et al. [28] supports the hypothesis that PLMS induces arousal; they found that PLMS are followed by autonomic activation, increase in HR, a significant increase in EEG activity, and subsequent arousal. Similarly, Winkelman [29] proposed the same hypothesis.
In contrast, other studies found that some form of cortical and autonomic activation starts before PLMS and that leg movements are considered a part of ongoing activation process. Ferri et al. [30] found an increase in both HR about 1 s and EEG power 7–8 s before the onset of PLMS. Similarly, Ferrillo et al. [31] found an increase in EEG activity before PLMS (about 3 s before for delta band activity and 1 s before for other EEG bands) and an increase in HR (about 4 s before PLMS).
Conclusion
The present study showed that OSA patients with PLM were older; had greater AHI, hypopnea index, desaturation index, and PLMs with arousal index; and had lower BMI. Larger multi-center studies are needed for better understanding this complex interaction. Further investigations are needed to identify and treat PLM of respiratory origin (RERA-induced PLMS) because agents used to treat PLMD, e.g., benzodiazepine, may cause exacerbation of sleep-disordered breathing.
Limitations
The present study did not investigate the effect of continuous positive airway pressure (CPAP) used in the treatment of OSA on PLMSI and other PSG variables.
Availability of data and materials
Not applicable.
Abbreviations
- PLMS:
-
Periodic limb movements during sleep
- OSAS:
-
Obstructive sleep apnea syndrome
- ESS:
-
Epworth Sleepiness
- PSG:
-
Polysomnography
- AHI:
-
Apnea hypopnea index
- PLMI:
-
Periodic limb movement index
- BMI:
-
Body mass index
- SBD:
-
Sleep breathing disorder
- SMD:
-
Sleep movement disorder
- URAS:
-
Upper airway resistance syndrome
- RERA:
-
Respiratory effort related arousal
- RDI:
-
Respiratory disturbance index
- ODI:
-
Oxygen desaturation index
References
Sateia MJ (2014) International classification of sleep disorders. Third edition Chest 146(5):1387–1394
American Academy of Sleep Medicine (2005) International classification of sleep disorders. Diagnostic and Coding Manual, 1st edn. American Academy of Sleep Medicine, Westchester
Young T, Palta M, Dempsey J et al (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl Med 328(17):1230–5
Exar EN, Collop NA (2001) The association of upper airway resistance with periodic limb movements. Sleep 24(2):188–192
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S et al (2008) STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 108(5):812–821
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Otero A, Felix P, Presedo J, Zamarron C (2012) An evaluation of indexes as support tools in the diagnosis of sleep apnea. Ann Biomed Eng 40(8):1825–1834
Chung F, Liao P, Elsaid H, Islam S, Shapiro CM, Sun Y (2012) Oxygen desaturation index from nocturnal oximetry: a sensitive and specific tool to detect sleep-disordered breathing in surgical patients. Anesth Analg 114(5):993–1000
Coleman RM, Pollak CP, Weitzman ED (1980) Periodic movements in sleep (nocturnal myoclonus):relation to sleep disorders. Ann Neuro 8(4):416–421
Hornyak M, Feige B, Riemann D, Voderholzer U (2006) Periodic leg movements in sleep and periodic limb movement disorder: prevalence, clinical significance and treatment. Sleep Med Rev 10(3):169–177
Al-Alawi A, Mulgrew A, Tench E, Ryan CF (2006) Prevalence, risk factors and impact on daytime sleepiness and hypertension of periodic leg movements with arousals in patients with obstructive sleep apnea. J Clin Sleep Med 2(3):281–7
Javaheri S, Abraham WT, Brown C, Nishiyama H, Giesting R, Wagoner LE (2004) Prevalence of obstructive sleep apnea and periodic limb movement in 45 subjects with heart transplantation. Eur Heart J 25(3):260–266
Huang CY, Yu CC (2019) Different diagnostic criteria for periodic leg movements in patients with obstructive sleep apnea after continuous positive airway pressure titration. Neuropsychiatr Dis Treat 15:2129–2136
Ren R, Huang G, Hang J et al (2016) Age and severity matched comparison of gender differences in the prevalence of periodic limb movements during sleep in patients with obstructive sleep apnea. Sleep Breath 20(2):821–7
Murase K, Hitomi T, Hamada S et al (2014) The additive impact of periodic limb movements during sleep on inflammation in patients with obstructive sleep apnea. Ann Am Thorac Soc 11(3):375–382
Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, Netusil N, Fowler JS (2001) Brain dopamine and obesity. Lancet 357(9253):354–357
Clemens S, Rye D, Hochman S (2006) Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology 67(1):125–130
Sforza E, Juony C, Ibanez V (2002) Time-dependent variation in cerebral and autonomic activity during periodic leg movements in sleep: implications for arousal mechanisms. Clin Neurophsiol 113(6):883–891
Ferri R, Manconi M, Lanuzza B et al (2008) Age-related changes in periodic limb movements during sleep in patients with restless legs syndrome. Sleep Med 9(7):790–798
Manconi M, Fanfulla F, Ferri R et al (2018) Periodic limb movements during sleep in stroke/TIA: prevalence, course, and cardiovascular burden. Neurology 90(19):1663–1672
Hermann W, Flemming T, Brandt M et al (2020) Asymmetry of periodic leg movements in sleep (PLMS) in Parkinson’s disease. J Parkinsons Dis 10(1):255–266
Zhou X, Zhou B, Li Z et al (2021) Periodic limb movements in patients with obstructive sleep apnea syndrome. Sci Rep 11(1):15341
Mahowald MW (2001) Con: assessment of periodic leg movements is not an essential component of overnight sleep study. Am J Resp Crit Care Med 164(8 pt 1):1340–1341
Baran AS, Richert AC, Douglass AB et al (2003) Change in periodic limb movement index during treatment of obstructive sleep apnea with continuous positive airway pressure. Sleep 26:717–720
Carelli G, Krieger J, Calvi-Gries F et al (1999) Periodic limb movements and obstructive sleep apneas before and after continuous positive airway pressure treatment. J Sleep Res 8(3):211–216
Uçar ZZ, Erbaycu AE, Taymaz Z et al (2010) Effect of hypoxia on periodic limb movement in sleep related breathing disorders. J Neurolo sci (TURKISH) 27(1):050–060
Sieminski M, Pyrzowski J, Partinen M (2017) Periodic limb movements in sleep are followed by increases in EEG activity, blood pressure, and heart rate during sleep. Sleep Breath 21(2):497–503
Sforza E, Nicolas A, Lavigne G et al (1999) EEG and cardiac activation during periodic leg movements in sleep: support for a hierarchy of arousal responses. Neurology 52(4):786–791
Winkelman W (1999) The evoked heart response to periodic leg movements of sleep. Sleep 22(5):575–580
Ferri R, Zucconi M, Rundo F et al (2007) Heart rate and spectral EEG changes accompanying periodic and non –periodic leg movements during sleep. Clin Neurophysiol 118(2):438–48
Ferrillo F, Beelke M, Canovaro P et al (2004) Changes in cerebral and autonomic activity heralding periodic limb movements in sleep. Sleep Med 5(4):407–412
Acknowledgements
The authors are grateful to the medical staff at the Department of Chest Diseases Mouwasat Hospital, Saudi Arabia, for their kind help and support throughout the study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization—R.I.A., M.S., and M.I.A. Methodology—M.S., R.H., R.I.A., and M.I.A. Writing—original draft preparation—M.S., R.H., S.A.A., M.M.A., R.I.A., and M.I.A. Writing—review and editing—M.S. and R.I.A. Statistical analysis and supervision—R.I.A., M.I.A., M.S., R.H., S.A.A., and M.M.A. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work was approved by the ethical committee following the ethical standards of the 1964 Helsinki Declaration and its later amendments.
Consent for publication
Approved by El-Mouwasat Hospital.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, R.I., Hendy, R.M., Ahmed, M.I. et al. Periodic limb movement index and severity of obstructive sleep apnea. Egypt J Bronchol 16, 35 (2022). https://doi.org/10.1186/s43168-022-00130-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-022-00130-0