Abstract
Background
Rotator cuff tendinopathy (RCT) is a leading cause of shoulder pain and disability. Management is mainly conservative, but the limited ability of tendons to regenerate is the main cause of unsatisfactory results. So, we conducted our study to compare the efficacy of deep prolotherapy (glucose 25%), platelet-rich plasma (PRP), and betamethasone corticosteroid for treatment of RCT to find the most effective one based on clinical, functional, and radiological assessment.
Results
Regarding visual analog scale (VAS), it was significantly (p < 0.001) improved after injection among group 1 (prolotherapy group) and group 3 (steroid group) patients, while no significant improvement was noted among group 2 (PRP group) (p = 0.212) patients. The Western Ontario Rotator Cuff (WORC) Index significantly improved among the studied groups (p < 0.001, p = 0.049, and p < 0.001, respectively) after injection. Regarding the range of motion (ROM), a significant improvement (p = 0.029) was achieved in group 1 after injection but no significant improvements were noted among group 2 and 3 patients (p = 0.529 and 0.121, respectively). There was a significant improvement among group 1 and 2 patients (p < 0.001 and p = 0.020, respectively) regarding the grade of tendon lesions but no improvement occurred among group 3 patients (p = 0.470).
Conclusion
Prolotherapy injections improve shoulder ROM, VAS, WORC index, and rotator cuff tendon healing while PRP injections improve WORC index and tendon healing but steroid injection has no effect on healing.
Trial registration
PACTR202005610509496. Retrospective registration on May 25, 2020, Pan African Clinical Trial Registry.
Similar content being viewed by others
Background
Rotator cuff tendinopathy (RCT) or rotator cuff disease (RCD) is a leading cause of shoulder pain and a significant source of disability and loss of work. It is a common disorder, and its prevalence increases with age and with occupations involving overhead activities [1].
Sometimes, tendon healing is unsatisfactory with the resultant tendinosis which progresses to partial tear then full-thickness tear. Histopathological study of chronic tendinopathy showed a disturbance in collagen fibers with increased vessel number and leukocyte count denoting inflammatory reaction in chronic tendinopathy [2]. RCT can be diagnosed by musculoskeletal ultrasound (MSUS) as it is rapid, inexpensive, non-invasive, has virtually no side effects and allows the rotator cuff to be visualized dynamically [3].
Management of RCD without full-thickness tear is mainly conservative in addition to physiotherapy, manipulation, and non-steroidal anti-inflammatory drugs (NSAIDs) which show a high rate of recurrence and persistent pain due to the limited ability of rotator cuff tendon to regenerate leading to chronic tendon disease [4].
Prolotherapy is the injection of an irritant agent, most commonly a hyperosmolar dextrose solution, at multiple painful entheses. It initiates an inflammatory cascade at the site of injection, which causes fibroblast proliferation with subsequent collagen synthesis resulting in a stronger tendon or ligament. Also, it may act as a central pain modulator [5].
It is known that healing is a highly complex biological process and various factors are required [1]. So, the potential for the use of platelet-rich plasma (PRP) is increased, which is a centrifuged blood product that contains a supra-physiologic amount of platelets, containing several cytokines and bioactive factors including basic fibroblast growth factor (FGF2), vascular endothelial growth factor, and transforming growth factor β (TGF). It is implicated in improving proliferation and collagen secretion of tenocytes promoting tendon cell growth and decrease oxidative stress which lead to cell apoptosis. Although it is easily applicable in conservative or augmentation of healing after surgical repair, studies were inconclusive [6].
Local corticosteroid injections are potent anti-inflammatory drugs improving local tissue metabolism with pain relief. Despite extensive research, the effectiveness of steroid injection in RCT is still questionable [7].
The aim of the present study was to compare the efficacy of ultrasound-guided injections of prolotherapy, platelet-rich plasma (PRP), and corticosteroids on the treatment of RCT based on clinical, functional, and radiological assessment.
Methods
This study was a randomized controlled prospective interventional study which adheres to CONSORT guidelines carried out on 60 patients with RCT selected over a period of 1 year. Inclusion criteria: patients diagnosed clinically with unilateral RCT with symptoms of at least 3 months after failed conservative treatment in the form of physical modalities and therapeutic exercises for at least 4 weeks. Patients were excluded from the study if they had the previous injection in the shoulder within the previous 3 months, history of shoulder trauma, instability, rotator cuff full-thickness tear, shoulder surgery, patients who were suffering from diabetes, rheumatic diseases, chronic liver disease, hematological diseases, tumors, metastatic diseases, their platelet value < 150,000 mm3, or on anticoagulation therapy.
All patients were subjected to the following: thorough history taking with especial emphasis on the mechanism of injury, overuse, or spontaneous onset and limited activities. Clinical examination mainly for active and passive range of motion (ROM) flexion, extension, abduction external, and internal rotation using a goniometer. Special Tests as Neer’s, Hawkins’, and drop arm tests were done. Pain severity was evaluated by visual analog scale (VAS) (0 to 10) where 0 means no pain and 10 indicates the worst pain. Western Ontario Rotator Cuff (WORC) Index: A disease-specific quality of life measurement tool for patients with rotator cuff disease comprised of 21 questions answered on 100-mm VAS items in 5 domains: physical symptoms, sports/recreation, work, lifestyle, and emotions. The total score is from 0 to 2100 as 0 implies no reduction in quality of life and 2100 is the worst score possible. The score can be reported as a percentage of normal by subtracting the total from 2100, dividing by 2100, and multiplying by 100 [8]. Radiological assessment by shoulder plain X-ray to exclude any bone disease or abnormality and diagnostic musculoskeletal ultrasound examination (MSUS) performed using General Electric (GE, Milwaukee, Wisconsin, USA) Logiq P5 R4.0 with a multi-frequency linear transducer probe 3–12 μHz to identify rotator cuff abnormalities as bursitis, tenosynovitis, tendinitis, tendinosis, partial tear (small or large one by measuring its dimensions), or full-thickness tear.
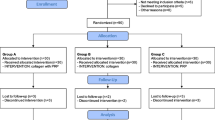
The patients were randomized by closed envelop method divided into three equal groups and each group received 2 ultrasound-guided injections with 2 weeks apart (Fig. 1).
Group 1: Twenty patients were injected with dextrose 25%: 10 ml (8 ml dextrose 25% and 2 ml lidocaine) to all the affected muscles and tendons.
Group 2: Twenty patients were injected with 5 ml PRP: 20 ml of venous blood mixed with 2 ml 10% sodium citrate then centrifuged at 1500 rpm for 15 min to create upper plasma layer, middle buffy coat layer, and a lower red blood cell layer. The upper and middle layers were collected in a sterile empty tube and re-centrifuged at 3500 rpm for 10 min resulting in the formation of a platelet plug and platelet-poor plasma. Platelet-poor plasma was withdrawn and discarded. The remaining PRP and platelet plug resulted in 5 ml PRP with a concentration of 6.7 times of whole blood ready for use [9].
Group 3 (control group): Twenty patients received an injection of 3 ml betamethasone and 2 ml local anesthetic (lidocaine).
Patients were instructed to limit their shoulder movements for 48 h after injection and to use acetaminophen for pain control if needed, but the use of NSAIDs was prohibited. Reassessment was done after 3 months by shoulder ROM, VAS for pain, WORC index, and diagnostic MSUS examination.
Statistical analysis
Statistical analysis was carried out using the Statistical Package for Social Sciences software version 23. The quantitative data were presented as ranges, and mean ± standard deviation and qualitative variables were presented as numbers and percentages. Regarding quantitative data, the comparison between paired groups was done by using paired t test, between more than two independent groups was done by using one-way ANOVA followed by post hoc analysis using the least significant difference (LSD) test and regarding qualitative data, and comparison between groups was done by using chi-square test and/or Fisher’s exact test when the expected count in any cell found less than 5. The confidence interval was set to 95%, and the margin of error accepted was set to 5%. So, the p value ≤ 0.05 was considered significant. The sample size 60 subjects (20 control on steroid therapy and 20 patients each group) was calculated by adjusting the power of the test to 80%, and the ratio between cases and controls was set to 2:1.
Results
This study was conducted on 60 patients with RCDs, their mean ages were 43.03 ± 12.17 years, and male to female ratio was 18:42 and dominant hand affection in 57 patients (95%) with 58% of them having occupations involving overhead activities. Regarding MSUS, 35 patients (58.33%) had partial tears, 19 (31.66%) with tendinosis, and 5 (8.33%) with tendinitis, bursitis, and bicipital tenosynovitis were detected in 38 (63.33%) and 24 (40%) of them respectively (Table 1).
Three months post-injection, there was a significant improvement (p = 0.029) in ROM of group 1 but no improvement was detected in group 2 or 3 (p = 0.529 and 0.121, respectively), with one of the patients in group 2 became worse and had ROM limitations in all directions (Table 2). Also, there was a significant improvement in VAS in group 1 and 3 (p < 0.001) but no improvement in group 2 (p = 0.212), while there was a significant improvement in all the 3 groups regarding WORC index (p < 0.001, 0.049, and p < 0.001, respectively) (Table 3).
Regarding ultrasound findings post-injection, there was a significant improvement in groups 1 and 2 (p < 0.001 and p = 0.020, respectively) in the grade of tendon lesions but no improvement occurred in group 3 (p = 0.470) with a significant difference (p < 0.000) between the 3 groups. Bursitis improved significantly in groups 1 and 3 (p < 0.001and p = 0.025, respectively), and no improvement was noticed in group 2 (p = 1.000). Also, bicipital tenosynovitis was improved in group 3 (p = 0.028) while no improvement was detected in groups 1 or 2 (p = 0.113 and 0.465, respectively) (Table 4). On comparing all the 3 groups to each other, post injection group 1 showed better results than groups 2 and 3 (Table 5, Figs. 2 and 3).
Discussion
In the current study, we compared ultrasound-guided injections of prolotherapy, corticosteroid, and PRP for the treatment of RCT.
We observed that group 1 patients achieved significant improvements (p = 0.029) in ROM and (p < 0.001) in other parameters used after prolotherapy injection. This agreed with Lee et al. [10], Seven et al. [5], and Huang [11] and Soliman et al. [12], which could be explained as hypertonic dextrose injection initiates a brief inflammatory cascade which in turn stimulates natural healing process with subsequent clinical improvement following the restoration of tissue integrity.
Also, by stimulating the production of multiple profibroblastic cytokines and glucose transport into human cells by glucose transporter (GLUT1) which is coupled with cytokine elevations and a direct pain-modulating effect either by downregulation of the transient receptor potential vanilloid type 1 (TRPV1) receptor, a chief receptor in maintenance of a chronic pain state, or by the effects on downstream mediators of TRPV1 activation [13].
Among group 2 patients, significant (p = 0.049 and p = 0.020) improvement of WORC index and tendon lesions, respectively, with no improvements noticed regarding other parameters used. This may be related to the beneficial effects of PRP on the healing process attributed to bone morphogenetic proteins, TGFs and FGFs [14], which proved to promote tendon cell proliferation, collagen synthesis, and vascularization in vitro and in vivo [15]. This agreed with Kesikburun and his colleague [1] and Carr et al. [16] who state that no difference in clinical outcomes in patients who received PRP injection for RCT compared to controls. Also, our results were in accordance with Rha et al. [17] who reported PRP injections revealed no improvement of shoulder ROM although provided more significant pain relief and improved arm function in patients with RCT or partial tear when compared to dry needling.
Our findings were contrary to Shams et al. [18] who demonstrated a statistically significant improvement in clinical outcomes 12 weeks after PRP injections but no difference after 24 weeks. Also, Ibrahim et al. [19] revealed a significant improvement in VAS, shoulder ROM, tear, and effusion but no improvement in tendinitis or bursitis 8 weeks after PRP injections.
A meta-analysis of PRP effect on surgical repair of rotator cuff tears by Warth et al. [20] indicated that there were no differences in clinical outcomes between patients who received PRP and those who did not, but it significantly lower the increased incidence of re-tear rates for large (> 3 cm) tear. However, Vavken et al. [21] found that PRP is effective in reducing re-tear rates in the arthroscopic repair of small- and medium-sized rotator cuff tears but no evidence that re-tear rates decreased for large and massive tears.
This could be explained by the substantial variability in the methods of PRP production among commercial systems [22]. Additionally, within a given PRP preparation protocol, there is a high degree of inter- and intra-subject variability in the PRP composition [23] which makes it difficult to assess the efficacy of PRP treatment for rotator cuff disease.
In group 3 in this study, there was a significant (p < 0.001, p < 0.001, p = 0.025, and p = 0.028) improvement of VAS, WORC index, bursitis, and bicipital tenosynovitis, respectively, but no improvement in shoulder ROM or tendon lesion.
Our findings were similar to Shams et al. [18] where there was an improvement of VAS, but MRI showed a slight nonsignificant improvement in the grades of tendinopathy/tear. Although, Ibrahim et al. [19] revealed that there was a significant improvement of pain and bursitis as our results, yet Shoulder Disability Questionnaire, ROM, and tendinitis were improved in contrary to ours. This could be explained by the analgesic effects of corticosteroid which may be mediated by neuropeptides, calcitonin gene-related peptide, and substance P which are found to increase in tendinopathies [24]. However, this should be balanced by their deleterious effects on the tendon tissue as collagen disorganization, decreased mechanical properties of the tendon, and long-term harm to the tendon tissue and cells [25].
In the present study, on comparing the dextrose prolotherapy to PRP versus steroid injection, we found significant results for the healing of tendon injuries for both dextrose prolotherapy and PRP, leading to decrease tear size up to complete healing for tendinosis and small partial tears which is due to their regenerative power, while non-significant change for steroid group. But for the effect on bursitis and tenosynovitis leading to improvement in pain, ROM, VAS, and WORC index, only prolotherapy having a significant effect which may be due to anti-inflammatory effect and pain modulation effect in addition to its regenerative power and to some extent steroids due to its anti-inflammatory effect.
Also, there was no side effects or difficulties related to prolotherapy injection except for pain with needle insertion, the same with PRP, but in addition to the extra cost added, while steroid has its usual side effects of the small amount released to bloodstream (as a transient increase in blood pressure or blood sugar) which was not significant in our study as we excluded diabetic and hypertensive patients.
The limitations in our study were the small sample size and the short term of follow-up period to demonstrate how long the effect will be maintained.
Conclusion
Prolotherapy injections improve shoulder ROM, VAS, WORC index, and rotator cuff tendon healing while PRP injections improve WORC index and tendon healing, but steroid injection has no effect on healing. Prolotherapy injection was superior to PRP and steroid in the treatment of RCT.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RCT:
-
Rotator cuff tendinopathy
- RCDs:
-
Rotator cuff diseases
- PRP:
-
Platelet-rich plasma
- ROM:
-
Range of motion
- VAS:
-
Visual analog scale
- WORC:
-
Western Ontario Rotator Cuff Index
- MSUS:
-
Musculoskeletal ultrasound
- ml:
-
Milliliter
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- FGF2:
-
Fibroblast growth factor
- TGF:
-
Transforming growth factor β
- LSD:
-
Least significant difference
- TRPV1:
-
Transient receptor potential vanilloid type 1 receptor
References
Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K (2013) Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med 41(11):2609–2616. https://doi.org/10.1177/0363546513496542
Dean BJ, Franklin SL, Murphy RJ, Javaid MK, Carr AJ (2014) Glucocorticoids induce specific ion-channel-mediated toxicity in human rotator cuff tendon: a mechanism underpinning the ultimately deleterious effect of steroid injection in tendinopathy? Br J Sports Med 48(22):1620–1626. https://doi.org/10.1136/bjsports-2013-093178
Plomb-Holmes C, Clavert P, Kolo F, Tay E, Lädermann A (2018) An orthopaedic surgeon’s guide to ultrasound imaging of the healthy, pathological and postoperative shoulder. Orthop Traumatol Surg Res 104(8S):S219–S232. https://doi.org/10.1016/j.otsr.2018.07.011
Chou WY, Ko JY, Wang FS, Huang CC, Wong T, Wang CJ et al (2010) Effect of sodium hyaluronate treatment on rotator cuff lesions without complete tears: a randomized, double-blind, placebo-controlled study. J Shoulder Elbow Surg 19(4):557–563. https://doi.org/10.1016/j.jse.2009.08.006
Seven MM, Ersen O, Akpancar S, Ozkan H, Turkkan S, Yıldız Y et al (2017) Effectiveness of prolotherapy in the treatment of chronic rotator cuff lesions. Orthop Traumatol Surg Res 103(3):427–433. https://doi.org/10.1016/j.otsr.2017.01.003
Lane JG, Healey RM, Chase DC, Amiel D (2013) Use of platelet-rich plasma to enhance tendon function and cellularity. Am J Orthop 42(5):209–214
Koester MC, Dunn WR, Kuhn JE, Spindler KP (2007) The efficacy of subacromial corticosteroid injection in the treatment of rotator cuff disease: a systematic review. J Am Acad Orthop Surg 15(1):3–11
Kirkley A, Alvarez C, Griffin S (2003) The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the western ontario rotator cuff index. Clin J Sport Med 13(2):84–92
Sweeny J, Grossman BJ (2002) Blood collection, storage and component preparation methods. In: Brecher M (ed) Technical Manual, 14th edn. American Association of Blood Banks (AABB), Bethesda MD, pp 955–958
Lee DH, Kwack KS, Rah UW, Yoon SH (2015) Prolotherapy for refractory rotator cuff disease: retrospective case-control study of 1-year follow-up. Arch Phys Med Rehabil 96(11):2027–2032. https://doi.org/10.1016/j.apmr.2015.07.011
Huang S (2018) Effects of hypertonic dextrose injection on chronic supraspinatus tendinopathy: a pilot study of randomized controlled trial. Ann Phys Rehabil Med 61S:e146. https://doi.org/10.1016/j.rehab.2018.05.326
Soliman DMI, Sherif NM, Omar OH, El Zohiery AK (2016) Healing effects of prolotherapy in treatment of knee osteoarthritis. Egypt rheumatol rehabil 43(2):47–52
Heilig CW, Deb DK, Abdul A, Riaz H, James LR, Salameh J et al (2013) Glut1 regulation of the pro-sclerotic mediators of diabetic nephropathy. Am J Nephrol 38(1):39–49. https://doi.org/10.1159/000351989
Cervellin M, De Girolamo L, Bait C, Denti M, Volpi P (2012) Autologous platelet-rich plasma gel to reduce donor-site morbidity after patellar tendon graft harvesting for anterior cruciate ligament reconstruction: a randomized, controlled clinical study. Knee Surg Sports Traumatol Arthrosc 20(1):114–120. https://doi.org/10.1007/s00167-011-1570-5
Heisterbach PE, Todorov A, Fluckiger R, Evans CH, Majewski M (2012) Effect of BMP-12, TGF-beta1 and autologous conditioned serum on growth factor expression in Achilles tendon healing. Knee Surg Sports Traumatol Arthrosc 20(10):1907–1914. https://doi.org/10.1007/s00167-011-1772-x
Carr AJ, Murphy R, Dakin SG, Rombach I, Wheway K, Watkins B et al (2015) Platelet-rich plasma injection with arthroscopic acromioplasty for chronic rotator cuff tendinopathy: a randomized controlled trial. Am J Sports Med 43(12):2891–2897. https://doi.org/10.1177/0363546515608485
Rha DW, Park GY, Kim YK, Kim MT, Lee SC (2013) Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil 27(2):113–122. https://doi.org/10.1177/0269215512448388
Shams A, El-Sayed M, Gamal O, Ewes W (2016) Subacromial injection of autologous platelet-rich plasma versus corticosteroid for the treatment of symptomatic partial rotator cuff tears. Eur J Orthop Surg Traumatol 26(8):837–842. https://doi.org/10.1007/s00590-016-1826-3
Ibrahim DH, El-Gazzar NM, El-Saadany HM, El-Khouly RM (2019) Ultrasound-guided injection of platelet rich plasma versus corticosteroid for treatment of rotator cuff tendinopathy: effect on shoulder pain, disability, range of motion and ultrasonographic findings. Egyptian Rheumatol 41:157–161. https://doi.org/10.1016/j.ejr.2018.06.004
Warth RJ, Dornan GJ, James EW, Horan MP, Millett PJ (2015) Clinical and structural outcomes after arthroscopic repair of full-thickness rotator cuff tears with and without platelet-rich product supplementation: a meta-analysis and meta-regression. Arthroscopy 31(2):306–320. https://doi.org/10.1016/j.arthro.2014.09.007
Vavken P, Sadoghi P, Palmer M, Rosso C, Mueller AM, Szoelloesy G et al (2015) Platelet-rich plasma reduces retear rates after arthroscopic repair of small- and medium-sized rotator cuff tears but is not cost-effective. Am J Sports Med 43(12):3071–3076. https://doi.org/10.1177/0363546515572777
Degen RM, Bernard JA, Oliver KS, Dines JS (2017) Commercial separation systems designed for preparation of platelet-rich plasma yield differences in cellular composition. HSS J 13(1):75–80. https://doi.org/10.1007/s11420-016-9519-3
Mazzocca AD, McCarthy MB, Chowaniec DM, Cote MP, Romeo AA, Bradley JP et al (2012) Platelet-rich plasma differs according to preparation method and human variability. J Bone Joint Surg Am 94(4):308–316. https://doi.org/10.2106/JBJS.K.00430
Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B (2013) Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. JAMA 309(5):461–469. https://doi.org/10.1001/jama.2013.129
Dean BJ, Lostis E, Oakley T, Rombach I, Morrey ME, Carr AJ (2014) The risks and benefits of glucocorticoid treatment for tendinopathy: a systematic review of the effects of local glucocorticoid on tendon. Semin Arthritis Rheum 43(4):570–576. https://doi.org/10.1016/j.semarthrit.2013.08.006
Acknowledgements
The authors acknowledged Prof. Dr. Neveen Fouda, Professor of Physical Medicine, Rheumatology and Rehabilitation, Faculty of Medicine – Ain Shams University, for her help in the ultrasonic assessment of the study.
Funding
No funding was received to this article.
Author information
Authors and Affiliations
Contributions
HMAS: Contribution to the conception and design of the work; the acquisition, analysis, and interpretation of data; and revision through a suggestion of the research idea and aim, clinical assessment of patients and controls, and preparation of the manuscript and statistical data. He also approved the submitted version and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work. MAN: Contribution to the design of the work; follow-up of patients, interpretation of data; and has drafted the work and substantively revised it. He also contributed to the preparation of the manuscript and statistical data, approved the submitted version, and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work. The authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ain Shams University, Faculty of Medicine Research Ethics Committee (REC) FWA 000017s8s. FMASU R41/2018.
A written informed consent was obtained from patients sharing in the study.
Consent for publication
A written consent was taken from the patients and available upon request.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sabaah, H.M., Nassif, M.A. What is better for rotator cuff tendinopathy: dextrose prolotherapy, platelet-rich plasma, or corticosteroid injections? A randomized controlled study. Egypt Rheumatol Rehabil 47, 40 (2020). https://doi.org/10.1186/s43166-020-00040-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-020-00040-3