Abstract
Background
To study the most common rheumatologic manifestations of hepatitis C viral (HCV) infection in Egyptian patients and associated risk factors with assessment the effect of current therapies on these manifestations. A prospective study was carried out to HCV patients attending the tropical medicine department referred to rheumatology department, over a year. A total of 204 hepatitis C virus treatment-naïve patients aged 21–71 years old suffering from rheumatologic manifestations were recruited, and history taking, general and musculoskeletal examination, laboratory and serological investigations, imaging, and liver fibrosis findings were assessed: baseline, end of treatment, and 12 weeks later, either sofosbuvir/ribavirin or sofosbuvir/simeprevir regimens and through three consecutive visits: joint activity and functional scores were taken.
Results
Common observed rheumatologic manifestations were fibromyalgia (74.5%), arthralgia (73.5%), Raynaud’s phenomenon (54.9%), peripheral neuropathy (29.4%),chronic fatigue syndrome and purpura (24.5%), arthritis (16.7%), Sicca symptoms and skin ulcers (9.8%), and vasculitic CNS involvement (5.9%), mostly seen in females. VAS and FAS scales have improved across visits (p value < 0.001) with lowered number and percentage of arthralgia (tender joint counts), arthritis (swollen joint counts), improvement of fibromyalgia, purpura, peripheral neuropathy, anemia, and thrombocytopenia (p < 0.001). Common reported risk factors were barber shaving (52 %), dental procedures (44.1%), and surgical interventions (36.3%). Non-reactive cases shown by HCV-PCR response increased at the end of study reaching 62%. The percent of improvement was significantly higher in patients receiving sofosbuvir/simeprevir regimen (100%) versus sofosbuvir/ribavirin (58.2%).
Conclusion
Direct antiviral drugs seem to improve the rheumatic extra-hepatic manifestations of HCV patients and lowering viremia level especially sofosbuvir/simeprevir regimen in hepatitis C treatment-naïve patients.
Similar content being viewed by others
Background
Hepatitis C virus (HCV) is known to affect the patients’ health-related quality of life compared to the controls [1]. There is a decrease in functional ability, reduced daily activities, and cost burdens, as well. Improvement in health-related quality of life is maintained and kept up with better viral control [2]. It was found that 45 to 85% of HCV-infected individuals are still unaware of their status [3]. Mortality rates were estimated to be three times higher than those in the general population and that each year, more than three hundred and fifty thousand patients die from HCV-related liver diseases [4, 5]. It was shown that HCV infection was associated not only with death from hepatic but also from extra-hepatic diseases [6]. This seemed to be a significant endemic medical issue in Egypt: an Egyptian demographic health survey done in 2008 from both urban and rural areas has demonstrated that 14.7% of the population has been infected, making this the highest prevalence in any population in the world [7,8,9]. It was found that the Nile Delta and Upper Egypt infection rates of HCV are 26% and 28%, respectively. Every year, incidence rates range between 2 and 6 per 1000, thus an estimation of 170,000 new cases every year in addition to the 11.5 million patients suffering from the HCV [10]. HCV viremia may provoke non-specific rheumatologic manifestations described as extra-hepatic ones [11]; non-specific serological abnormalities can occur and/or manifested clinical disease, affecting multiple organs and systems [12].
In Egypt, one of the virus highest world prevalence of 13.9–15.5% (14.7%) [13], a nucleic acid test that is positive in 7.0–12.2% (9.8) [14], genotype-4 (GT-4) was found in 90% of patients, which is typically difficult to treat [15].
Direct-acting antiviral drugs (DAAs) use for HCV treatment with research efforts going on intensively have resulted in the development of HCV sub-genomic replicons and are capable of autonomous replication [16] and cell culture models for HCV infection [17] resulting in screening assays identifying specific antiviral targets [18].
The aim of this study is to detect the most common rheumatologic manifestations of hepatitis C viral infection in newly diagnosed (treatment-naïve) Egyptian patients and their associated risk factors and assessment of current therapies of direct acting anti-virals on these manifestations.
Methods
Study design and setting
A prospective study was conducted over a year. The patients were referred from Tropical medicine and Hepatology outpatient clinic to Rheumatology and rehabilitation outpatient clinic, Faculty of Medicine.
Patients
Two hundred and four newly diagnosed hepatitis C treatment-naïve patients, who have never taken any antiviral therapy before, 100 males (49%) and 104 females (51%), were prospectively examined for HCV infection by ELISA and quantitative PCR test, over a period of a year, through history taking and general and musculoskeletal examination. Screening for extra-hepatic rheumatologic manifestations (fibromyalgia, arthralgia, arthritis, peripheral neuropathy, sicca symptoms, Raynaud’s phenomenon, purpura, skin ulcers, vasculitic CNS involvement, cryogloblulinemia, chronic fatigue syndrome) visual analog scale of pain (VAS) [19], and fatigue activity scale (FAS) [20] was taken across three consecutive visits (baseline, 12 weeks later, then 12 weeks after second visit).
Inclusion criteria
HCV treatment- naïve patients who never took an antiviral treatment for hepatitis C before were included, and the most discovered and associated important risk factors causing those prone subjects to be infected were asked to be included in this study.
Exclusion criteria
Patients presented with decompensated cirrhosis or organ transplants or malignancies were excluded. Patients positive for HCV Ab and negative by qualitative PCR test or patients co-infected with human immune deficiency virus or hepatitis B virus were also excluded. Exclusion of other autoimmune diseases (RA, SLE, primary Sjogren syndrome, other forms of vasculitis), mechanical or degenerative causes, lymphoproliferative and myeloproliferative disorders, and endocrinal causes is like thyroid dysfunction.
Laboratory investigations
Blood specimens were collected after an overnight fasting analyzed for complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), serum transaminases (AST, ALT), serum bilirubin, liver and kidney function tests were considered, prothrombin concentration and international normalized ratio, oral glucose tolerance test, and complete urine analysis. Serologically, rheumatoid factor (RF) was assayed with a quantitative immunonephelometry test, antinuclear antibodies (ANA), serum complement 3 (C3) and complement 4 (C4), cryoglobulin profile, anti-neutrophil cytoplasmic antibodies (ANCA), anti-thyroid antibodies (Anti-TPO and anti-TG antibodies), quantitative HCV-polymerase chain reaction to detect viral load (above 800.000 means high viremia, from 100.00 to less than 800.000 means moderate viremia, from 1000 to less than 100.000 means mild viremia, and less than 1000 means negative from viremia or the non-reactive stage), the bilharzial antibodies, and alpha-feto-protein.
Imaging studies
Plain radiographs of both hands and chest radiographs, abdominal ultrasonography (US), and assessing liver fibrosis by liver biopsy or fibroscan.
Sample size calculation
Sample size was calculated using a special formula based on the reported prevalence of rheumatologic extra-hepatic manifestations in HCV patients 17%, with 95% confidence interval, precision of 5%, population size 1000 available during study period to be 179. Finally, sample was increased by 10% to overcome non-response [21].
Selected protocols
Selected direct-acting antiviral therapy (DAA) combinations in this section were done according to their availability in Egypt. The two protocols were mainly sofosbuvir (NS5B inhibitor)-based.
Protocol A: sofosbuvir (NS5B inhibitor)-based protocols on 182 patients: sofosbuvir (400 mg) and weight-based ribavirin (RBV) (1000 mg [< 75 kg] to 1200 mg [> 75 kg]) for 12 weeks [22].
Protocol B: simeprevir (NS3/4A-inhibitor) + sofosbuvir (NS5B) inhibitor-based protocols on twenty two patients: simeprevir (150 mg) and sofosbuvir (400 mg) for 12 weeks [23].
Statistical analysis
Data was collected, coded, and analyzed using the Statistical Package for Social Science (SPSS) software version 16. A descriptive analysis in the form of means and standard deviations was calculated for numerical data, number, and percent for qualitative data, comparing between groups that was done using (chi-square) test for qualitative data. Comparison to investigations across visits was done (paired t test) for two reading and repeated measure ANOVA for more than two readings for testing all quantitative variables for normal distribution. The level of statistical significance was ≤ 0.05.
Results
Two hundred and four newly diagnosed (treatment-naïve) hepatitis C patients were investigated for extra-hepatic rheumatic manifestations: 100 (49.0%) were males, and the 104 (51.0%) were females. The mean age of patients with rheumatic manifestations was 48.11 ± 12.65, and the age group of the patient in this study range from 21 to 71 years. Majority of the patients were non-educated, and the mean disease duration of hepatitis C virus (HCV) was 2.46 ± 1.86.years (Table 1).
The most common risk factors associated with the hepatitis C virus (HCV) transmission were barber shaving (52%), dental procedures (44.1%), and surgical procedures (36.3%). Moreover, surgery, bilharzial treatment, tattooing, and Hegama were significantly more seen in male than female patients (Table 1).
The most common observed extra-hepatic rheumatologic manifestations of HCV-positive patients were fibromyalgia 152 (74.5%), arthralgia 150 (73.5%), raynaud’s phenomenon 112 (54.9%), peripheral neuropathy 60 (29.4%), chronic fatigue syndrome 50 (24.5%), purpura 50 (24.5%), arthritis 36 (16.7%), sicca symptoms 20 (9.8%), skin ulcers 20 (9.8%), and vasculitic CNS involvement 12 (5.9%), respectively. Most of these manifestations were significantly more seen in females than males (Table 2).
During the study period, we assessed the extra-hepatic rheumatologic manifestations across the three visits, and it was detected: lowered number and percentage of arthralgia (tender joint counts) 150 (73.5%), 80 (39.2%), and 40 (19.6%); arthritis (swollen joint counts) 36 (16.7%), 20 (9.8%), and 16 (7.8%); fibromyalgia syndrome 152 (74.5%), 86 (42.2%), and 50 (24.5%); purpura 50 (24.5%), 6 (3.0%), and 4 (2.0%); peripheral neuropathy 60 (29.4%), 56 (27.4%), and 40 (19.6%); also laboratory investigations anemia 28 (13.7%), 26 (12.8%), and 12 (5.9%); and thrombocytopenia 51 (25.0%), 7 (3.4%), and 4 (2.0%) (p < 0.001) (Table 3).
By forward stepwise regression analysis to detect risk factors of the most common rheumatic manifestations, young age, having diabetes and hypertension, low C3, positive rheumatoid factor, and high HCV-PCR titer were documented risk factors of arthritis. Regarding arthralgia, female sex and high HCV-PCR titer were reported risk factors. High HCV-PCR titer was also a reported risk factor in fibromyalgia, where HCV-PCR was measured before the start of the antiviral treatment, 12 weeks at end of treatment course, and a third time 12 weeks later to document non recurrence of the virus (Table 4).
During the study period, we compared the visual analog scale (VAS) of pain and fatigue activity scale (FAS) through three consecutive visits and observed significant decreases of mean scores across visits ( p value < 0.001) (Table 5).
A significant difference of laboratory investigations readings across time visits for PLT, WBCS, ALT, AST, albumin, and creatinine (Table 6).
Regarding rheumatologic manifestations, percentage of patients with low C3 (21.6%, 19.6%, 2.9%), low C4 (7.8%, 2.9%, 2.9%), and positive RF (42.2%, 32.4%, 18.6%) decreased significantly across the three visits (Fig. 1).
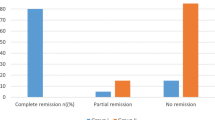
By comparing between the two regimens regarding response to treatment, all patients who received sofosbuvir/simeprevir regimen have improved at the end of treatment 22 (100%) versus 106 (58.2%) who received sofosbuvir/ribavirin regimen, where 76 (41.8%) patients receiving sofosbuvir/ribavirin did not improve from the 182 patients who took this regimen.
Regarding the adverse effects of the treatment, the most side effects were reported with sofosbuvir/ribavirin in 102 patients (56%) in the form of GIT upset in 44 patients (24%) and skin manifestations in the form of skin rash and photosensitivity in 14 patients (7.7%). Both GIT upset with skin manifestations were reported in 22 patients (12%), and no reported side effects with sofosbuvir/simeprevir regimen (Table 7).
Discussion
A high prevalence of rheumatologic extra-hepatic manifestations of hepatitis C virus among Egyptians has been documented [21]. In this study, we observed the effect of combined direct antiviral therapy on newly diagnosed (treatment-naïve) hepatitis C patients and its effects on their extra-hepatic manifestations. Direct-acting antivirals (DAAs) are medications having specific targets. The four classes are nonstructural proteins: 3/4A (NS3/4A) protease inhibitors (PIs), NS5A inhibitors, NS5B nucleoside polymerase inhibitors (NPIs), and NS5B non-nucleoside polymerase inhibitors (NNPIs). The four classes of DAAs target specific nonstructural proteins of the HCV life cycle, resulting in disruption of viral replication and infection [18].
Patients in this study showed significant improvement that lowered number and percentage of arthralgia (tender joint counts) 150 (73.5%), 80 (39.2%), and 40 (19.6%); arthritis (swollen joint counts) 36 (16.7%), 20 (9.8%), and 16 (7.8%); fibromyalgia syndrome 152 (74.5%); 86 (42.2%), and 50 (24.5%); purpura 50 (24.5%), 6 (3.0%), and 4 (2.0%); peripheral neuropathy 60 (29.4%), 56 (27.4%), and 40 (19.6%); also laboratory investigations anemia 28 (13.7%), 26 (12.8%), and 12 (5.9%); and thrombocytopenia 51 (25.0%), 7 (3.4%), and 4 (2.0%) (p < 0.001) after direct antiviral therapy, in which 106 (58.2%) of the patients improved after combined therapy by (sofosbuvir/ribavarin), and 22 (100.0%) improved after combined therapy by (sofosbuvir/simeprevir) with a total 62.7% improvement after treatment with comparison done shown during assessment when compared baseline and after treatment at week 24.
Similar results to an Egyptian research which treated newly diagnosed (treatment-naïve) patients who never took an anti-viral therapy before to take a direct acting therapy as their initial medication and treatment-experienced patients with genotype-4 HCV infections with sofosbuvir 400 mg/ribavirin 1000–1200 mg daily for 12 or 24 weeks, and rates were 90% (46/51) with 24 weeks and 77% (40/52) with 12 weeks of sofosbuvir and ribavirin therapy [22]. This may reflect the idea that the longer the duration of the therapy, the higher the percentage of improvement.
Ruane and colleagues [24] have demonstrated that the interferon-free therapy with sofosbuvir/ribavirin achieved a sustained virological response (SVR) of 100% in treatment-naïve for 24 weeks; in this current study, HCV-PCR was measured before start of the antiviral treatment, 12 weeks at end of treatment course, and a third time 12 weeks later to document non recurrence of the virus following sofosbuvir-based antiviral therapy detecting less than 1000 signifies non-reactive in 62% of patients whereas the combination of sofosbuvir/ledipasvir for 12 weeks resulted in sustained virological response (SVR) of 95% [24]. In another study using a combination of sofosbuvir (an NS5B inhibitor) and ribavirin for 12 to 24 weeks, with a SVR of 68–90% [25], the effect of using sofosbuvir/simeprevir was inconsistent with phase III PLUTO clinical trial, with high SVR 12 rate to patients receiving the same combination [26] and nearly same results in a previous study done by EL-Khayat and co-workers [27]. These two clinical trials may highlight the efficacy of the regimen using sofosbuvir/simeprevir in particular.
The most common observed rheumatologic manifestations in this study were fibromyalgia (74.5%), arthralgia (73.5%), and peripheral neuropathy (29.4%) that were more seen in females than in males. Observed significant mean visual analog scale (VAS) and mean fatigue activity score (FAS) across visits reported (p value <0.001) to all patients who received sofosbuvir/simeprevir regimen and 58.2% of patients who received sofosbuvir/ribavirin regimen across different visits. Similar results have shown that mean of FAS scale and VAS scale decreased significantly across follow-up visits in patients using SOF-based antiviral combinations mainly sofosbuvir/simeprevir regimen [28]. Also, a study done in 2016 showed that treated mixed cryoglobulinemic (MCS) patients with interferon-free, DAA-based therapy reported improvement in clinical parameters in all the patients with mixed cryoglobuniamia with 100% SVR12 and SVR24 by using different SOF-based antiviral combinations, resulting in a high antiviral efficacy of these drugs [29]. A small number of patients in this current study were found to have cryoglobinemia, and our results did not demonstrate a significant effect of the therapy on cryoglobulinemia. Another study done in Egypt 2017 on HCV patients was associated with arthropathy treated with combination therapy that consists of sofosbuvir, daclatasvir, and ribavirin and has shown marked improvement of manifestations of arthropathy in hepatitis C patients after treatment [30].
On the contrary, relapse was documented in few patients with vasculitis, who previously achieved a sustained virologic response (SVR) [31]. After interferon-free antiviral therapy was given, persistence of vasculitis was detected [32].
As reported above in this study, RF levels decreased from 42.2 to 18.6%, and low complement 3 (C3) was detected in first visit in 22% and reached to be detected into 3% of the patients with normalization across visits after antiviral treatment.These results are nearly similar to a study done in 2017 that had shown the safety and efficacy of direct-acting antiviral agents (DAAs) in treating HCV extra-hepatic manifestations, and a complete response was obtained in 77.3% of patients receiving direct-acting antiviral agents and RF levels normalized in 50% and C4 in 63.6% of the patients [33]. Although, rheumatoid factor is non-specific but included as one of the serological investigations of extra-hepatic viral C infection. When repeated in the follow-up evaluation, some patients who were having positive serology of this test have changed to be negative later on, with a significant decrease in their next visits after taking direct acting antiviral medications in the two protocol regimens.
In this study, sicca symptoms were detected in 9.8%, and arthritis was found in 16.7% patients only. A study done in 2017 has detected the prevalence of Sjögren syndrome in patients with HCV is less than 5% while arthritis being a rheumatic manifestation of HCV occurred in less than 10% of patients [34].
In the current study, a remarkable improvement of the clinical manifestations was observed during administration of DAAs, although symptoms persisted or worsened in 6 (3.3%) with sofosbuvir/ribavirin regimen but not with sofosbuvir/simeprevir regimen. An Egyptian study has shown the superiority of sofosbuvir-based antiviral therapy over pegylated interferon/ribavirin with marked SVR12 (100%) and lesser side effects [28]. On the other hand, a study had showed that (67%) of patients experiencing at least one adverse event during therapy based mainly on ribavirin containing regimen [35].
In the current research work, the most common risk factors triggering disease development in hepatitis C virus (HCV) transmission were having barber shaving, dental procedures (44.1%), and surgery procedures (36.3%), respectively. Surgery, bilharzial treatment, tattooing, and Hegama were significantly more seen in male than female patients. Most detected risk factors were found in systematic reviews that were in seven of the nine studies: surgery was reported to be significant. Also, blood transfusion, age, and hospitalization which were examined in 64–82% of total studies (n = 11). Five articles examined familial transmission in (45%), dental procedure in four articles (36%), and schistosomiasis or bilharziasis treatment and mother’s HCV status in three articles (27%). Almost 80% (79.2%; n = 42) of the risk factors assessed was found to be statistically associated with HCV infection, thus HCV prevention and early eradication is becoming a priority [36].
Accordingly, a proper assessment of modifiable risk factors of the disease, importance of proper health education, and the new interventions of preventive measures, targeting the whole community, can result in better outcomes.
Conclusions
The new era of using direct antiviral drugs seems to improve the rheumatologic extra-hepatic manifestations of hepatitis C viral infected patients. Thus, early interventions are needed especially, in newly diagnosed patients with HCV.
We recommend using direct anti-viral treatment and expanding the health education of modifiable risk factors which will aid in preventing re-infection once more and thus improving the quality of life in this community. Also, it is recommended in the future studies to consider more number of patients, which may help to verify our results.
Availability of data and materials
An availability of all datasets used and/or analyzed during this study were granted with raw data available on asking on private bases and will be available on open request.
Abbreviations
- HCV:
-
Hepatitis C virus
- DAAs:
-
Direct acting antivirals
References
Bonkovsky H, Snown K, Malet P, Back-Madruga C, Fontana R, Sterling R, HALT-C Trial Group (2007) Health- related quality of life in patients with chronic hepatitis C and advanced fibrosis. J Hepatol 46:420–431
Cacoub P, Ratziu V, Myers R, Ghillani P, Piette J, Moussalli J (2002) Multivirc group. Impact of treatment on extra hepatic manifestations in patients with chronic hepatitis C. J Hepatol 36:812–818
Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Teo CG et al (2012) Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945–1965. MMWR Recomm Rep 61:1–32
Neal KR, Ramsay S, Thomson BJ, Irving WL (2007) Excess mortality rates in a cohort of patients infected with the hepatitis C virus: a prospective study. Gut 56:1098–1104
Lavanchy D (2009) The global burden of hepatitis C. Liver Int 29(Suppl 1):74–81
Lee MH, Yang HI, Lu SN, Jen CL, You SL, Wang LY et al (2012) Chronic hepatitis C virus infection increases mortality from hepatic and extrahepatic diseases: a community-based long-term prospective study. J Infect Dis 206:469–477
Frank C, Mohamed M, Strickland GT (2000) The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet 355(9207):887–891
Shepard CW, Finelli L, Alter MJ (2005) Global epidemiology of hepatitis C virus infection. Lancet Infect Dis 5(9):558–567
El-Zanaty F, Way A. Egypt Demographic and Health Survey 2008. Cairo, Egypt. Ministry of Health, El-Zanaty and Associates, and Macro International; 2009:431.
Wanis H. HCV treatment in Egypt – why cost remains a challenge? Cairo, Egypt: Egyptian initiative for personal rights [serial on the Internet]; 2014:1–4. Availablefrom:http://www.eipr.org/sites/default/files/pressreleases/pdf/hcv_treatment_in_egypt.pdf. Accessed 16 June 2016.
Sterling RK, Bralow S (2006) Extra-hepatic manifestations of hepatitis C. Curr Gastroenterolo Rep 8(1):53–59
Galossi A, Guarisco R, Bellis L, Puoti C (2007) Extrahepatic manifestations of chronic HCV infection. J Gastointestin Liver Dis 16(1):65–73
Cuadros DF, Branscum AJ, Miller FD, Abu-Raddad LJ (2014) Spatial epidemiology of hepatitis C virus infection in Egypt: analyses and implications. Hepatology 60:1150–1159
Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi HGJ (2014) Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol 61(1 Suppl):S45–S57
Kamal SM, Nasser IA (2008) Hepatitis C genotype 4: what we know and what we don’t yet know. Hepatology 47:1371–1383
Lohmann V, Körner F, Koch J, Herian U, Theilmann L, Bartenschlager R (1999) Replication of subgenomic hepatitis C virus RNAs in a hepatoma cell line. Science 285:110–113
Lindenbach BD, Evans MJ, Syder AJ, Wölk B, Tellinghuisen TL, Liu CC, Maruyama T, Hynes RO, Burton DR, McKeating JA, Rice CM (2005) Complete replication of hepatitis C virus in cell culture. Science 309:623–632
Barth HW (2015) J Hepatology 7(5):725–737
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain. Arthritis Care Res 63(11):S240–S252
Michielsen HJ, De Vries J, Van Heck GL (2003) Psychometric qualities of a brief self-rated fatigue measure: the fatigue assessment scale. J Psychosom Res 54(4):345–352
Mohammed RH, El Makhzangy HI, Gamal A, Mekky F, El Kassas M, Mohammed N et al (2010) Prevalence of rheumatologic manifestations of chronic hepatitis C virus infection among Egyptians. Clin Rhematol 29(4):1373–1380
Doss W, Shiha G, Hassany M, Soliman R, Fouad R, Khairy M et al (2015) Sofosbuvir plus ribavirin for treating Egyptian patients with hepatitis C genotype 4. J Hepatol 63(3):581–585
Lawitz E, Matusow G, DeJesus E, Yoshida E, Felizarta F, Ghalib R (2015) LP04: a phase 3, open-label, single-arm study to evaluate the efficacy and safety of 12 weeks of simeprevir (SMV) plus sofosbuvir (SOF) in treatment-naive or-experienced patients with chronic HCV genotype 1 infection and cirrhosis: Optimist-2. J Hepatol 62:S264
Ruane PJ, Ain D, Stryker R, Meshrekey R, Soliman M, Wolfe PR et al (2015) Sofosbuvir plus ribavirin for the treatment of chronic genotype 4 hepatitis C virus infection in patients of Egyptian ancestry. J Hepatol 62(5):1040–1046
Foster GR, Pianko S, Brown A, Forton D, Nahass RG, George J (2015) Et al, Efficacy of Sofosbuvir plus ribavirin with or without peg-interferon in patient with HCV genotype 3 infection and treatment-experienced patients with cirrhosis and HCV genotype 2 infection. Gastroenterology 149:1462–1470
Buti M, Calleja JL, Lens S, Diago M, Ortega E, Crespo J et al (2017) Simeprevir in combination with sofosbuvir in treatment naïve and experienced patients with hepatitis C virus genotype 4 infection: a phase III, open- label, single arm study (PLUTO). Alimen Pharmacol Ther 45(3):468–475
El-Khayat HR, Foud YM, Maher M, El-Amin H, Muhammed H. Efficacy and safety of sofosbuvir plus simiprevir therapy in Egyptian patients with chronic hepatitis C: a real- world experience. Gut 2016; 0:1-5.
Shahin AA, Zayed HS, Said M, Amer SA (2018) Efficacy and safety of sofosbuvir –based, interferon-free therapy: the management of rheumatic extrahepatic manifestations associated with chronic hepatitis C infection. Z Rheumatol 77(7):621–628
Gragnani L, Visentini M, Fognani E, Urraro T, De Santis A, Petraccia L et al (2016) Prospective study of guideline-tailored therapy with direct-acting antivirals for hepatitis C virus-associated mixed cryoglobulinemia. Hepatology. 64:1473–1482
Yasmin Abdl AMT. Effects of Direct Antiviral Agents on Hepatitis C Virus Arthropathy. Clinical Trials.gov July, 2017; 24-26.
Landau A, SaadounD HP (2008) Relapse of hepatitis C virus-associated mixed cryoglobulinemiavasculitis in patients with sustained viral response. Arthritis Rheum 58:604–611
Sollima S, Milazzo L, Peri AM, Torre A, Antinori S, Galli M (2016) Persistent mixed cryoglobulinaemia vasculitis despite hepatitis C virus eradication after interferon-free antiviral therapy. Rheumatology (Oxford) 55:2084–2085
Lauletta G, Russi S, Pavone F, Vacca A, Dammacco F (2017) Direct-acting antiviral agents in the therapy of hepatitis C virus-related mixed cryoglobulinaemia: a single-Centre experience. Arthritis Res Ther 19:74. https://doi.org/10.1186/s13075-017-1280-16
Cacoub P, Commarmond C, Sadoun D, Desbois AC (2017) Hepatitis C virus infection and rheumatic diseases: the impact of direct-acting antiviral agents. Rheum Dis Clin N Am 43(1):123–132
Sise ME, Bloom AK, Wisocky J, Lin MV, Gustafson JL, Lundquist AL, Steele D, Thiim M, Williams WW, Hashemi N, Kim AY, Thadhani R, Chung RT (2016) Treatment of hepatitis C virus–associated mixed Cryoglobulinemia with direct-acting antiviral agents. Hepatol. 63(2):408–417
Mahmoud YA, Mumtaz GR, Riome S, Miller DW, Abu-Raddad LJ (2013) The epidemiology of hepatitis C virus in Egypt: a systematic review and data synthesis. BMC Infect Dis 13:288–292
Acknowledgements
We are grateful to the patients for their participation in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptions. Constructing an idea or hypothesis for research and/or manuscript: SS. Design: HF. Planning methodology to reach the conclusion: HF and SS. Supervision: organizing and supervising the course of the project or the article and taking the responsibility: AG, S S, HF, and EHA. Fundings: no funding sources. Data collection and/or processing. Taking responsibility in execution of the experiments, patient follow-up, data management, and reporting: HF, SS, AG, EHA, and FA. Analysis and/or interpretation. Taking responsibility in logical interpretation and presentation of the results: HF, WAW, and HE. Literature review. Taking responsibility in this necessary function: All authors. Writer. Taking responsibility in the construction of the whole or body of the manuscript: All authors. Critical review for spelling or grammar mistakes and for intellectual contents: HF. All authors have read and approved the manuscript and ensured that this is the case.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current research has been approved by the Local Ethical Committee, Faculty of medicine, Fayoum University, R29 8th session on 23 November 2014. A written informed consent was obtained from educated patients, while detailed explanation about the study aims to those non-educated patients followed by their oral consent and approval for research publication and was enrolled in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fathi, H.M., Abdel Wahed, W.Y., Gomaa, A.A. et al. A prospective study in hepatitis C virus treatment-naïve patients showing rheumatologic extra-hepatic manifestations of hepatitis C with associated risk factors: efficacy and safety using sofosbuvir-based direct antiviral therapy. Egypt Rheumatol Rehabil 47, 20 (2020). https://doi.org/10.1186/s43166-020-00023-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-020-00023-4