Abstract
Background
The standard methods for diagnosing otosclerosis (OS) include clinical and audiological testing. Radiologic imaging continues to expand with use in diagnosis, staging, surgery planning, and outcomes.
Objective
To determine if high resolution computed tomography (HRCT) imaging advances to the audiological findings in the diagnosis of otosclerosis.
Methods
This prospective randomized controlled study was conducted from June 2018 to June 2022. Fifty patients with OS who divided into two subgroups: group 2a, 50 early OS ears, and group 2b, 35 ears with late OS. The controls includes 50 individuals who have healthy ears (group 1). All participants had otorhinolaryngology examination, audiological evaluation and HRCT imaging.
Results
Early OS had higher air conduction thresholds than control, and late OS had considerably higher air conduction thresholds than either the early or control subjects (p < 0.001). Early OS patients had higher bone conduction threshold (BCT) than control, while late OS patients had higher BCT than both early and control subjects (p < 0.001). In early and late OS, there is a significant association between bone conduction of 11 dB and 21.6 dB, respectively (P = 0.004), and a significant air–bone gap of 25.5 and 31 dB, respectively (P = 0.03). HRCT showed a sensitivity of 75% and high specificity 92% with accuracy 83% in early OS and sensitivity of 78% and high specificity 94% with accuracy 86% in late OS.
Conclusion
HRCT is a more sensitive and specific diagnostic tool for OS than audiometry. HRCT could discriminate between early and late OS, suggesting that it can be used to do so with a high degree of confidence.
Similar content being viewed by others
Background
OS is a unique otic capsule otodystrophy that is autosomal dominant. Because spongy vascular bone replaces the typical ivory-like enchondral bone, it is also known as "otospongiosis."Patients typically present in their second or fourth decades of life with any type of hearing loss with/without tinnitus. OS affects white people 0.3%–0.4% more frequently than it does black people. Females are more likely than males to have bilateral (85%) OS [1].
The diagnosis is frequently made using audiometric results and clinical suspicion [2]. The stapedotomy operation, which entails the creation of window at stapes footplate and installation of a prosthesis that replaces the stapes, is presently thought to be the standard surgical technique in the literature that have high success rates [3,4,5].
Diagnosis, grading, surgical planning, complications, and results are the goals of increasingly performed radiological imaging when handled properly, and temporal bone HRCT is the preferred imaging approach [6, 7]. There have also been suggested applications for single photon emission computed tomography, magnetic resonance imaging, and cone beam computed tomography. Therefore, typical patients do not always obtain imaging, and the clinical usefulness of imaging is yet uncertain [8, 9].
It is known that fine-cut CT scans show evidence of otosclerotic foci surrounding the middle ear windows and the otic capsule. The clinical utility of CT scanning for OS is still up for debate. In order to aid with surgical planning and patient management, HRCT scanning is recommended as an efficient way of recognizing middle ear abnormalities and affirming the presence of OS prior to management [10].
This study sought to determine if the degree of OS and the degree of hearing loss (conductive or sensorineural) were related, as well as whether HRCT scanning accurately identified otosclerolic foci.
Methods
Participants
This prospective randomized controlled study was conducted from June 2018 to June 2022 on patients identified as OS, regardless of age or gender, attending otorhinolaryngology clinics in Damietta, Al-Azhar University Hospital in Egypt or private centers. The exclusion criteria for all participants include no history of past exposure to noise, ototoxic medication use, no history of congenital disease and no history of consanguinity, head trauma, diabetes mellitus, hypertension, kidney, or cardiovascular illness.
Fifty healthy adult volunteers made up the control group (group 1). They all had normal hearing thresholds, normal otoscopic findings, and normal middle ear as shown by both tympanometry and acoustic reflex. They were chosen from the workers at Damietta Al-Azhar University Hospital as well as from relatives of patients who accompanied them to the Otorhinolarngology clinics and audiology clinics in university hospital or private centers.
This patients (group 2) consists of 50 individuals with OS, of which 15 have unilaterally and 35 have bilaterally, for a total of 85 afflicted ears.They were classified into 2 subgroups; group 2a: early OS involved 50 ears and group 2b: late OS involved 35 ears.
When a patient experiences hearing loss that lasts less than thirty months (the average duration of the disease in our study), we refer to it as early OS. We used the term "late OS" to refer to hearing loss that has been present for more than 30 months.
The Helsinki Declaration and the standard operating procedure standards of the Helsinki and Domietta Faculty of Medicine et al. Azhar University were followed in the acceptance of this research, with the approval number (DFM-IRB 00012367–23-09–001) serving as the basis. Every participant provided written consent.
Otological and audiological evaluation
Participants in all groups underwent the following assessments: Taking a detailed medical history to rule out any systemic illness, hearing loss in the family, otoscopic evaluation, basic audiological testing, involving the subsequent: a) Pure tone audiometry in octaves, starting at 250,500,1000,2000,4000,8000 Hz for air conduction and 500,1000,2000,4000 Hz for bone conduction. The TDH 39P supra-aural headphone type was used to give the air conduction stimulation. A bone conduction vibrator was used to deliver the bone conduction. b) Speech audiometry, which uses Arabic phonetically balanced words (PB words) for speech discrimination scores and Arabic spondee words for speech reception threshold (SRT). c) Tympanometry, which is performed at pressures between + 200 and –400 mm H2O, and acoustic reflex threshold evoked same and other side using a frequency range of (500 up to 4000Hz) are two components of impedancemetry.
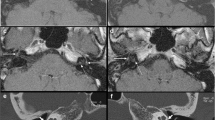
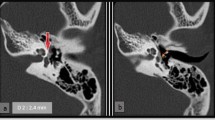
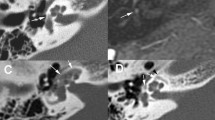
HRCT study
Axial and coronal temporal bone CT cuts were produced using the following parameters (cut thickness, 0.5–1 mm; increment, 0.5 mm). With the use of a 4-detector CT, high-quality images of the temporal bones have been captured. At least two radiologists reviewed all HRCT studies (Fig. 1).
The otic capsule's hypodense zones or the presence of localized thickening and/or decimation lesions within the oval and round windows were used to describe lesions with OS. Any footplate thickness greater than 0.6 mm is thought of as abnormal. Otosclerotic foci were localized within the otic capsule and were restricted to fenestral and retrofenestral lesions [11].
Six places are most frequently affected by OS; ante fenestrum, round window, cochlear promontory, cochlear apex, basal turn of cochlea, and posterior fenestrum [12].
CT grading
Grade 0: normal. Grade 1: a small lucent lesion within the fissula ante fenestram. Grade 2A: characterized by sclerosis and constriction of the basal turn. Grade 2B: lucent lesion that extends to the cochlea's middle turn from the fissula ante fenestram. Grade 2C: Patchy lucency surrounds the lateral side of the basal, middle, and apical turns of the cochlea, while the medial region of the cochlea appears to be spared. Severe, confluent lucency encircling the cochlea is grade 3 [6].
Statistical analysis
The analyses were carried out using the statistical software SPSS v23 (SPSS, Inc., Chicago, Illinois). Descriptive statistics, such as mean, standard deviation, frequency, and correlation coefficients, were calculated for each measure. A paired t-test was used to compare the two groups, and P values were ascertained by applying the corresponding χ2 test, Pearson's correlation test, one-sample t-test, and Wilcoxon test as needed. The Analysis of Variance (ANOVA) test should be used when comparing more than two groups (F). A statistically significant level was defined as P < 0.05.
Results
This study includes 50 patients with OS; 15 of them was unilateral and another 35 patients with bilateral OS of total 85 affected ears. Their ages ranged from 23 – 39 years. They were 28 ears for males and 57 ears for females. They were classified into two subgroups; early OS involved 50 ears (15 males and 35 females) and late OS involved 35 ears (13 males and 22 females). Another 50 ears of 50 healthy volunteers were served as control subjects, they were 25 males and 25 females matched with the patients’ group (p > 0.05) (Table 1).
Air conduction threshold (ACT) showed elevation in the early OS group than control subjects and much more elevation in late OS then both early and control subjects (p < 0.001) (Table 2).
Bone BCT showed elevation in the early OS group than control subjects and more elevation in late OS then early OS and control subjects (p < 0.001) (Table 3). Air–bone gap (ABG) was increased in late than early OS (p < 0.001). These tests were observed in all audiometric tones used (Air conduction done from 250 to 8000 Hz; while in bone conduction done only for 500 to 4000 Hz) (Table 4).
The results of several audiometric tests were contrasted with the Footplate thickening (FPT) results from the CT scan. FPT significantly correlates with means of 36.4 dB and 52.75 dB in air conduction in early and late OS, respectively (P = 0.002). Significant correlation of 11 dB and 21.6 dB in bone conduction in early and late OS, respectively (P = 0.004), with a significant ABG of 25.5 and 31 dB in early and late OS, respectively (P = 0.03) (Table 5).
Grading by computed tomography in early and late OS were performed. Grade 1 was found in 26% of the affected ears in early OS only, grade 2A in 54% in early OS and 8.6% in late OS. Grade 2B in 18% in early OS and 22.9%, in late OS. Grade 2C in 2% and 31.4% in early and late OS, respectively and finally grade 3 was found in 37.1% in late OS only. They showed a statistically highly significant differences between early and late OS in all grades (P < 0.001) except grade 2B that showed significant difference (p = 0.041) (Table 6).
In the current study, HRCT demonstrated a sensitivity of 75%, high specificity of 92%, and accuracy of 83% in early OS and 78%, high specificity, and accuracy of 94% in late OS (Table 7).
Discussion
When doing HRCT scans for OS, a bone computational scan with a slice thickness of 1 mm or less is usually used; higher slice thicknesses result in higher false negative rates. Several studies have demonstrated that the sensitivity of HRCT is limited by infra-millimeter with superficial foci, dormant illness, and density variations of less than 200 Hounsfield units that are imperceptible to the naked eye [7, 13].
Better CT scanning equipment with improved collimation is thought to have improved the quality of the images accessible for analysis [14], this has resulted in a greater diagnostic yield, together with the use of automated workstations for image analysis like HRCT. The possibility to zoom in and scroll through images on computerized workstations helps one better understand tiny anomalies [15].
Various studies compared clinical outcomes to evaluate the sensitivity of CT in the diagnosis of OS [8, 16]. Therefore, the goals of our investigation were to ascertain if there is a relationship between the degree of hearing loss and the degree to which OS, as well as the accuracy of HRCT scanning in identifying OS foci. To represent 85 affected ears in this context, we selected 15 unilateral and 35 bilateral otosclerotic patients, in comparison to 50 healthy ears (controls).
In our study, there is a highly significant difference between patients with early OS compared to controls, while there is a very highly significant difference between late OS and controls as regard delay in air-conduction threshold in all pure tone audiometry. However, it was more significant between 1 and 4 kHz with maximum value at 2 kHz (Carhart notch).
This was identical to other studies that found that the mean ambient absorbance values in the normal and OS groups were not significantly different at low frequencies up to 1 kHz, contrary to previous findings in a larger sample of ears [17].
The tympanic membrane (TM) may have stiffened because of the ossicular chain's relative stiffness, overloading the TM, which might account for these low-frequency effects. The OS group had a notable and distinct decrease in ambient absorbance at 4 kHz, which might be related to functional variations in ossicular-chain transmission above the first resonance of the TM. The tympanometric absorbance at the tympanometric peak pressure (TPP) at low frequencies (0.7–1 kHz) and the absorbance at the positive-tail pressure (2.8 kHz) both showed mean variations [18].
Furthermore, a different investigation corroborated our findings, observing that at both the early and late phases of the OS, hearing loss was considerably higher than in the reference population for both air and bone conduction thresholds, although it was more noticeable in the late group [19].
In a study that observed the same results and stated that Carhart notch was observed at 2 kHz. They advised no treatment required in air conduction thresholds are lower than 30 dB HL or air–bone gap less than15dB. Treatment would be medical in early and surgical in late OS. Therefore, it is important to determine the stage of OS for an appropriate treatment modality [20, 21].
Our study found that CT scanning had a 75% sensitivity, a high specificity of 92%, and an accuracy of 83% in OS diagnosis. Several investigations examined audiometric and CT data to determine if endosteal marginal involvement is linked to SNHL related to OS. Patients with endosteal involvement on CT were reported to have an average BCT that was considerably higher than those without endosteal involvement [22]. This suggests a positive endosteal marginal involvement on CT images and a generally optimal association between the OS resulting in SNHL. On histology, every temporal bone with endosteal marginal involvement on CT showed endosteal marginal involvement [23]. The current investigation demonstrates a strong association between audiometric and CT results.
According to history and audiometry, it was found radiolucent regions in 45% of individuals who were suspected of having cochlear OS. This weak correlation may have resulted from a misdiagnosis of cochlear otosclerosis or from the CT scan's inability to identify radiolucent foci involving the endosteal border [24]. The low association seen in the previous research can be partially explained by the 37% (3/8) false negative rate for endosteal marginal involvement on CT, consequently, CT is not as reliable in ruling out participation in their research but can be utilized to establish endosteal marginal involvement [14].
A broad range of sensitivity, from 34 to 95%, was reported in earlier evaluations; some reviews stated values higher than 90% [25]. The reviewed literatures showed a high positive predictive value, a high specificity, and a poor sensitivity overall. However, there were high confidence ranges, especially in the sensitivity, which was mostly because of another work (12%) [26].
Other considerations include the diversity of features across the people being tested and potential differences in disease stages at the time of the scans. For instance, only a research sample of Taiwanese individuals was included in the investigation of HRCT in the diagnosis of OS in Taiwan (46% sensitivity). As with previous reports suggesting low sensitivity and incidence in other ethnic groups, it is impossible to determine whether the relatively low sensitivity in this study is due to ethnic differences per se or is a manifestation of other factors like patients presenting late in the otosclerotic phase. These problems are inextricably linked to the delayed presentation and maybe the low level of sensitivity about HRCT. These results' wider scope is restricted by the subgroup's unique characteristics [7, 27].
Even though retrofenesteral OS is less prevalent than fenesteral OS, HRCT is superior at diagnosing fenestral OS, supporting findings from other investigations. However, recognizing retrofenestral and endosteal margin involvement remains problematic [26, 28]. Research has indicated the limits of HRCT in the diagnosis of retrofenestral OS, with a 58% sensitivity [29].
The cochlear, pericochlear, and regions anterior to the round window niche are the primary regions of concern in retrofenesteral OS [30]. Because of the possibility of developing SNHL, cochlear disease has clinical consequences for treatment planning and patient counseling. Preoperative diagnosis is therefore beneficial.
Unluckily, there are still issues with CT diagnosis, especially in cases with tiny otospongiotic foci and associated disorders that demineralize the otic capsule, such syphilis, osteogenesis imperfecta, or Paget's disease. These limitations are pointed out in another study, where CT was 63% sensitive in detecting endosteal margin involvement.inframillimeter disease was the cause of the misleading negative results. This highlights that while endosteal lesions can be detected by HRCT, they cannot be ruled out definitively [7, 28].
Our study requires additional patients with a greater range of variations, despite our best efforts to ascertain if HRCT imaging contributes to the diagnosis of OS in association with audiological results.
Conclusion
When compared to audiometry, HRCT is more sensitive and specific for the diagnosis and grading of OS. Since HRCT was able to distinguish between early and late OS, it may be utilized to make this difference more accurately.
Availability of data and materials
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Purohit B, Hermans R, Op de Beeck K (2014) Imaging in otosclerosis: A pictorial review. Insights Imaging 5(2):245–252. https://doi.org/10.1007/s13244-014-0313-9
Wegner I, Bittermann AJ, Hentschel MA, Van Der Heijden GJ, Grolman W (2013) Pure-tone audiometry in otosclerosis: Insufficient evidence for the diagnostic value of the Carhart notch. Otolaryngol Head Neck Surg 149:528–532
Bittermann AJ, Rovers MM, Tange RA, Vincent R, Dreschler WA, Grolman W (2011) Primary stapes surgery in patients with otosclerosis: Prediction of postoperative outcome. Arch Otolaryngol Head Neck Surg 137:780–784
Wegner I, Verhagen JJ, Stegeman I, Vincent R, Grolman WA (2016) Systematic review of the effect of piston diameter in stapes surgery for otosclerosis on hearing results. Laryngoscope 126:182–190
Ho S, Patel P, Ballard D, Rosenfeld R, Chandrasekhar S (2021) Systematic Review and Meta-analysis of Endoscopic vs Microscopic Stapes Surgery for Stapes Fixation. Otolaryngol Head Neck Surg 165:626–635
Lee TC, Aviv RI, Chen JM, Nedzelski JM, Fox AJ, Symons SP (2009) CT Grading of Otosclerosis. Am J Neuroradiol 30(7):1435–1439. https://doi.org/10.3174/ajnr.A1558
Lee TL, Wang MC, Lirng JF, Liao WH, Yu EC, Shiao AS (2009) High resolution computed tomography in the diagnosis of otosclerosis in Taiwan. J Chin Med Assoc 72:527–532
Lagleyre S, Sorrentino T, Calmels MN, Shin YJ, Escude B, Deguine O et al (2009) Reliability of high-resolution CT scan in diagnosis of otosclerosis. Otol Neurotol 30(8):1152–1159
Marx M, Lagleyre S, Escude B et al (2011) Correlations between CT scan findings and hearing thresholds in otosclerosis. Acta Otolaryngol 131:351Y7
Virk JS, Singh AL, Ravi K (2013) The Role of Imaging in the Diagnosis and Management of Otosclerosis. Otol Neurotol 34(7):e55–e60. https://doi.org/10.1097/MAO.0b013e318298ac96
Francis V, Sophie R, Bogdan E, Danisia H, Marie-Noëlle R, Michel G, Jean T (2001) Imaging of the windows of the temporal bone Seminars in Ultrasound, CT, and MRI. In: Seminar of Ultrasound, CT and MRI. Elsevier 22(3):271–280. https://doi.org/10.1016/S0887-2171(01)90011-3
Dewan K, Wippold FJ 2nd, Lieu JE (2009) Enlarged vestibular aqueduct in pediatric SNHL. Otolaryngol Head Neck Surg 140(4):552–558
Bassiouni M, Bauknecht H-C, Muench G, Olze H, Pohlan J (2023) Missed Radiological Diagnosis of Otosclerosis in High-Resolution Computed Tomography of the Temporal Bone—Retrospective Analysis of Imaging, Radiological Reports, and Request Forms. J Clin Med 12(2):630. https://doi.org/10.3390/jcm12020630
Quesnel AM, Moonis G, Appel J, O’Malley JT, Curtin HD, McKenna MJ (2013) In response to letter to the editor: “Correlation of computed tomography with histopathology in otoslcerosis”, Quesnel et al. Otol Neurotol 2013; 34(1): 22–8. Otol Neurotol 34:1546–1547
Kanzara T, Virk JS (2017) Diagnostic performance of high-resolution computed tomography in otosclerosis. World J Clin Cases 5(7):286–291
Berrettini S, Ravecca F, Volterrani D, Neri E, Forli F (2010) Imaging evaluation in otosclerosis: single photon emission computed tomography and computed tomography. Ann Otol Rhinol Laryngol 119(4):215–224
Shahnaz N, Bork K, Polka L, Longridge N, Bell D, Westerberg BD (2009) Energy reflectance and tympanometry in normal and otosclerotic ears. Ear Hear 30(2):219–233
Keefe DH, Archer KL, Schmid KK, Fitzpatrick DF, Feeney MP, Hunter LL (2017) Identifying Otosclerosis with Aural Acoustical Tests of Absorbance, Group Delay, Acoustic Reflex Threshold, and Otoacoustic Emissions. J Am Acad Audiol 28(9):838–860. https://doi.org/10.3766/jaaa.16172
Redfors YD, Möller C (2011) Otosclerosis: thirty-year follow-up after surgery. Ann Otol Rhinol Laryngol 120(9):608–614. https://doi.org/10.1177/000348941112000909
Somers T, Declau F, Kuhweide R, Robillard T (2007) Otosclerosis. Acta oto-rhino-laryngologica Belgica 3:3–10
Maalouf RR, Marc M, Mukherjee P, Van Rompaey V, Eliezer M, Hautefort C, Verillaud B, Herman P, Kania R (2023) Otosclerosis: audiometric results and quality of life after stapedectomy with interposition or CO2 laser-calibrated stapedotomy without interposition. Acta Otolaryngol 143(3):231–236. https://doi.org/10.1080/00016489.2023.2186482. (Epub 2023 Mar 20 PMID: 36939022)
Kawase S, Naganawa S, Sone M, Ikeda M, Ishigaki T (2006) Relationship between CT densitometry with a slice thickness of 0.5 mm and audiometry in otosclerosis. Eur Radiol 16(6):1367–73
Pucetaite M, Quesnel AM, Juliano AF, Curtin HD, Reinshagen KL (2020) The Cochlear Cleft: CT Correlation With Histopathology. Otol Neurotol 41(6):745–749. https://doi.org/10.1097/MAO.0000000000002637. (PMID: 32221113)
Guneri EA, Ada E, Ceryan K, Guneri A (1996) High-resolution computed tomographic evaluation of the cochlear capsule in otosclerosis: relationship between densitometry and sensorineural hearing loss. Ann Otol Rhinol Laryngol 105(8):659–664
Shin YJ, Fraysse B, Deguine O, Cognard C, Charlet JP, Sévely A (2001) Sensorineural hearing loss and otosclerosis: a clinical and radiologic survey of 437 cases. Acta Otolaryngol 121:200–204
Zhu MM, Sha Y, Zhuang PY, Olszewski AE, Jiang JQ, Xu JH, Xu CM, Chen B (2010) Relationship between high-resolution computed tomography densitometry and audiometry in otosclerosis. Auris Nasus Larynx 37:669–675
Wegner I, van Waes AM, Bittermann AJ, Buitinck SH, Dekker CF, Kurk SA, Rados M, Grolman W (2016) A Systematic Review of the Diagnostic Value of CT Imaging in Diagnosing Otosclerosis. Otol Neurotol 37:9–15
Vicente Ade O, Yamashita HK, Albernaz PL, Penido NO (2006) Computed tomography in the diagnosis of otosclerosis. Otolaryngol Head Neck Surg 134:685–692
Dudau C, Salim F, Jiang D, Connor SE (2017) Diagnostic efficacy and therapeutic impact of computed tomography in the evaluation of clinically suspected otosclerosis. Eur Radiol 27:1195–1201
Grayeli AB, Yrieix CS, Imauchi Y, Cyna-gorse F, Ferrary E, Sterkers O (2004) Temporal bone density measurements using CT in otosclerosis. Acta Otolaryngol 124:1136–1140
Acknowledgements
Thanks for all our collages and participants who help in this work for their compliance and patience.
Funding
No particular grant was given for this research by governmental, private, or nonprofit funding organizations.
Author information
Authors and Affiliations
Contributions
IHA had given his help in scientific writing, responsible for audiological data collection and analysis and contributed to the design of the research. YGA contributed to the design and was responsible for radiological data collection and analysis. BAZ contributed to the design and radiological data collection and analysis. HAH was responsible for study conception and design, analysis, otorhinolaryngology data collection, writing of manuscript, and publication. SSG was responsible for study conception and design, material preparation, data collection. All authors discussed the results and approved final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Helsinki Declaration and the standard operating procedure standards of the Helsinki and Domietta Faculty of Medicine et al. Azhar University were followed in the acceptance of this research, with the approval number (DFM-IRB 00012367–23-09–001) serving as the basis. Every participant provided written consent.
Consent for publication
Not applicable.
Competing interests
No conflict of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abd-Elhmid, I.H., Abish, Y.G., Zaghloul, B.A. et al. Correlation between audiological and radiological findings in otosclerosis: randomized clinical study. Egypt J Otolaryngol 40, 65 (2024). https://doi.org/10.1186/s43163-024-00627-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-024-00627-z