Abstract
Background
Mucormycosis is an invasive and possibly fatal fungal infection that frequently affects the mouth. Co-infection in post COVID-19 patients is an emerging concern, owing to their complex nature and higher mortality. Therefore, this study aimed to report the underlying risk factors, clinical characteristics, presentation, and final outcome of COVID-19 associated oral mucormycosis cases.
Results
This study included 51 patients with oral mucormycosis 28 (55%) males and 23 (45%) females. Twenty-three patients (45%) presented with deep necrotic ulcer, 16 patients (31%) presented with superficial ulcer, and 12 patients (23%) of them presented with fistula. The overall survival rate was 51% (26 patients recovered). On the other hand, mortality rate was 49% (25 patients), of which 68% suffered from uncontrolled diabetes mellitus.
Conclusions
The mortality rate of COVID-19 associated mucormycosis cases with oral manifestations was found to be quite high mostly due to delayed diagnosis and lack of timely treatment. Thus, increasing the awareness of dentists and maxillofacial surgeons is crucial for the early diagnosis of oral mucormycosis which is vital to improve prognosis of this serious infection. This is of high importance in view of the escalating numbers of mucormycosis cases being recorded worldwide.
Similar content being viewed by others
Background
Mucormycosis or black fungus is an aggressive potentially fatal fungal infection that is caused by phycomycetes mainly by species of Rhizopus and Mucor. Humans could be infected primarily via inhalation of spores and sometimes by accidental inoculation or consumption of polluted diet [1].
Mucormycosis is characterized by angio-invasion and poor prognosis [2, 3]. The exact frequency or prevalence of mucormycosis is difficult to ascertain because most cases are misdiagnosed because deep tissue samples are difficult to obtain and current test methods have low sensitivity [4, 5]. There are six possible clinical manifestations of mucormycosis: cutaneous, pulmonary, gastrointestinal, central nervous system, and rhinocerebral [6]. The rhinocerebral variety, which accounts for about half of all zygomycosis cases, is the most common form observed in dental practice [7, 8].
Rhino-orbito-cerebral mucormycosis (ROCM) form may present with wide range of symptoms, including runny nose, facial edema, orofacial pain, and loosening of the teeth, as well as the development of an oro-nasal/oro-antral fistula and a black necrotic ulcer or sequestrum in the palate, buccal vestibule, or maxillary alveolus. Following the disease’s spread into the cerebral vault, it may result in mortality, seizures, lethargy, and blindness [9].
Mucormycosis of the maxillary sinus follows breathing of the sporangiospores of mucoromycetes molds that are abundant in the environment and may spread to the hard palate and progress into painful necrotic ulcers [10, 11].
The exact species that causes mucormycosis and the prevalence of risk factors and underlying systemic disorders may vary by country around the world [2]. The ongoing COVID-19 outbreak had damaging and deteriorating effects on the superior respiratory tract and the eye, raising the susceptibility to fungal infection along with the associated acute inflammatory immune response; thus, it is currently considered one of debilitating condition that predisposes patients to mucormycosis besides diabetes. It was even suggested that invasive mucormycosis are more prone to occur in COVID-19 patients, particularly those who are immunocompromised or severely ill [12].
Mucorales spores may germinate more easily in patients with SARS-CoV-2 infection in cases of hypoxia, diabetes, hyperglycemia, and ketoacidosis brought on by steroids, immune subversion, mechanical ventilation, and extended hospital stays [2, 3]. More than 100 occurrences of oral and maxillofacial mucormycosis in COVID-19 patients were documented in a recent thorough review [13].
Given the high morbidity and mortality of this rapidly progressive fulminant fungal infection, a comprehensive and efficient multidisciplinary treatment must be performed swiftly. The overall mortality rate of rhinocerebral mucormycosis is still high despite active interventions;, thus, future research has to concentrate on finding ways to get an early diagnosis, implementing vigorous multidisciplinary therapy, and exploring novel therapeutic options [14].
Currently, the available literature discussing different risk factors and clinical presentations of COVID-19 associated oral mucormycosis is still scarce and mostly limited to either case reports or case series with no long-term data available.
Methods
Aim
The present investigation aimed to assess the clinical characteristics, systemic comorbidities, risk factors, and the final outcome of COVID-19 associated oral mucormycosis cases during the viral pandemic in Egypt.
Study design and patient’s selection
This retrospective cross-sectional multicenter study analyzed data from 51 post COVID-19 patients with oral mucormycosis in different hospitals and institutes in Egypt.
Sample size
Convenience sampling, a kind of non-probability sampling, was used to recruit patients. It involves considering the current pool of post COVID-19 patients who have oral mucormycosis and were infected between September 2021 and March 2023.
Inclusion criteria
Post COVID-19; patients on or who had corticosteroids and immunosuppressive drugs; ROCM type.
Exclusion criteria
Patients with pulmonary, cutaneous, gastrointestinal, and disseminated mucormycosis types.
The protocol of this study was in accordance with the principles established by the Declaration of Helsinki and approved by the ethics committee of the British University in Egypt, Cairo, Egypt (BUE REC-21–022).
Data for patients were collected by electronic survey filled by the internal residents in the ENT clinics which included history taking (personal history, current and past medical and drug history, presence or absence of oxygen therapy and its type, presence or absence of mucormycosis and if yes then presence or absence of the oral involvement, the presence or absence of eye manifestations and the symptoms that mainly affect those patients).
If the patient had oral mucormycosis in our survey then he or she was subjected to intra-oral examination by oral medicine specialist using plain dental mirror under the artificial light to detect the presence of oral lesion, ask about its symptoms, detect its location, clinical presentation of the lesion, as well as color of the surrounding mucosa as showed in Figs. 1, 2 and 3.
a Showing left facial swelling with black crust on the left nostril. b The left half of the hard palate showing superficial ulcer with yellowish exudates. c Axial CT showing opacification of the left nasal cavity, left ethmoidal air sinus and thickening of the lining mucosa of the left maxillary sinus
a Showing left cheek swelling and facial asymmetry with history of headache and facial pain of acute onset. b Showing superficial ulcer with yellowish exudate at the hard palate with history of facial pain of acute onset. c T1 weighted MDI image showing low to intermediate signal intensity within the nasal cavities, thickening of the lining mucosa of the left sinus with intermediate signal intensity
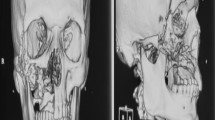
a Showing right facial swelling and black crustation at the right nostril. b Showing deep ulcer with black necrotic mucosa at the right half of the hard palate associated with loose teeth at the same side and perforation of the palate. c Axial CT bone window showing unilateral proptosis related to the right orbit and partial opacification of the ethmoidal air sinus and complete opacification of the right and left nasal cavities, mucosal thickening and air-fluid level in the right maxillary sinus
Then, a radiographic assessment with computerized tomography (CT) scan of the paranasal sinuses (PNS) and magnetic resonance imaging (MRI) requested if central nervous system (CNS) manifestations were present and they were evaluated by multidisciplinary team. A biopsy specimen from tissue samples, such as nasal/sinus tissue, and excisional biopsies from ulcers were evaluated microbiologically and histopathologically to reach a definite diagnosis in all the suspected cases. The patients with oral mucormycosis were followed up to 12 months to assess the final outcome.
Data of the patients were recorded and analyzed using IBM SPSS software package version 20.0.Footnote 1 The Kolmogorov–Smirnov was used to confirm the normality of variables’ distribution. Comparisons of groups regarding categorical variables were evaluated using chi-square test (Fisher or Monte Carlo).
Results
The present study included a total of 51 patients with oral mucormycosis 28 males (55%) and 23 females (45%) with mean age of 50.8 ± 15.4. Many patients 25 (49%) suffered from uncontrolled diabetes mellitus (DM), 19 (37%) suffered from hypertension, 14 (27%) had controlled diabetes mellitus, 9 (17%) had ischemic heart disease (IHD), and 8 (16%) were medically free.
All patients with oral mucormycosis received systemic corticosteroids as well as systemic antibiotics in the treatment protocol of COVID-19. Besides, 37 (72%) of them were on oxygen therapy, 10 (19%) of them were on C-PAP while 27 (53%) used oxygen mask. Regarding eye and CNS involvement, 26 (51%) of the patients had eye lesions, while 22 (43%) of the patients had CNS manifestations as shown in Table 1.
All patients had palatal lesions with different clinical presentations as shown in Fig. 4. Twenty-three patients (45%) presented with deep necrotic ulcer, 16 patients (31%) presented with superficial ulcer, and 12 (23%) of them presented with fistula.
Regarding the color of affected palatal mucosa, 10 patients (19%) had normally looked mucosa, and 19 patients (37%) had yellowish exudate, while 22 patients (43%) had necrotic black mucosa.
Regarding early symptoms, 50 patients with oral mucormycosis (98%) complained of different early symptoms, 39 patients (78%) had facial pain, 32 patients (64%) had dental pain, 18 patients (36%) had headache, and 8 patients (16%) had swelling, while only one patient (2%) complained of fever. It is apparent that the majority presented at the first time with dental and facial pain.
Additionally, 25 patients with oral mucormycosis (49%) presented with late symptoms, 17 of them (68%) had loose teeth, 20 patients (80%) had foul odor, 22 patients (88%) had palatal perforation, and 9 patients (36%) had nasal perforation as shown in Fig. 4.
The overall survival rate was 51% (26 patients recovered). On the other hand, mortality rate was 49% (25 patients) in the present study, of which 68% suffered from uncontrolled diabetes mellitus. Moreover, 92% of diseased patients had deep necrotic ulcer and 88% had necrotic black mucosa. Additionally, 88% of fatalities were associated with eye lesions and CNS manifestations as presented in Table 2.
The relation between clinical picture and different medical conditions showed that patients with uncontrolled diabetes mellitus had superficial ulcers (37.5%), deep necrotic ulcer (65.2%), and fistula (33.3%). Patients with hypertension had superficial ulcer (37.5%), deep necrotic ulcer (43.5%), and fistula (25.0%). While 12.5% of the medically free patients had superficial ulcer, 4.3% of them had deep necrotic ulcer, and 41.7% had fistula as presented in Table 3.
Discussion
The current COVID-19 pandemic may coexist with a variety of bacterial and fungal infections, particularly mucormycosis, especially in cases where there is underlying comorbidity such diabetes mellitus or lung diseases [15]. Moreover, the use of systemic corticosteroid in immune-compromised patients with uncontrolled diabetes is blamed to be the reason behind the current rise in mucormycosis cases [16].
Certain characteristics of COVID-19, such as its ability to result in widespread lung disease and consequent alveolo-interstitial pathology, may increase the risk of aggressive fungal infections. Furthermore, the immunological dysregulation linked to COVID-19, which is characterized by a decrease in T lymphocytes, particularly CD4 + T and CD8 + T cells, may modify the innate immune response against a range of pathogenic pathogens [17].
Mucormycosis is classified according to the occurrence site to rhinocerebral, pulmonary, cutaneous, gastrointestinal, and disseminated types [18]. Rhinocerebral or sino-orbital types are common among diabetics, especially poorly controlled diabetic patients. These types may present with a variety of symptoms of sinusitis. Tissue necrosis is a characteristic sign of mucormycosis, stemming from angio-invasion with consequent vascular thrombosis [19]. Approximately 40–70% of all reported mucormycosis cases manifest signs and symptoms involving facial and oral tissues [20].
In the present study, males demonstrated a higher prevalence in oral mucormycosis patients than females. This was in accordance with previous studies who reported the higher prevalence of mucormycosis among males [21,22,23,24,25,26]. Results of the present study showed a mean age in patients with oral mucormycosis of 50.8 ± 15.4 years. This agreed with previous studies [21, 24, 25].
The majority of the 43 (84.3%) oral mucormycosis patients in the current study had multiple medical disorders. However, of these patients, only 8 (15.7%) were free from medical conditions. Patients that are medically compromised are typically linked to mucormycosis. These infections often spread locally in an immunocompetent host, going straight to the nearby tissue and sporadically spreading elsewhere. Mucormycosis may develop in otherwise healthy or immunocompetent people as a result of a persistent injury that occurs locally [27]. This theory was further reinforced by the observation that a persistent local injury modifies the body’s first line of defense by impairing the mucous membrane, leaving the victim more susceptible to fungus infection [28]. These factors hence explain possible mucormycosis in immunocompetent individuals.
However, the most common medical condition reported in patients with oral involvement in our study was 22 patients with uncontrolled DM (43.13%). This result was in accordance with previous studies which reported a high prevalence of uncontrolled diabetes mellitus among their studied samples [2, 21, 24, 25, 29, 30]. Patients with uncontrolled DM are poorly affected by hyperglycemia as well as immune dysfunction, for instance neutrophils dysfunction, decline of antioxidant system, and humoral immune system. Germination and aggressive growth of the fungal spores are accelerated by elevated glucose levels, increased levels of ketone bodies, lowered pH, diminished oxygen, and high level of iron [31].
In several studies, DM has been described as a predisposing factor [32,33,34]. Patients with poorly controlled DM, specifically those with ketoacidosis, are the most liable [7]. Furthermore, mucormycosis is rarely found in people with well-controlled DM [35], although it may be the first symptom in some undiagnosed DM patients [35, 36]. There are several purported risk factors for mucormycosis, including type 1, type 2, and secondary DM [33]. Consequently, with an average mortality rate of 50%, diabetes mellitus continues to be the main risk factor internationally connected with mucormycosis [2].
All patients in our study with oral involvement received systemic corticosteroids as well as systemic antibiotics. This was not surprising as corticosteroid therapy is a known major risk factor that renders the patients more susceptible to mucormycosis by inhibiting macrophage and neutrophil functions as well as steroid-induced hyperglycemia [29, 37]. While consumption of corticosteroids for prolonged durations has often been associated with numerous opportunistic fungal infections as mucormycosis, even a brief corticosteroids course has just been confirmed to be associated with mucormycosis especially in diabetic patients. An accumulative dose of greater than 600 mg prednisone or a total dose of 2–7 g methyl prednisone provided during the previous month predisposes immunocompromised patients to mucormycosis [38]. Our results agreed with previous studies which reported up to 88% of the mucormycosis patients were on corticosteroid therapy [13, 39].
Furthermore, few case reports of mucormycosis following even a shorter steroid course (5–14 days) were reported, especially in diabetic patients [40]. Moreover, in a former study, 46% of patients had taken corticosteroids during the month preceding the diagnosis of mucormycosis [41]. These findings necessitate reconsideration of corticosteroid use in the course of COVID-19 pandemic. Likewise, a number of case reports are being registered from other parts of the world. These conclusions are exceptional and carry an enormous public health significance particularly because of the high mortality rate of mucormycosis. Particularly cases of intracranial mucormycosis which boosts the mortality rate to as high as 90% [42].
In the present study, the early symptoms reported by oral mucormycosis cases were assessed, most cases (78%) presented at the first time with facial pain, dental pain (64%), followed by 36% who had headache and 16% who had swelling, while only 2% had fever. On the contrary, most cases reported late symptoms (49%) and the most encountered late symptom (88%) were perforating palate, followed by foul odor (80%), loose teeth (68%), and perforating nose (36%). These results were in accordance with [28, 43, 44], who reported similar clinical findings.
Oral ulceration is preceded by facial pain and swelling, which then develops into necrotic eschars in the palate and nasal turbinates, leading to osteomyelitis or denudation of the underlying bone. Angio-aggressive infections are indicated by necrotizing lesions [45, 46]. A paranasal sinus infection can quickly transfer to the orbit and nasolacrimal duct, or it might cause palatal perforation. Infection can reach the brain via the cribriform plate, vessels, or orbital apex [47].
Moreover, eye involvement was evident in 26 (51%) of our studied sample of oral mucormycosis cases with varied clinical manifestations. Our findings were also in line with other studies which reported that the primary symptoms might include eye and/or facial pain and numbness pursued by blurry vision [37]. And another study revealed the signs and symptoms suggestive of mucormycosis in vulnerable people such as unilateral periorbital facial pain, multiple cranial nerve palsies, eyelid edema, orbital inflammation, blepharoptosis, proptosis, acute ocular motility changes, headache, and acute loss of vision. Though a black necrotic eschar is the characteristic sign of mucormycosis. Nevertheless, its absence should not rule out the probability of mucormycosis [48].
Assessment of the clinical manifestations in the present study revealed that in most mucormycosis cases (71.4%) the oral lesions were presented as palatal ulcers where 52.4% of them were deep necrotic ulcers, and 19% were superficial palatal ulcers, while 28.6% of cases presented with fistula. Regarding the color of affected palatal mucosa, 23.8% had normal looking mucosa, and 28.6% had yellowish exudate, while 47.6% of cases had necrotic black mucosa. Our results align with a number of studies that documented the occurrence of excruciating ulcers or necrotic palatal ulcers that began early in the illness course occasionally causing palatal perforation, necrosis, oral pain, or even loss of maxillary bone. Therefore, palate ulcerations may be the initial symptom bringing the patient to the dentist; hence, he could be the first to suspect and diagnose mucormycosis infection [49,50,51,52,53].
Maintaining a high index of suspicion is crucial for clinicians interacting with patients at risk since early diagnosis can save lots of lives [54]. Symptoms typically start as a generalized headache and malaise, followed by acute inflammation of the sinuses, eye symptoms, face edema and pain, rhinorrhea, and finally ophthalmoplegia, lethargy and blindness [55].
In the current investigation, patients with mucormycosis associated with COVID-19 had an overall survival rate of 51% (26 individuals recovered). However, the current study’s mortality rate of 49% (25 patients) was consistent with other research [56,57,58]. Furthermore, it was consistent with one of the rare studies carried out in Egypt that revealed a 46.2% overall mortality rate among patients with mucormycosis associated with COVID-19.
This high mortality rate is mostly due to the late appearance, self-medication of COVID-19 instead of seeking medical care for moderate and severe cases, and the excessive or redundant use of corticosteroids [59]. Moreover, 68% of diseased patients suffered from uncontrolled diabetes mellitus, 92% had deep necrotic ulcer, and 88% had necrotic black mucosa. Additionally, 88% of fatalities were encountered in patients with eye lesions and CNS manifestations with mortality [29, 30].
A significant mortality rate following ROCM was previously reported, and a subgroup of patients who present with severe ocular disease or severe COVID-19 are at a higher risk of passing away within 10 days of being admitted [60].
Any disease’s prognosis is heavily influenced by how quickly it spreads, how aggressive it is, and how long it takes to treat it. When pulmonary disease is present along with orbito-cognitive dysfunction, mucormycosis is thought to have a high mortality rate. If the fungus has not spread past the sinus prior to the surgery, the prognosis is substantially better [61]. Time between disease diagnosis and treatment is a significant predictive factor [62].
A previous study reported that by postponing the amphotericin B treatment for more than 5 days the mortality rates increased from 48.6 to 82.9%, particularly in patients with hematologic malignancies [63]. Since ROCM can be identified quicker than pulmonary type, it has a better prognosis when treated promptly [64]. The documented mortality rates for all types of mucormycosis range from 40 to 80%, and the survival rates for individuals who have had organ transplantation or hematological malignancies are much worse [65].
Early diagnosis is the optimum approach in oral mucormycosis management, alongside elimination of all predisposing factors and medical conditions, and timely therapeutic intervention. It is also important for a dentist to be aware of the early signs and symptoms of mucormycosis, particularly when screening high-risk patients, as presence of a non-specific ulcer on the palate. Treatment for mucormycosis should begin as soon as feasible in an effort to reduce mortality; therefore, early diagnosis is essential [45].
Conclusion
Co-infection of mucormycosis in post COVID-19 patients is an evolving concern in Egypt with the documented high incidence of diabetes as well as the tendency for excessive use of steroid therapy especially during the pandemic era. The mortality rate of post COVID-19 associated oral mucormycosis in the present study was found to be quite high mainly due to delayed diagnosis and lack of timely treatment. Thus, it is necessary to increase the awareness of dentists and maxillofacial surgeons of the important oral presentations of mucormycosis in post COVID-19 patients especially deep palatal ulcers and dentofacial pain, which is crucial for the early diagnosis and improved prognosis of such aggressive infection. This is of high importance in view of the escalating numbers of COVID-19 associated mucormycosis cases in Egypt with abundance of the associated risk factors.
This is the first multicentric investigation of COVID-19 linked oral mucormycosis in Egypt; however, in order to track illness patterns during the next pandemic waves, an online national registry is required.
Availability of data and materials
The data that support the findings of this study are available from multiple hospitals and institutes in Egypt and restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data however are available from the corresponding author upon reasonable request.
Notes
Armonk, NY: IBM Corp.
Abbreviations
- ROCM:
-
Rhino-orbito-cerebral mucormycosis
- CT:
-
Computerized tomography
- PNS:
-
Paranasal sinuses
- MRI:
-
Magnetic resonance imaging
- CNS:
-
Central nervous system
- DM:
-
Diabetes mellitus
- IHD:
-
Ischemic heart disease
References
Richardson M (2009) The ecology of the zygomycetes and its impact on environmental exposure. Clin Microbiol Infect 15(Suppl 5):2–9. https://doi.org/10.1111/j.1469-0691.2009.02972.x. (PMID: 19754749)
Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, Chen SC (2019) The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect 25(1):26–34. https://doi.org/10.1016/j.cmi.2018.07.011. (Epub 2018 Jul 21. PMID: 30036666)
Prakash H, Ghosh AK, Rudramurthy SM, Singh P, Xess I, Savio J, Pamidimukkala U, Jillwin J, Varma S, Das A, Panda NK, Singh S, Bal A, Chakrabarti A (2019) A prospective multicenter study on mucormycosis in India: epidemiology, diagnosis, and treatment. Med Mycol 57(4):395–402. https://doi.org/10.1093/mmy/myy060. (PMID: 30085158)
Chakrabarti A, Dhaliwal M (2013) Epidemiology of mucormycosis in India. Curr Fungal Infect Rep 7:287–292. https://doi.org/10.1007/s12281-013-0152-z
Bongomin F, Gago S, Oladele RO, Denning DW (2017) Global and multi-national prevalence of fungal diseases-estimate precision. J Fungi (Basel) 3(4):57. https://doi.org/10.3390/jof3040057. (PMID: 29371573; PMCID: PMC5753159)
Rajendra Santosh AB, Muddana K, Bakki SR (2021) Fungal infections of oral cavity: diagnosis, management, and association with COVID-19. SN Compr Clin Med 3(6):1–12. https://doi.org/10.1007/s42399-021-00873-9. (Epub ahead of print. PMID: 33817556; PMCID: PMC8003891)
Greenberg RN, Scott LJ, Vaughn HH, Ribes JA (2004) Zygomycosis (mucormycosis): emerging clinical importance and new treatments. Curr Opin Infect Dis 17:517–525. https://doi.org/10.1097/00001432-200412000-00003
Jayachandran S, Krithika C (2006) Mucormycosis presenting as palatal perforation. Indian J Dent Res 17:139–142. https://doi.org/10.4103/0970-9290.29873
Reddy SG, Kumar KK, Sekhar CP, Reddy RBV (2014) Oral mucormycosis: need for early diagnosis!!. Journal of Dr. NTR University of Health Sciences 3(2). https://doi.org/10.4103/2277-8632.134900
Verma A, Singh V, Jindal N, Yadav S (2013) Necrosis of maxilla, nasal, and frontal bone secondary to extensive rhino-cerebral mucormycosis. Natl J Maxillofac Surg 4:249–251. https://doi.org/10.4103/0975-5950.127663
Garlapati K, Chavva S, Vaddeswarupu RM & Surampudi J (2014) Fulminant mucormycosis involving paranasal sinuses : a rare case report. Case Rep Dent 465919. https://doi.org/10.1155/2014/465919
Awal SS, Biswas SS, Awal SK (2021) Rhino-orbital mucormycosis in COVID-19 patients—a new threat? Egypt J Radiol Nucl Med. 52:152. https://doi.org/10.1186/s43055-021-00535-9
Singh AK, Singh R, Joshi SR, Misra A (2021) Mucormycosis in COVID19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr 15(4):102146. https://doi.org/10.1016/j.dsx.2021.05.019
Samaranayake LP, Fakhruddin KS, Ngo HC, Bandara HMNM, Leung YY (2022) Orofacial mycoses in coronavirus disease-2019 (COVID-19): a systematic review. Int Dent J:S0020–6539(22)00035–1. https://doi.org/10.1016/j.identj.2022.02.010. Epub ahead of print. PMID: 35367044; PMCID: PMC8885299
Mehta S, Pandey A (2020) Rhino-orbital mucormycosis associated with COVID-19. Cureus 12(9):e10726. https://doi.org/10.7759/cureus.10726
Ravani SA, Agrawal GA, Leuva PA, Modi PH, Amin KD (2021) Rise of the phoenix: mucormycosis in COVID-19 times. Indian J Ophthalmol 69(6):1563–1568. https://doi.org/10.4103/ijo.IJO_310_21. (PMID: 34011742; PMCID: PMC8302276)
Gangneux JP, Bougnoux ME, Dannaoui E, Cornet M, Zahar JR (2020) Invasive fungal diseases during COVID-19: we should be prepared. J Mycol Med 30(2):100971. https://doi.org/10.1016/j.mycmed.2020.100971. (Epub 2020 Apr 6. PMID: 32307254; PMCID: PMC7136887)
Denning DW, Wilson GE (1999) Fungal infections. In: James DG, Zumla A (eds) The granulomatous disorders. Cambridge University Press, Cambridge, pp 235–256. https://doi.org/10.3390/medicina55070319
Kontoyiannis DP, Lewis R.E (2009) “Agents of mucormycosis and entomophthoramycosis,” in Mandell, Douglas, and Bennett’s principles & practice of infectious diseases, G. L. Mandell, J. E. Bennett, and R. Dolin, Eds., chapter 259, pp. 3257–3266, Churchill Livingstone, Livingstone, Zambia, 7th edition. https://doi.org/10.1016/B978-1-4557-4801-3.00260-5
Doni BR, Peerapur BV, Thotappa LH, Hippargi SB (2011) Sequence of oral manifestations in rhino-maxillary mucormycosis. Indian J Dent Res 22:331–335. https://doi.org/10.4103/0970-9290.84313
Kontoyiannis DP, Yang H, Song J, Kelkar SS, Yang X, Azie N, Spalding JR (2016) Prevalence, clinical and economic burden of mucormycosis-related hospitalizations in the United States: a retrospective study. BMC Infect Dis 16:730. https://doi.org/10.1186/s12879-016-2023-z
Patel AK, Patel KK, Patel K, Gohel S, Chakrabarti A (2017) Mucormycosis at a tertiary care centre in Gujarat, India. Mycoses 60:407–411. https://doi.org/10.1111/myc.12610
Chander J, Kaur M, Singla N, Punia R, Singhal S, Attri A, Guarro J (2018) Mucormycosis: battle with the deadly enemy over a five-year period in India. J Fungi 4:46. https://doi.org/10.3390/jof4020046
Manesh A, Rupali P, Sullivan MO, Mohanraj P, Rupa V, George B, Michael JS (2019) Mucormycosis-a clinicoepidemiological review of cases over 10 years. Mycoses 62:391–398. https://doi.org/10.1111/myc.12897
Patel A, Kaur H, Xess I, Michael JS, Savio J, Rudramurthy S, Chakrabarti A (2020) A multi-centre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India. Clin Microbiol Infect 26:944.e9-944.e15. https://doi.org/10.1016/j.cmi.2019.11.021
Priya P, Ganesan V, Rajendran T, Geni VG (2020) Mucormycosis in a tertiary care center in South India: a 4-year experience. Indian J Crit Care Med 24:168–171. https://doi.org/10.5005/jp-journals-10071-23387
Mignogna MD, Fortuna G, Leuci S, Adamo D, Ruoppo E, Siano M, Mariani U (2011) Mucormycosis in immunocompetent patients: a case-series of patients with maxillary sinus involvement and a critical review of the literature. Int J Infect Dis 15(8):e533–e540. https://doi.org/10.1016/j.ijid.2011.02.005
Lane AP (2009) The role of innate immunity in the pathogenesis of chronic rhinosinusitis. Curr Allergy Asthma Rep 9(3):205–212. https://doi.org/10.1007/s11882-009-0030-5
Alfishawy M, Elbendary A, Younes A et al (2021) Diabetes mellitus and coronavirus disease (COVID-19) associated mucormycosis (CAM): a wake-up call from Egypt. Diabetes Metab Syndr 15(5):102195. https://doi.org/10.1016/j.dsx.2021.102195
Assaad Khalil SH, Megallaa MH, Rohoma KH et al (2018) Prevalence of type 2 diabetes mellitus in a sample of the adult population of Alexandria. Egypt Diabetes Res Clin Pract 144:63–73. https://doi.org/10.1016/j.diabres.2018.07.025
Krishna S.D, Raj H, Kurup P, Juneja M (2021) Maxillofacial infections in COVID-19 era-actuality or the unforeseen: 2 case reports. Indian J Otolaryngol Head Neck Surg 1–4. https://doi.org/10.1007/s12070-021-02618-5.
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, Walsh TJ (2005) Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis 41:634–653. https://doi.org/10.1086/432579
Chamilos G, Lewis RE, Kontoyiannis DP (2006) Lovastatin has significant activity against zygomycetes and interacts synergistically with voriconazole. Antimicrob Agents Chemother 50:96–103. https://doi.org/10.1128/AAC.50.1.96-103.2006
Ludvigsson J (2006) Why diabetes incidence increases—a unifying theory. Ann N Y Acad Sci 1079:374–382. https://doi.org/10.1196/annals.1375.058
Kontoyiannis DP (2007) Decrease in the number of reported cases of mucormycosis among patients with diabetes mellitus: a hypothesis. Clin Infect Dis 44:1089–1090. https://doi.org/10.1086/512817
Bhansali A, Bhadada S, Sharma A, Suresh V, Gupta A, Singh P, Dash RJ (2004) Presentation and outcome of rhino-orbital-cerebral mucormycosis in patients with diabetes. Postgrad Med J 80:670–674. https://doi.org/10.1136/pgmj.2003.016030
Ribes JA, Vanover-Sams CL, Baker DJ (2000) Zygomycetes in human disease. Clin Microbiol Rev 13(2):236–301. https://doi.org/10.1128/CMR.13.2.236
Lionakis MS, Kontoyiannis DP (2003) Glucocorticoids and invasive fungal infections. Lancet 362:1828–1838. https://doi.org/10.1016/S0140-6736(03)14904-5
John TM, Jacob CN, Kontoyiannis DP (2021) When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect storm for mucormycosis. J Fungi (Basel) 7(4). https://doi.org/10.3390/jof7040298
Hoang K, Abdo T, Reinersman JM, Lu R, Higuita NIA (2020) A case of invasive pulmonary mucormycosis resulting from short courses of corticosteroids in a well-controlled diabetic patient. Med Mycol Case Rep 29(1):22–24. https://doi.org/10.1016/j.mmcr.2020.05.008
Skiada A, Pagano L, Groll A, Zimmerli S, Dupont B, Lagrou K, Petrikkos G (2011) Zygomycosis in Europe: analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) Working Group on Zygomycosis between 2005 and 2007. Clin Microbiol Infect 17:1859–1867. https://doi.org/10.1111/j.1469-0691.2010.03456.x
Deutsch PG, Whittaker J, Prasad S (2019) Invasive and non-invasive fungal rhinosinusitis—a review and update of the evidence. Medicina 55:1–14. https://doi.org/10.3390/medicina55070319
Venkatesh D, Dandagi S, Chandrappa PR, Hema KN (2018) Mucormycosis in immunocompetent patient resulting in extensive maxillary sequestration. J Oral Maxillofac Pathol 22(Suppl 1):S112-116. https://doi.org/10.4103/jomfp.JOMFP_163_17
Sanath AK, Nayak MT, Sunitha JD, Malik SD, Aithal S (2020) Mucormycosis occurring in an immunocompetent patient: a case report and review of literature. Cesk Patol 56(4):223–226. https://doi.org/10.4317/jced.53655
Barrak HA (2007) Hard palate perforation due to mucormycosis: report of four cases. J Laryngol Otol 121(11):1099–102. https://doi.org/10.1017/S0022215107006354. (Epub 2007 Feb 26 PMID: 17319990)
Kumar JA, Babu P, Prabu K, Kumar P (2013) Mucormycosis in maxilla: rehabilitation of facial defects using interim removable prostheses: a clinical case report. J Pharm Bioallied Sci 5(Suppl 2):S163-5. https://doi.org/10.4103/0975-7406.114322. (PMID: 23956598; PMCID: PMC3740667)
McSpadden RP, Martin JR, Mehrotra S, Thorpe E (2017) Mucormycosis causing Ludwig angina: a unique presentation. J Oral Maxillofac Surg 75(4):759–762. https://doi.org/10.1016/j.joms.2016.10.025. (Epub 2016 Oct 29. PMID: 27875707)
Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP (2012) Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis 54:S23–S34. https://doi.org/10.1093/cid/cir866
Auluck A (2007) Maxillary necrosis by mucormycosis. a case report and literature review. Med Oral Patol Oral Cir Bucal 12(5):E360-4 (PMID: 17767099)
Viterbo S, Fasolis M, Garzino-Demo P, Griffa A, Boffano P, Iaquinta C, Modica R (2011) Management and outcomes of three cases of rhinocerebral mucormycosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:e69–e74. https://doi.org/10.1016/j.tripleo.2011.04.048
Metzen D, Böhm H, Zimmermann M, Reuther T, Kubler AC, Müller-Richter DA (2012) Mucormycosis of the head and neck. J Craniomaxillofac Surg 40:e321-327. https://doi.org/10.1016/j.jcms.2012.01.015
Brand~ao TB, Gueiros LA, Melo TS, Prado-Ribeiro AC, Alo Nesrallah ACF, Prado GVB & Migliorati CA, (2020) Oral lesions in patients with SARS-CoV-2 infection: could the oral cavity be a target organ ? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 131:e45–e51. https://doi.org/10.1016/j.oooo.2020.07.014
Amorim dos Santos J, Normando AGC, Carvalho da Silva RL, Acevedo AC, De Luca CG, Sugaya N, Guerra ENS (2021) Oral manifestations in patients with COVID-19: a living systematic review. J Dent Res 100:141–154. https://doi.org/10.1177/0022034520957289
Islam MN, Cohen DM, Celestina LJ, Ojha J, Claudio R, Bhattacharyya IB (2007) Rhinocerebral zygomycosis: an increasingly frequent challenge: update and favorable outcomes in two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104(5):e28-34. https://doi.org/10.1016/j.tripleo.2007.06.014. (PMID: 17964469)
Safar A, Marsan J, Marglani O, Al-Sebeih K, Al-Harbi J, Valvoda M (2005) Early identification of rhinocerebral mucormycosis. J Otolaryngol 34(3):166–71. https://doi.org/10.2310/7070.2005.04023. (PMID: 16089219)
Maini Aastha et al (2021) Sino-orbital mucormycosis in a COVID-19 patient: a case report. International Journal of Surgery Case Reports 82:105957
Hoenig M, Seidel D*, Carvalho A, Rudramurthy SM, Arastehfar A, Gangneux JP, Nasir N, Bonifaz A, Araiza J, Klimko N, Serris A, Lagrou K, Meis JF, Cornely OA, Perfect JR, White PL, Chakrabarti A, on behalf of ECMM and ISHAM collaborators (2022) The emergence of COVID-19 associated mucormycosis: a review of cases from 18 countries. Lancet Microbe. Available at: https://ecommons.aku.edu/pakistan_fhs_mc_med_med/657
Damaraju V et al (2023) Isolated tracheobronchial mucormycosis: report of a case and systematic review of literature. Mycoses 66(1):5–12
Fouad YA, Bakre HM, Nassar MA, Gad MOA, Shaat AAK (2021) Characteristics and outcomes of a series of COVID-associated mucormycosis patients in two different settings in Egypt through the third pandemic wave. Clin Ophthalmol 22(15):4795–4800. https://doi.org/10.2147/OPTH.S344937. (PMID:34992339;PMCID:PMC8711239)
Choksi T, Agrawal A, Date P et al (2022) Cumulative mortality and factors associated with outcomes of mucormycosis after COVID-19 at a multispecialty tertiary care center in India. JAMA Ophthalmol 140(1):66–72. https://doi.org/10.1001/jamaophthalmol.2021.5201
El-Kholy NA, El-Fattah AMA, Khafagy YW (2021) Invasive fungal sinusitis in post COVID-19 patients: a new clinical entity. Laryngoscope 131(12):2652–2658. https://doi.org/10.1002/lary.29632. (Epub 2021 May 22. PMID: 34009676; PMCID: PMC8242424)
Janjua OS, Shaikh MS, Fareed MA, Qureshi SM, Khan MI, Hashem D, Zafar MS (2021) Dental and oral manifestations of COVID-19 related mucormycosis: diagnoses, management strategies and outcomes. J Fungi (Basel) 8(1):44. https://doi.org/10.3390/jof8010044. (PMID: 35049983; PMCID: PMC8781413)
Chamilos G, Marom EM, Lewis RE, Lionakis MS, Kontoyiannis DP (2005) Predictors of pulmonary zygomycosis versus invasive pulmonary aspergillosis in patients with cancer. Clin Infect Dis 41(1):60–6. https://doi.org/10.1086/430710. (Epub 2005 May 24 PMID: 15937764)
Agrawal R, Yeldandi A, Savas H, Parekh ND, Lombardi PJ, Hart EM (2020) Pulmonary mucormycosis: risk factors, radiologic findings, and pathologic correlation. Radiographics 40(3):656–666. https://doi.org/10.1148/rg.2020190156. (Epub 2020 Mar 20 PMID: 32196429)
Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SC, Dannaoui E, Hochhegger B, Hoenigl M, Jensen HE, Lagrou K, Lewis RE (2019) Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis 19:e405–e421. https://doi.org/10.1016/S1473-3099(19)30312-3. (Epub 2019 Nov 5. PMID: 31699664; PMCID: PMC8559573)
Acknowledgements
We would like to acknowledge the contributions of the ENT specialists and oral maxillofacial staff for helping us throughout the study.
Funding
This research is self-funded.
Author information
Authors and Affiliations
Contributions
D.G. writing original draft, editing, clinical examination. A.A. data curation, methodology, clinical examination. R.R. visualization, writing—review. A.E. final editing and data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from the Research Ethics Committee, Faculty of Dentistry, the British University in Egypt with approval No. 21–022. The procedures were fully explained to the patients, and they signed an informed consent to share their clinical data and images for scientific purposes. Individual patient’s personal data and results have been kept confidential by filing system with passwords to protect them being preached. Patient’s names were not shown in the analyzed data; instead, they were encoded by coding system known by the main investigator only.
Consent for publication
The procedures were fully explained to all the participants, and they signed an informed consent to share their pictures and clinical data for scientific purposes.
Competing interests
No conflict of interest exists.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ghalwash, D., Abou-Bakr, A., Hussein, R.R. et al. Comorbidities and final outcome of post COVID-19 associated oral mucormycosis patients: a cross-sectional study. Egypt J Otolaryngol 40, 51 (2024). https://doi.org/10.1186/s43163-024-00614-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-024-00614-4