Abstract
Background
The aim of this pilot study was to compare the operation time, intraoperative and postoperative bleeding, postoperative pain, and wound healing of the thulium RevoLix laser tonsillectomy method over the more commonly practiced cold steel tonsillectomy.
Methods
A prospective, single-blinded randomized pilot trial was conducted. Twenty-four adult patients with a mean age of 28.7 years with chronic recurrent tonsillitis were observed and underwent tonsillectomy. The patients were randomly assigned to have one tonsil removed with a thulium RevoLix laser 200, and the conventional cold steel tonsillectomy method was used for the other side.
Results
The tonsillectomy time from incision to hemostasis was 12.08 ± 0.77 (SE) min with the laser method and 10.92 ± 1.31(SE) min with the cold dissection method, with no statistically significant difference (P < 0.121). Intraoperative blood loss in the cold dissection method was 10.92 ± 1.31 ml, and 2.04 ± 1.62 ml was observed during laser treatment (P < 0.000, t = 8.363). In the cold steel tonsillectomy group, the pain score was significantly higher than that in the laser tonsillectomy group on the 7th and 12th postoperative days.
Conclusion
The use of the thulium RevoLix 200 laser for tonsillectomy in the present pilot study of 24 patients showed significantly better outcomes than those in conventional cold dissection methods in terms of intraoperative bleeding and postoperative pain; however, there was no statistically significant difference in other parameters, such as operational time and late postoperative bleeding. A large full-scale prospective study is needed to increase the generalizability and reliability of the results.
Clinical trial registration
ISRCTN16280803, registered on 25 March 2020, https://www.isrctn.com/ISRCTN16280803.
Similar content being viewed by others
Background
Tonsillectomy is one of the most common surgical procedures performed by otolaryngologists, with the number of tonsillectomies performed per year increasing over recent decades [1,2,3,4].
Indications for tonsillectomy in adults include chronic or recurrent tonsillitis, airway obstruction due to hypertrophied tonsils, or any other suspicious tumors of the tonsils [3, 5, 6].
Multiple surgical techniques and instruments with their advantages and disadvantages have been described to minimize intraoperative hemorrhage and reduce the operation time, postoperative pain, and incidence of complications in patients undergoing tonsillectomy [2, 6,7,8,9,10,11,12]. The most common complications of the procedure are intraoperative bleeding, postoperative bleeding, and pain [13,14,15,16].
Cold dissection is the most commonly used tonsillectomy technique, with low postoperative hemorrhage rates [17]. Cold methods include dissection, partial tonsillectomy with microdebrider, guillotine, plasma-mediated ablation, harmonic scalpel, and cryosurgery [18]. Hot tissue preparation involves the use of thermal energy to dissect the space around the tonsil. This includes electrosurgery, coblation, radiofrequency, and laser ablation [19].
There are various comparative studies in the literature to compare tonsillectomy methods used to date and the rates of their major complication [2, 5, 10, 12, 18, 20, 21]. Hot tonsillectomy is believed to cause more postoperative pain but less perioperative bleeding and shorten the operation time [18]. Of the available “hot” methods, laser tonsillectomy has become a new procedure, and the results of laser surgery in recent years suggest an overall improvement [8, 20, 22].
Although numerous articles have been published in general surgery and urology on the use of thulium lasers [23, 24], very few otolaryngology studies are available that specifically address its use for tonsillectomy and compare it with other methods of tonsillectomy. In many studies, researchers have stated that the use of thulium lasers is safe and effective. And in many studies, authors have validated the effectiveness and safety of thulium laser implementation in surgery [23, 24].
The aim of this pilot study was to compare the operation time, intraoperative and postoperative bleeding, postoperative pain, and wound healing of the thulium RevoLix laser method with those of the more commonly practiced cold steel tonsillectomy.
Methods
The prospective, single-blinded randomized pilot trial was conducted from February 2020 to March 2021. The patients were recruited by physician referral from the ENT and Maxillofacial Surgery Department of “Heratsi” №1 University Hospital in Yerevan, Republic of Armenia. The patients with chronic recurrent tonsillitis in remission, who tonsillectomy is indicated, were informed by physician about the ongoing trial. To avoid self-selection bias, the different methods of tonsillectomy were blindly and randomly selected for the same patient on the left or right side.
Informed consent was obtained from all participants after providing written and oral information about the study. The study protocol was approved by the Ethics Committee of Yerevan State Medical University, and the trial “A pilot study of thulium RevoLix laser usage for tonsillectomy” was registered in ISRCTN 16280803 (IRB no. YSMU N 6-1/2020).
The inclusion criteria were adolescents from 16 years and adult patients with the clinical diagnosis of chronic recurrent tonsillitis, since the hospital, where the clinical trial was carried out, is not pediatric and authorized to accept patients from 16 years old (from pre-conscription age). Twenty-four patients (14 males and 10 females) with chronic recurrent tonsillitis were observed and underwent tonsillectomy. Sample size was calculated twice based on power (1-β = 0.8) and alfa 0.05, standard deviations and desirable observed differences for intraoperative time (estimated size 10 people), and bleeding (estimated size 11).
The formula used for sample size calculation is as follows:
With some precaution, we selected sample sizes of n = 24 patients. All participants provided informed consent for trial participation after providing written and oral information about the study
The exclusion criteria were as follows: (1) bleeding diathesis, (2) poor anesthetic risk, (3) uncontrolled medical illness, (4) anemia, or (5) acute infection.
All recruited patients underwent surgery under general anesthesia by the same surgeon.
The method of removal of each tonsil was blindly randomly assigned to have one tonsil removed with a thulium RevoLix laser 200 (manufacturer: LISA laser products, Germany: serial number PTK-MCL#116), and the conventional cold steel tonsillectomy method was used for the other side. The thulium RevoLix laser 200 has a wavelength of 2.0 µm and is used for incision and vaporization. The RevoLix laser beam is delivered by flexible laser fibers. A power of 8 W was used for laser tonsillectomy in all cases.
The hospital stay was 2–4 days for all patients, with an outpatient follow-up of 12 days. The end of participation was elected on the 13th postoperative day. All patients used the same medications for 12 postoperative days. Outcome measures included the following:
-
1.
Intraoperative blood loss quantified by measuring suction bottle fluid and weight measurement of surgical sponges
-
2.
Time taken for surgery, which was measured from the beginning and finishing of tonsillectomy on each side
-
3.
Postoperative pain was measured by a numerical rating scale (NRS) from 0 to 10 at 2, 5, 7, and 10 days postoperatively.
-
4.
Postoperative bleeding was assessed by the effectiveness of the management strategy (no therapy, clot suction, direct pressure, or electrocautery) immediately after operation until 12th post-operational days.
-
5.
Time taken for complete healing was compared on both tonsillectomy sides by serial direct clinical examinations at 5, 7, and 12 days postoperatively.
Statistical analysis was performed using the SPSS 16.0 statistical package. Normal distribution of data was assessed using the Kolmogorov-Smirnov test. For comparison of means if the data were normally distributed, independent samples, two-sided Student’s t-test was applied. For analysis of intraoperative blood loss, a one-sample t-test was performed. In the case of an asymmetric distribution (only PLas day 12), a nonparametric two-sided Mann-Whitney test was used. In all cases, differences were considered significant at the P < 0.05 level.
Results
All patients undergoing tonsillectomy were Armenians with a mean age of 28.7 years (range, 17–42 years).
The tonsillectomy time from incision to hemostasis was 12.08 ± 0.77 (SE) min with the laser method and 10.92 ± 1.31 (SE) min with the cold dissection method, with no statistically significant difference (P = 0.121) (n = 24; two-sided two independent group t-test). Intraoperative blood loss in the cold dissection method was 10.92 ± 1.31 ml (SE), and 2.04 ± 1.62 ml blood loss was observed during laser treatment (P < 0.001, one group two-sided t-test; t = 8.363; n = 24).
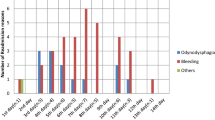
On the 2nd, 5th, 7th, and 12th days, pain intensity was recorded using the numeric rating pain scale. The mean pain severity on the second day after surgery was 5.7 ± 0.54 (SE) on the laser side and 7.25 ± 0.46 (SE) on the cold dissection side, with a significant difference (P = 0.037; n = 24). No significant difference was found between pain intensity on the 5th day after surgery between the laser (3.9 ± 0.49; SE) and cold dissection (5.58 ± 0.66; SE) methods (P = 0.055; n = 24). On the 7th and 12th postoperative days, the pain severity decreased on both sides, but laser tonsillectomy showed significantly lower pain severity values than cold steel dissection (Table 1).
No significant difference was detected in the comparison of the patients’ sex with bleeding rate during surgery and pain intensity after surgery.
No postoperative bleeding was observed on either side in the postoperative period; thus, there was no need for any management.
Wound healing was assessed visually on the 5th, 7th, and 12th postoperative days. On the fifth postoperative day, on the laser tonsillectomy sides, the fibrin plaque was softer and less remarkable. On the cold steel tonsillectomy sides, the fibrin plaque was whitish and more pronounced (Fig. 1).
On the 7th postoperative day, on the laser tonsillectomy side, the fibrin plaque somewhere was sloughing off and covered with newly formed epithelial tissue. On the cold dissection sides, the fibrin plaque was somewhat sloughed off and had somewhat of a green-gray color (Fig. 2).
On the 12th postoperative day, on the hot dissection side, almost full epithelization was observed. On the cold dissection side, fibrin plaques existed in some islands, and the main surface was closed with newly formed epithelial tissue (Fig. 3).
Discussion
Tonsillectomy is one of the most common surgeries in the field of otolaryngology and is often performed to treat recurrent tonsillitis or upper airway obstruction caused by tonsil hypertrophy [1, 5, 6, 12, 22].
There are many methods for removing tonsils as described in the literature, and the main goal of new research methods and their clinical application is to reduce the incidence of intraoperative and postoperative complications [3, 22]. Nowadays, the methods of tonsillar surgery continue to evolve [18]. There are several methods of tonsillectomy, which can be divided into cold and hot. Technological innovations are focused on a bloodless surgical field, reduced operation time, reduced postoperative pain, and increased healing rate, accessibility, and safety [18]. There is a great deal of discussion about the relative merits of the various methods [4, 6, 10,11,12, 22]. The cost of equipment used for different techniques varies, although the time of operation is an important factor in the cost of tonsillectomy [18].
Cold dissection is the most commonly used tonsillectomy technique and is still the most practiced technique, especially in the developing world [17, 18]. This technique uses stainless steel scissors and scalpels, serrated forceps, and a herd dissector/retractor to separate all of the tonsil tissue from its capsule and expose the underlying compressive muscles [18].
Of the available “hot” techniques, laser tonsillectomy has become a new procedure [8]. In 1994, Krespi and Ling [25] introduced the concept of bloodless tonsillectomy with a laser. The CO2 laser as an excellent cutting tool plays a valuable role in otolaryngological practice. Linder et al. [9] in 1999 suggested the use of laser for tonsillotomy. This causes less bleeding, less pain, and discomfort and is a day case procedure. However, more secondary bleeding and postoperative pain were noted with the laser.
The RevoLix laser has a wavelength is 2 µm and was specifically developed for soft tissue surgery. This wavelength is similar to holmium, but the radiation is continuous, not pulsed. The RevoLix laser beam is delivered by flexible laser fibers, which is ideal for endoscopic, laparoscopic, open, and minimally invasive surgery. Incision and vaporization of tissue are similar to CO2 laser technology. Unlike green lasers, the effectiveness of RevoLix vaporization does not decrease during surgery, since the absorbing chromophore is water, and the effect of the laser on tissues does not depend on their vascularization [26, 27]. Excessive laser radiation does not damage tissue more than 3 mm from the fiber tip, and tissue damage is limited to 0.2–1.0 mm. The optical penetration of RevoLix in tissue is app. 0.25 mm [24]. Neither bleeding nor visible laser glare affects the vision of the surgical site; thus, the visualization is quite well [24, 26, 27].
In the present study, the mean surgery time for the RevoLix laser technique was 12.08 ± 0.77 (SE) min (range, 9.0–16.0 min), which is nonsignificantly longer than that for cold steel tonsillectomy (10.92 ± 1.31 (SE) min, range 6.00–15.00 min, P = 0.121).
The most common complication of tonsillectomy is bleeding during or after surgery [15, 16]. Despite the surgeon’s best efforts to prevent it, bleeding remains the most serious complication after tonsillectomy [13, 15, 16]. Windfuhr et al. [1] reported that the rate of primary hemorrhage (within 24 h of surgery) ranged from 0.2 to 2.2%, whereas secondary hemorrhage (24 h after surgery) ranged from 0.1 to 3%.
Ahmed and Arya [8] performed systematic reviews and meta-analyses comparing laser tonsil surgery with other techniques, and a total of 14 articles were evaluated. A variety of laser techniques were used, including CO2 (66%), potassium-titanyl-phosphate (19%), and contact diodes (15%). Nonlaser techniques included dissection (62%), diathermy (20%), and coblation (18%). The generalized findings suggest that laser techniques are superior to intraoperative bleeding and procedure time. Laser techniques also provide inconsistent or superior results in terms of postoperative bleeding, pain, and overall healing time. In the present study, there was the mean 2.04 ± 1.62 ml (SE) (min 0.3 ml, max 2.5 ml) intraoperative bleeding in laser surgery, and the mean bleeding in cold steel tonsillectomy was 10.92 ± 1.31 ml (SE) (min 6 ml, max 20 ml). There was no case of postoperative bleeding in the presented study patients.
Local pain after surgery is a significant disadvantage of tonsillectomy. However, Wiltshire et al. [11] reported significant postoperative pain relief and faster return to normal food intake when using coblation. Since then, several other studies have shown varying results. Arbin et al. [7] reported no significant difference in pain scores among 60 patients who underwent either bipolar diathermy scissors tonsillectomy (higher temperature dissection) or harmonic scalpel tonsillectomy (lower temperature dissection). However, Hegazy et al. [20] found that potassium titanyl phosphate laser avoided immediate postoperative pain when compared with the bipolar radiofrequency technique but caused more late postoperative pain.
In the present pilot study, the highest NRS pain scores were revealed in the second post-op day, which slightly decreased over the next 12 post-op days in both groups. In the cold steel tonsillectomy group, the pain score was significantly higher than that in the laser tonsillectomy group on the 7th and 12th postoperative days: 1.67 ± 0.33 via 4.00 ± 0.69 (SE) (P = 0.006; n = 24) on the 7th postoperative day and 0.17 ± 0.11 via 2.67 ± 0.73 (SE) (P = 0.003; n = 24) on the 12th postoperative day.
Piitulainen et al. [4] determined that the duration of postoperative recovery depends on three endpoints: pain at rest, pain on swallowing, and regular use of analgesics. In the present study, wound repair was assessed by the time taken for complete healing, and both tonsillectomy sides were compared by serial direct clinical examinations at 5, 7, and 12 postoperative days.
Only a few studies have compared wound healing after different tonsillectomy methods [26, 27]. As noted by Isaacson [28], epithelial ingrowth beneath a fibrin clot begins shortly after wounding. The separation of the fibrin clot approximately 7 days after surgery exposes the vascular stroma. Involution of the vascular stroma and completion of epithelial coverage correlated with a reduction in pain levels and a reduced risk of bleeding. The tonsillar fossa healing in the present pilot study was faster on the laser tonsillectomy sides than on the cold dissection sides. On the 7th postoperative day on the laser tonsillectomy side, the fibrin layer partially sloughed off, and underlying tissue covered with newly formed epithelial tissue was observed. On the 12th post-op day, full epithelization of a tonsillar fossa was visualized on the laser dissection side. On the cold dissection side, the fibrin layer still existed in some islands, although the main surface was closed with newly formed epithelial tissue.
Study limitations
The study was performed in adult patients, but complementary studies are needed to confirm the use of this method as a standard protocol for tonsillectomy in all age groups. Despite the benefits of the RevoLix laser technique, the higher cost of the thulium RevoLix 200 system should be considered. A large full-scale randomized controlled trial is needed to increase the generalizability and reliability of the results.
The presented pilot study can be used to evaluate the feasibility of recruitment, randomization, and retention, comparative assessment of proposed methods, and implementation of the novel intervention with a thulium RevoLix laser.
Conclusions
The use of the thulium RevoLix 200 laser for tonsillectomy in the present pilot study of 24 patients showed significantly better outcomes than those in conventional cold dissection methods in terms of intraoperative bleeding and postoperative pain; however, there was no statistically significant difference in other parameters, such as operational time and late postoperative bleeding. A large full-scale prospective study is needed to increase the generalizability and reliability of the results.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon request.
References
Windfuhr JP, Toepfner N, Steffen G, Waldfahrer F, Berner R (2016) Clinical practice guideline: tonsillitis II. Surgical management. Eur Arch Otorhinolaryngol 273:989–1009
Pynnonen M, Brinkmeier JV, Thorne MC, Chong LY, Burton MJ (2017) Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev 8(8):CD004619
Torres BPG, García FDM, Orozco JW (2018) Tonsillectomy in adults: analysis of indications and complications. Auris Nasus Larynx 45:517–521
Piitulainen JM, Uusitalo T, Sjöblom HM, Ivaska LE, Jegoroff H, Kauko T et al (2022) Intracapsular tonsillectomy in the treatment of recurrent and chronic tonsillitis in adults: a protocol of a prospective, single-blinded, randomised study with a 5-year follow-up (the FINITE trial). BMJ Open 12:e062722
Karimi E, Safaee A, Bastaninejad S, Dabiran S, Masoumi E, Salehi FM (2017) A comparison between cold dissection tonsillectomy and harmonic scalpel tonsillectomy. Iran J Otorhinolaryngol 29:313–317
Zhou X, Xu A, Zhen X, Gao K, Cui Z, Yue Z et al (2019) Coblation tonsillectomy versus coblation tonsillectomy with ties in adults. J Int Med Res 47:4734–4742
Arbin L, Enlund M, Knutsson J (2017) Post-tonsillectomy pain after using bipolar diathermy scissors or the harmonic scalpel: a randomised blinded study. Eur Arch Otorhinolaryngol 274:2281–2285
Ahmed J, Arya A (2021) Lasers in tonsillectomy: revisited with systematic review. Ear Nose Throat J 100:14S–18S
Linder A, Markström A, Hultcrantz E (1999) Using the carbon dioxide laser for tonsillotomy in children. Int J Pediatr Otorhinolaryngol 50:31–36
Magdy EA, Elwany S, El-Daly AS, Abdel-Hadi M, Morshedy MA (2008) Coblation tonsillectomy: a prospective, double-blind, randomised, clinical and histopathological comparison with dissection–ligation, monopolar electrocautery and laser tonsillectomies. J Laryngol Otol 122:282–290
Wiltshire D, Cronin M, Lintern N, Fraser-Kirk K, Anderson S, Barr R et al (2018) The debate continues: a prospective, randomised, single-blind study comparing coblation and bipolar tonsillectomy techniques. J Laryngol Otol 132:240–245
Basu S, Sengupta A, Dubey AB, Sengupta A (2019) Harmonic scalpel versus coblation tonsillectomy a comparative study. Indian J Otolaryngol Head Neck Surg 71:498–503
Windfuhr JP, Deck JC, Remmert S (2005) Hemorrhage following coblation tonsillectomy. Ann Otol Rhinol Laryngol 114:749–756
Bhattacharyya N, Kepnes LJ (2014) Revisits and postoperative hemorrhage after adult tonsillectomy. Laryngoscope 124:1554–1556
Hsueh WY, Hsu WC, Ko JY, Yeh TH, Lee CH, Kang KT (2019) Postoperative hemorrhage following tonsillectomy in adults: analysis of population-based inpatient cohort in Taiwan. Auris Nasus Larynx 46:397–406
Liu Q, Zhang Y, Lyu Y (2021) Postoperative hemorrhage following coblation tonsillectomy with and without suture: a randomized study in Chinese adults. Am J Otolaryngol 42:102760
Ahmad MU, Wardak AN, Hampton T, Siddiqui MRS, Street I (2020) Coblation versus cold dissection in paediatric tonsillectomy: a systematic review and meta-analysis. J Laryngol Otol 134:197–204
Verma R, Verma RR, Verma RR (2017) Tonsillectomy-comparative study of various techniques and changing trend. Indian J Otolaryngol Head Neck Surg 69:549–558
Metcalfe C, Muzaffar J, Daultrey C, Coulson C (2017) Coblation tonsillectomy: a systematic review and descriptive analysis. Eur Arch Otorhinolaryngol 274:2637–2647
Hegazy HM, Albirmawy OA, Kaka AH, Behiry AS (2008) Pilot comparison between potassium titanyl phosphate laser and bipolar radiofrequency in paediatric tonsillectomy. J Laryngol Otol 122:369–373
Lieberg N, Aunapuu M, Arend A (2019) Coblation tonsillectomy versus cold steel dissection tonsillectomy: a morphological study. J Laryngol Otol 133:770–774
Chung JEREW, van Geet R, van Helmond N, Kastoer C, Böhringer S, van den Hout WB et al (2022) Time to functional recovery after laser tonsillotomy performed under local anesthesia vs conventional tonsillectomy with general anesthesia among adults: a randomized clinical trial. JAMA Netw Open 5:e2148655
Cui D, Sun F, Zhuo J, Sun X, Han B, Zhao F et al (2014) A randomized trial comparing thulium laser resection to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: four-year follow-up results. World J Urol 32:683–689
Sun F, Han B, Cui D, Zhao F, Sun X, Zhuo J et al (2015) Long-term results of thulium laser resection of the prostate: a prospective study at multiple centers. World J Urol 33:503–508
Krespi YP, Ling EH (1994) Laser-assisted serial tonsillectomy. J Otolaryngol 23:325–327
Kim JW, Moon DG (2011) Basic principles of laser for prostate surgery. Korean J Androl 29:101–110
Davidoss NH, Eikelboom R, Friedland PL, Maria PLS (2018) Wound healing after tonsillectomy – a review of the literature. J Laryngol Otol 132:764–770
Isaacson G (2012) Tonsillectomy healing. Ann Otol Rhinol Laryngol 121:645–649
Acknowledgements
We greatly acknowledge Dr. Garo M. Tertzakian for providing the RevoLix 200 thulium laser and technical support to “Heratsi” №1 hospital complex of YSMU.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Author information
Authors and Affiliations
Contributions
MB, conceptualization and methodology. GM, writing—original draft preparation. MM, visualization and investigation. VV, data curation and software. AT, statistics and validation. AB, software and supervision. AP, writing—reviewing and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was conducted in accordance with relevant ethical standards, and the study protocol was approved by the Yerevan State Medical University Ethics Committee (IRB no. YSMU N 6-1/2020). Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
Written informed consent for publication of their clinical details and/or clinical images was obtained from the patients.
Compseting interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baghdasaryan, M.K., Mkhitaryan, G.K., Misakyan, M.S. et al. Thulium laser versus cold steel tonsillectomy: a prospective pilot study in adult patients. Egypt J Otolaryngol 40, 26 (2024). https://doi.org/10.1186/s43163-024-00584-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-024-00584-7