Abstract
The human voice is commonly affected by hormonal changes, both in physiological and pathological conditions. Voice changes were reported in a number of endocrine disorders, and dysphonia may be the initial sign of these disorders. A number of studies documented endocrine-related voice changes utilizing both subjective and objective voice assessment tools. The objective of the present review is to draw the phoniatrician’s attention to the wide variety of typical changes, as well as the potential for hormonal imbalances that may affect the voice, in order to identify them promptly and generate proper treatment and referrals.
Similar content being viewed by others
Background
The endocrine system is composed of glands that release hormones into the bloodstream. These hormones are carried via the blood to their target cells. The hormone's interaction with its receptor (located on the cell surface) sets off a series of biochemical events in the target cell that ultimately modify the cell's activity or function [1]. The major endocrine glands are illustrated in Fig. 1 and include:
Schematic representation of the location of the major hormone-producing (i.e., endocrine) organs in the body. (For the purposes of illustration, both male and female endocrine organs are presented here) [1]
-
The hypothalamus (which releases Corticotropin-releasing hormone, Gonadotropin-releasing hormone, Thyrotropin-releasing hormone, Growth hormone-releasing hormone, Somatostatin, and Dopamine).
-
The pituitary gland (the anterior pituitary releases Adrenocorticotropic hormone, Luteinizing hormone, Follicle-stimulating hormone, Thyroid-stimulating hormone, Growth hormone, and Prolactin, whereas the posterior pituitary releases Vasopressin and Oxytocin).
-
The adrenal cortex (which releases Cortisol and Aldosterone).
-
The testes (which release Testosterone).
-
The ovaries (which release Oestrogen and Progesterone).
-
The thyroid gland (which releases Thyroid hormones and Calcitonin).
-
The parathyroid glands (which release Parathyroid hormone).
-
The pancreas (which releases Insulin and Glucagon) [1].
The human voice is very sensitive to endocrine changes, with various endocrine changes affecting the voice throughout the normal human life cycle [2]. The detection of androgen, oestrogen, and progesterone, in addition to thyroid hormone receptors in the human vocal fold (VF), may provide evidence to the hypothesis that variations in vocal quality are caused by hormonal influences [3,4,5].
The phoniatrician must be familiar with the wide variety of typical changes, as well as the potential for hormonal imbalances that may affect the voice, in order to identify them promptly and generate proper treatment and referrals [2].
Evaluation of voice disorders
It is ideal to obtain a thorough case history and conduct the following battery of tests when examining individuals with voice abnormalities in order to characterize the disorder's impact on all relevant mechanisms and dimensions: auditory perceptual assessment, laryngeal endoscopy, acoustics, aerodynamics, and patients' self-perception of how voice issues affect their daily function are among the other factors to consider [6,7,8,9,10].
As stated by Kotby [11], the voice evaluation protocol proceeds through three levels:
-
(1)
Elementary procedures: which encompasses thorough history-taking (including vocal habits, occupation, onset, course, and duration of dysphonia), and auditory perceptual assessment (APA) of the voice with ENT and laryngeal inspection. Subjective voice assessment could also be achieved by using questionnaires such as the voice handicap index [12].
-
(2)
Clinical aids: this level includes videolaryngostroboscopy using either a rigid 90° laryngoscope or a flexible nasolaryngoscope. Stroboscopic examination allows the observation of the mucosal wave, amplitude of VF vibration, symmetry and periodicity, glottis closure, and ventricular folds.
High-fidelity voice recordings in a sound-treated room should be used for APA's documentation in order to reduce background noise. The recorded material is rated using the modified GRBAS "Grade, Roughness, Breathiness, Asthenia, Strain" scale with 4 grades from 0 "normal" to 3 "severe dysphonia" for describing the grade and character of dysphonia.
-
(3)
Additional measures: this includes acoustic analysis (e.g., shimmer, jitter, and harmonic to noise "H/N" ratio) and aerodynamic analysis (e.g., maximum phonation time "MPT") of voice.
Effects of sex hormones on voice throughout life
Voice is regarded as a crucial secondary sexual characteristic that gives a unique impression to a person's character and personality [3]. The voice alters in response to changing sex hormones throughout life. The first and most noticeable changes occur for both sexes at puberty, when hormonal changes lead the male voice to drop by even one octave and the female voice to drop by one-third [2, 13]. At puberty, the dimensions of the male's vocal tract and larynx increase, and VFs become thicker and longer, lowering the fundamental frequency of the voice. In contrast, the female's vocal tract and VFs are shorter, resulting in their brighter voice timbre and higher voice pitch [14].
Males experience a more pronounced initial pubertal voice change but then have relatively stable circulating levels of sex hormones across their life span and undergo fewer subsequent voice changes. In females, cyclic voice and laryngeal changes occur with each menstrual cycle, and a second permanent change occurs at menopause [2].
Voice changes in the premenstrual days are common and known as dysphonia premenstrualis. The most frequent voice symptom reported by female singers was difficulty singing high notes [15]. Other commonly reported vocal symptoms were vocal fatigue, changes in voice quality, and reduced vocal range [2]. Female opera singers were excused from performance in the premenstrual and early menstrual days, a practice named “grace days” [16].
In the premenstrual period, oestrogen and progesterone work together to relax smooth muscles, which induces venodilatation. Moreover, polysaccharides break down into smaller molecules in the vocal folds (VFs) and bind water, enhancing fluid retention. These changes result in vocal fold congestion and edema [2]. Progesterone also causes mucosal dryness by increasing epithelial desquamation and decreasing mucous secretions at the vocal fold edges [13].
Some studies provided evidence of the direct effect of sex hormones on the VFs’ tissue. Abitbol et al. [13] demonstrated that a woman's normal menstrual cycle resulted in noticeable alterations in both superficial laryngeal and vaginal smears. Surprisingly, at each phase of the cycle, the smears from the cervix and larynx were indistinguishable. This work has been supported by the localization of oestrogen, progesterone, and androgen receptors in both the mucosa and deeper tissues of the larynx [2, 17, 18]. Using narrow band imaging, Shoffel-Havakuk et al. [19] demonstrated increased laryngeal vascular congestion during the premenstrual period consistent with the progesterone peak (Fig. 2).
Different events of the menstrual cycle and corresponding laryngeal changes as seen by narrow band imaging [19]
On the other hand, Chae et al. [20] and Ryan & Kenny [21] suggested the role of secondary effects of premenstrual syndrome (PMS)-related mood variations and abdominal spasms on voice. Both could result in laryngeal muscle tension or a decrease in respiratory effort, signifying that females suffering from PMS have a greater tendency for premenstrual dysphonia [19].
It is thought that the greater susceptibility of females to microvascular VF lesions, including ectasias and varices, is related to the female hormonal cycle and hormonal variations. Care should be taken as the presence of these microvascular lesions increases the risk for VF haemorrhage [22].
Pregnancy-related voice changes may be similar to those encountered premenstrually [23]. The main vocal complaints were breathiness and vocal fatigue, especially in the third trimester [24,25,26]. During pregnancy, the oestrogen and progesterone levels are significantly increased [27]. This leads to variable degrees of edema and congestion of the VFs' mucosa, as detected by laryngoscopy [28] and high-speed digital imaging [27]. Aggravated laryngopharyngeal reflux could also play a role [26]. Pregnancy-induced rhinitis affects about 22% of females [29], and negatively affects the voice due to the dehydrated VF mucosa subsequent to mouth breathing [30].
A significant decrease in MPT during the third trimester of pregnancy was observed in a number of studies [26, 27, 31, 32]. As explained by Cassiraga et al. [31], the diaphragm moves up during the third trimester, causing upper chest breathing. This results in poor respiratory support and a reduction of MPT. Ulkumen et al. [33] compared certain voice parameters in the third trimester with the third month postpartum and found a significant increase in MPT in the third month postpartum.
In the majority of studies of gestational voice changes [26, 32, 34], no significant changes were reported in acoustic and aerodynamic parameters during the first and second trimesters of pregnancy. On the other hand, Li and Xu [28] mentioned that the fundamental frequency of the voice is significantly decreased in some pregnant women, predominantly during the second trimester, and particularly with male fetuses. The authors found that, at 2-year follow-up, the pitch increased in most cases but did not return to normal levels and recommended further study to elucidate the cause.
In light of these findings, it would be reasonable to educate pregnant women about poor vocal habits and vocal hygiene, mainly in the third trimester. Breathing exercises and professional voice support during pregnancy would be of special importance to professional voice users, particularly singers [33].
After menopause, the relative increase of androgens together with the marked drop in oestrogen and progesterone levels may cause vocal fold thickening with a slight decrease in the vocal pitch [35]. Other observable post-menopausal voice alterations include vocal fatigue, reduced vocal range, and failure to reach high notes. Professional vocalists are more attentive to these changes [36]. Most vocal abnormalities in postmenopausal females have been proven to be reversed by hormone replacement therapy (HRT) [37]. The studies of D’haeseleer et al. [38] and Hamdan et al. [39] indicated that menopausal women on HRT have a higher habitual pitch compared to those not on HRT, demonstrating the counter effect of oestrogen replacement on the VFs. It is well known that oestrogen markedly increases the glandular secretions above and below the VF edges, enhancing mucosal viscosity. It also improves VF capillary permeability, promoting better tissue oxygenation [13]. Proper counseling and cautious consideration of the risks and benefits of HRT are strongly recommended for professional voice users approaching menopause.
In males, aging is associated with a progressive thinning of the vocal folds. After the age of 30, a decline in serum testosterone levels occurs by 1% per year. The resultant sarcopenia in aged males over 65 years affects the vocalis muscle, leading to VF bowing and reduced glottic closure with perceived breathiness [40, 41]. Additionally, elevated fundamental frequency is perceived with vocal feminization [35].
Voice changes in reproductive disorders
Polycystic Ovarian Syndrome (PCOS) is the most prevalent endocrinopathy among middle-aged women [42]. Anovulation and hyperandrogenism can lead to marked virilization. Although hirsutism, oily skin, and acne are most common, androgen-mediated vocal changes can also occur [2]. Nygren et al. [43] hypothesized that high levels of androgens can result in hypertrophy of the thyroarytenoid muscle, which coincides with a lowered vocal pitch. Hannoun et al. [44] reported increased incidence of throat clearing, deepening of voice, and decreased maximum phonation time among patients with PCOS. In a group of patients with PCOS, laryngeal abnormalities such as impaired VF vibration, incomplete glottic closure configuration, and supraglottic hyperfunction (reflecting a deviant muscle tension pattern) were found to be significantly more common, according to a study by Aydin et al. [45].
Although psychogenic causes are more common, hypogonadism in males (resulting from anomalies of the gonads) can lead to puberphonia (a.k.a. incomplete mutation or mutational falsetto) [46, 47]. Failure to adopt the lower-pitched voice of adulthood is the defining feature of puberphonia. In addition to an unusually high pitch, common signs include a breathy, weak voice, reduced loudness, and pitch breaks [48, 49].
Exogenous androgens (e.g., anabolic steroids) should be avoided in females if there are any appropriate therapeutic alternatives. In clinical practice, these drugs are most frequently used for treating endometriosis or (illicitly) to improve athletic performance [50, 51], as well as in female to male transgender patients [2]. Exogenous androgens produce instability of the female voice and increased muscle mass of the VFs, leading to a drop in fundamental voice frequency and deep voice [47, 50, 52]. These changes are often irreversible, and can occur within weeks of the initiation of androgens [2].
Androgenic progesterone-containing oral contraceptives were reported to change voice character and range deleteriously after only a few months of starting therapy and may permanently masculinize the voice [53, 54]. Modern formulations of oral contraceptives use much lower hormone doses, and voice changes have not been reported [55]. In fact, current oral contraceptive formulations tend to reduce hormonal fluctuations throughout the menstrual cycle, stabilizing the singing voice [56].
Voice changes in thyroid and parathyroid gland disorders
Thyroid gland disorders can result in laryngeal dysfunction either through hormonal effects or due to local effects on the recurrent laryngeal nerves (RLNs) or surgery [2].
A) Voice changes related to hormonal disturbances
According to McIvor et al. [57], up to one-third of thyroid disease patients present with dysphonia. Thyroid hormone receptors, TR alpha and beta, have been detected in the fibrous lamina propria, cartilage, and glands of the human larynx. These receptors may contribute to the voice changes associated with thyroid dysfunction [4].
Hypothyroidism is a well-known cause of voice problems [36]. Chronic autoimmune thyroiditis, "also known as Hashimoto’s disease", is the most frequent cause of primary hypothyroidism in well-developed countries (without iodine deficiency). Other less common causes are iodine deficiency, thyroidectomy, or radioiodine treatment [58]. The clinical manifestations of hypothyroidism include weight gain, persistent fatigue, cold intolerance, hair loss, skin dryness, menstrual disturbances, voice alterations, and myxedema [59].
Up to 80% of patients with hypothyroidism may have voice complaints, with the frequency of voice problems increasing with more severe hypothyroidism [60]. The voice change is sometimes the main complaint of the patient [47]. Dysphonia, vocal fatigue, softening of the voice, reduced voice range, and globus sensation may be observed even in mild hypothyroidism. The mechanism of voice changes associated with hypothyroidism is not completely understood, especially in cases of mild hypothyroidism [2]. Ritter [61] demonstrated an increased level of acid mucopolysaccharides submucosally in the vocal folds in hypothyroidism. These excess mucopolysaccharides most likely act to increase the osmolality of the lamina propria, increasing its fluid content. This results in increased vocal fold mass and decreased vibration, leading to a deep irregular voice [47]. In some cases, changes similar to Reinke’s edema may be apparent [2].
In severe hypothyroidism with myxedema, these changes are more intense and may be associated with paresis of the VFs due to the thyroid gland expansion, cricothyroid muscle oedema, and vagus nerve edema [36]. Moreover, hypothyroidism may influence voice function by affecting the breathing control system, diaphragmatic muscle function, or goitre-induced obstruction of the upper airway [62]. The voice alterations reverse completely within three to six months after achieving euthyroidism [36]. As shown by Birkent et al. [63], the voice fundamental frequency of 24 hypothyroid women treated with thyroid hormone replacement therapy and brought into an euthyroid state significantly improved from a pretreatment value of "223.48 ± 36.10" Hz to "237.64 ± 38.31" Hz.
Thyrotoxicosis refers to the clinical condition of excessive circulating thyroid hormones, regardless of the source, while hyperthyroidism results from increased thyroid hormone production and secretion from the thyroid gland. The commonest cause of hyperthyroidism (thyrotoxicosis with hyperthyroidism) is Graves’ disease, followed by toxic nodular goitre. Thyrotoxicosis (without hyperthyroidism) is most commonly caused by excess intake of the thyroid hormone medication or results from the release of preformed thyroid hormones due to thyroiditis [64]. The clinical manifestations of thyrotoxicosis comprise palpitations, fatigue, tremors, increased sweating, heat intolerance, nervousness, and weight loss [64, 65].
Mild hyperthyroidism usually does not cause voice problems. In more severe cases, muscle weakness, dehydration, and tremor all contribute to voice changes. Physiologic alterations in the laryngeal structure could also take place [2]. The most commonly reported voice changes include tremulous, breathy voice, and reduced loudness [66]. The general weakness and fatigue due to hyperthyroidism affect respiratory and laryngeal muscles, causing asthenic voice with a low H/N ratio and reduced MPT [67, 68]. The vocal behavior may reflect the anxiety element of the disease [47]. Kovacic [67] also reported that female patients with hyperthyroidism demonstrated reduced fundamental frequency and deep voice.
Voice dysfunctions in parathyroid gland diseases are caused by a general effect. Hypocalcaemia in hypoparathyroidism results in laryngospasm and other symptoms of neuromuscular irritability. On the other hand, hypercalcaemia in hyperparathyroidism leads to muscle weakness and easy fatigability [69, 70].
B) Voice changes related to local effects or surgery
The close anatomic relationship between the thyroid gland and the recurrent and superior laryngeal nerves places these nerves at risk when the thyroid gland is involved with structural or inflammatory disorders. Structural thyroid disorders, including locally infiltrating thyroid carcinoma and huge compressive goiter may affect the voice by stretching the nerves, causing vocal fold paresis or paralysis, or by invasion or compression of the larynx or trachea. Large thyroid masses can also impact voice by impairing vertical laryngeal motion. Neuropraxia of the recurrent or superior laryngeal nerves can result from inflammatory conditions of the thyroid gland, such as Hashimoto's thyroiditis [2, 71].
A hyperplastic parathyroid gland as well as a parathyroid carcinoma can lead to vocal fold paralysis due to recurrent laryngeal nerve involvement [72, 73].
Surgical Considerations
Recurrent Laryngeal Nerve (RLN) Paralysis and Paresis
Recurrent laryngeal nerve paralysis and paresis is the most feared complication of thyroid surgery, and may be unilateral or bilateral. However, such complication rarely occurs when the surgery is performed with nerve monitoring by an experienced thyroid surgeon [74, 75].
Unilateral vocal fold paralysis (UVFP) results in breathy voice quality, diplophonia, reduced loudness, short phonation duration, and a restricted pitch range [76]. Supraglottic hyperfunction is common, leading to a low-pitched, irregular voice [77].
Laryngoscopic examination in UVFP might reveal shortened and bowed VF [78]. Slight VF adduction on phonatory effort might be caused by the action of interarytenoid muscle still innervated partially from the contralateral nerve or by the intact cricothyroid muscle [79]. Arytenoid cartilage prolapse suggests intense denervation with loss of muscular support [80]. In longstanding UVFP with supraglottic hyperfunction, maneuvers such as humming permit a more in-depth evaluation of the glottic closure by causing the ventricular folds to relax [81]. On stroboscopic examination, the paralyzed VF shows wide undulating amplitudes "like the fluttering of a flag in the wind" (though amplitude could be reduced) and a loss of mucosal waves. Phase and amplitude asymmetry is obvious between the normal and paralyzed side with incomplete glottic closure [82].
External Branch of the Superior Laryngeal Nerve (EBSLN) Paralysis and Paresis
EBSLN injury causes a low pitched, weak voice that easily fatigues [57, 83,84,85]. Singers and professional voice users often complain of impairment in the production of high pitches and variations of speaking fundamental frequency [86].
Strobovideolaryngoscopic findings of EBSLN injury are controversial and may include VF bowing, ipsilateral glottal rotation, lack of brisk adduction and abduction, VF lag on the affected side, lower displacement of the affected VF with scissoring, and decreased amplitude and mucosal wave of the affected VF. In addition, a posterior glottic gap may be observed, although this is classically seen in concurrent RLN injury [57, 83,84,85]. These subtle clinical signs can be further highlighted by asking the patient to perform certain vocal maneuvers. Rubin et al. [87] claimed that VF lag (sluggishness), especially during repetitive phonatory tasks (e.g., /i/-/hi/-/i/-/hi/-/i/-/hi/), was a hallmark of SLN injury, clarifying that paretic nerves fatigue more quickly than normal nerves. Phonation in low pitch followed by phonation in high pitch is another simple and accurate diagnostic procedure for unilateral SLN paralysis. This task results in oblique glottis caused by posterior glottis rotation to the paralytic side [83, 88]. Roy et al. [89] identified epiglottic petiole deviation to the paralytic side during high-pitched phonation as a possible diagnostic marker of unilateral EBSLN denervation (Fig. 3).
Paresis of external branch of superior laryngeal nerve (ESLN) on right side [89]: A During vocal fold abduction, petiole is in midline. B During phonation produced at normal pitch and loudness, petiole remains in midline. C During phonation elicited at highest pitch during upward glissando maneuver, epiglottic petiole deviates to right side (arrow)
Non-neural Dysphonia
Post-operative dysphonia is sometimes seen, even in the absence of neural injury [36]. These voice changes may be related to soft tissue trauma, hemorrhage, infection, endotracheal intubation, arytenoid trauma (e.g., arytenoid dislocation), and strap muscles injury, which impairs vertical laryngeal movement or causes laryngotracheal fixation [84]. Such alterations can cause vocal fatigue, difficulty with singing high notes, and reduced vocal range [90,91,92], and may be temporary or permanent [36].
Voice changes in pituitary gland disorders
Disorders leading to deficiency in pituitary hormones are rare, and voice changes are not always obvious. Pituitary hormone excess, resulting from functional (i.e., endocrine-active or secreting) adenomas of the pituitary, is more common. As symptoms are generally insidious in onset and often nonspecific, a smart phoniatrician may be the first to suspect and diagnose a pituitary adenoma [2].
Growth Hormone
Excess growth hormone (GH) in adults causes acromegaly. The cartilaginous larynx widens and grows; the vocal folds become thickened, dropping the fundamental voice frequency and deepening the voice. Due to the general muscular weakness associated with the disease, the voice may be weak, sometimes phonasthenic [47]. Although much of the upper respiratory compromise is due to macroglossia and hypertrophy of pharyngeal soft tissue, cases of slowly progressive laryngeal obstruction requiring tracheotomy have been reported [93]. The cricoarytenoid joints may become fixed in acromegalics due to ankylosis of the cricoarytenoid joint. This could be related to the GH activity on joint chondrocalcification [94]. Pituitary adenomectomy has been shown to normalize vocal fundamental frequency within a few weeks of surgery [93]. Other physical changes (e.g., large hands, prominent jaw) are frequently permanent [2].
Adrenocorticotropic Hormone (ACTH)
Increased pituitary ACTH production causes Cushing’s disease. Voice changes are more noticeable in females than males and can range from mild changes resembling premenstrual voice changes to severe, irreversible virilization of the voice [2].
Prolactin
In females, prolactin-secreting tumors are manifested by amenorrhoea, infertility, and galactorrhea because high prolactin levels block the natural Luteinizing hormone (LH) surge that initiates ovulation. Voice changes are similar to premenstrual voice changes. Men with prolactinomas usually complain only of diminished libido, and voice changes are not noticeable [2].
Voice changes in adrenal gland disorders
Congenital adrenal hyperplasia (CAH) is an autosomal recessive disorder that results in 95% of cases from 21-hydroxylase deficiency. This causes deficient production of cortisol and often aldosterone, and overproduction of androgens [95, 96].
Nygren et al. [14] found that females with CAH showed lower voice pitch and darker voice timbre when compared with controls. The authors attributed these voice changes to the effects of androgens on the VF structure and suggested that late diagnosis or improper treatment with glucocorticosteroids after birth could be the cause.
Voice changes in diabetes
Dysphonia is encountered in 12.5% of diabetic patients, which is more than twice as common as in healthy people. Diabetes is well known to cause microvascular disease, which can lead to diabetes-related neuropathy and myopathy that affect laryngeal function [97]. Neuropathy leads to a gradual loss of fine motor control, which may be noticed early by a professional voice user. Neuropathy may also result in vocal fold paralysis in advanced cases [98]. Hamdan et al. [99] found that diabetic patients had a higher prevalence of laryngeal sensory neuropathy as compared to healthy individuals. The authors suggested that symptoms like cough and spasm could be a possible consequence of this state [58]. Xerostomia, xerophonia, and hearing loss in long-standing diabetes also contribute to voice changes in these patients [36]. Furthermore, diabetes mellitus is linked to a higher risk of infection, generalized fatigue, edema, inadequate wound healing, and other health issues that could affect voice performance [2].
Conclusion
Hormone imbalances and dysfunction commonly affect the voice, and dysphonia may be the initial sign of a serious systemic illness. Phoniatricians must be continually alert for hormonal dysfunction in patients with voice problems. Collaboration with an expert endocrinologist interested in professional voice problems is crucial [2]. Further research is needed to extend and enrich our knowledge of hormone-related voice changes.
Availability of data and materials
Not applicable.
Abbreviations
- ACTH:
-
Adrenocorticotropic Hormone
- APA:
-
Auditory Perceptual Assessment
- CAH:
-
Congenital Adrenal Hyperplasia
- EBSLN:
-
External Branch of the Superior Laryngeal Nerve
- ENT:
-
Ear, Nose, and Throat
- GH:
-
Growth Hormone
- H/N:
-
Harmonic to Noise
- HRT:
-
Hormone Replacement Therapy
- LH:
-
Luteinizing Hormone
- MPT:
-
Maximum Phonation Time
- PCOS:
-
Polycystic Ovarian Syndrome
- PMS:
-
Premenstrual Syndrome
- RLN:
-
Recurrent Laryngeal Nerve
- SLN:
-
Superior Laryngeal Nerve
- UVFP:
-
Unilateral Vocal Fold Paralysis
- VFs:
-
Vocal Folds
References
Hiller-Sturmhöfel S, Bartke A (1998) The endocrine system: an overview. Alcohol Health Res World 22(3):153–164
Anderson TD, Anderson DD, Sataloff RT (2017) Endocrine Function. In: Sataloff RT (ed) Clinical assessment of voice, 2nd edn. Plural Publishing, San Diego: CA, pp 275–289
Newman SR, Butler J, Hammond EH, Gray SD (2000) Preliminary report on hormone receptors in the human vocal fold. JVoice 14:72–81. https://doi.org/10.1016/s0892-1997(00)80096-x
Altman KW, Haines GK, Vakkalanka SK, Keni SP, Kopp PA, Radosevich JA (2003) Identification of thyroid hormone receptors in the human larynx. Laryngoscope 113:1931–1934. https://doi.org/10.1097/00005537-200311000-00014
Kirgezen T, Sunter AV, Yigit O, Huq GE (2017) Sex hormone receptor expression in the human vocal fold subunits. J Voice 31:476–482. https://doi.org/10.1016/j.jvoice.2016.11.005
Hirano M (1989) Objective evaluation of the human voice: Clinical aspects. Folia Phoniatr Logop 41:89–144
Hillman R, Montgomery W, Zeitels SM (1997) Appropriate use of objective measures of vocal function in the multidisciplinary management of voice disorders. Current Diagnostic and Office Practice 5:172–175
Behrman A (2005) Common practices of voice therapists in the evaluation of patients. J Voice 19(3):454–469. https://doi.org/10.1016/j.jvoice.2004.08.004
Roy N, Barkmeier-Kraemer J, Eadie T, Sivasankar MP, Mehta D, Paul D, Hillman R (2013) Evidence-based clinical voice assessment: A systematic review. Am J Speech Lang Pathol 22:212–226. https://doi.org/10.1044/1058-0360(2012/12-0014)
Patel RR, Awan SN, Barkmeier-Kraemer J, Courey M, Deliyski D, Eadie T, Paul D, Švec JG, Hillman R (2018) Recommended Protocols for Instrumental Assessment of Voice: American Speech Language-Hearing Association Expert Panel to Develop a Protocol for Instrumental Assessment of Vocal Function. Am J Speech Lang Pathol 27:887–905
Kotby N (1986) Voice disorders: recent diagnostic advances EJO 3:69–98
Jacobson BH, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger MS (1997) The Voice Handicap Index (VHI): development and validation. Am J Speech Lang Pathol 6:66–70
Abitbol J, Abitbol P, Abitbol B (1999) Sex hormones and the female voice. J Voice 13(3):424–446
Nygren U, Sodersten M, Falhammar H, Thorén M, Hagenfeldt K, Nordenskjöld A (2009) Voice characteristics in women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Clin Endocrinol 70:18–25
Davis CB, Davis ML (1993) The effects of premenstrual syndrome (PMS) on the female singer. J Voice 7(4):337–353
Luchsinger R, Arnold G (1965) Voice-speech-language clinical communicology: It’s physiology and pathology. Wadsworth, Belmont, CA
Voelter Ch, Kleinsasser N, Joa P, Nowack I, Martínez R, Hagen R, Voelker HU (2008) Detection of hormone receptors in the human vocal fold. Eur Arch Oto-Rhino-Laryngol 265:1239–1244. https://doi.org/10.1007/s00405-008-0632-x
Brunings JW, Schepens JJ, Peutz-Kootstra CJ, Kross KW (2013) The expression of estrogen and progesterone receptors in the human larynx. J Voice 27(3):376–380. https://doi.org/10.1016/j.jvoice.2013.01.011
Shoffel-Havakuk H, Carmel-Neiderman N, Halperin D, Galitz YS, Levin D, Haimovich Y, Cohen O, Abitbol J, Lahav Y (2018) Menstrual Cycle, Vocal Performance, and Laryngeal Vascular Appearance: An Observational Study on 17 Subjects. J Voice 32(2):226–233. https://doi.org/10.1016/j.jvoice.2017.05.001
Chae SW, Choi G, Kang HJ, Choi JO, Jin SM (2001) Clinical analysis of voice change as a parameter of premenstrual syndrome. J Voice 15(2):278–283. https://doi.org/10.1016/S0892-1997(01)00028-5
Ryan M, Kenny D (2009) Perceived effects of the menstrual cycle on young female singers in the Western classical tradition. J Voice 23(1):99–108. https://doi.org/10.1016/j.jvoice.2007.05.004
Postma G, Courey M, Ossoff R (1998) Microvascular lesions of the true vocal fold. Ann Otol Rhinol Laryngol 107(6):472–476
Gugatschka M, Kiesler K, Obermayer-Pietsch B, Schoekler B, Schmid C, Groselj-Strele A, Friedrich G (2010) Sex hormones and the elderly male voice. J Voice 24(3):369–373. https://doi.org/10.1016/j.jvoice.2008.07.004
Hamdan A-L, Mahfoud L, Sibai A, Seoud M (2009) Effect of pregnancy on the speaking voice. J Voice 23(4):490–493. https://doi.org/10.1016/j.jvoice.2007.11.006
La FMB, Sundberg J (2012) Pregnancy and the singing voice: reports from a case study. J Voice 26(4):431–439
Ghaemi H, Dehqan A, Mahmoodi-Bakhtiari B, Scherer RC (2020) Voice changes during pregnancy trimesters in Iranian pregnant women. J Voice 34(3):358–363. https://doi.org/10.1016/j.jvoice.2018.09.016
Kosztyła-Hojna B, Łobaczuk-Sitnik A, Biszewska J, Moskal-Jasińska D, Kraszewska A, Zdrojkowski M, Duchnowska E (2018) Subjective and objective assessment of voice quality in pregnancy. Otolaryngol Pol 73(2):1–5
Li X, Xu W (2021) Clinical Characteristics of Women With Low Vocal Pitch During Pregnancy. J Voice 35(1):113–115. https://doi.org/10.1016/j.jvoice.2019.06.018
Ellegard E, Hellgren M, Toren K, Karisson G (2000) The incidence of pregnancy rhinitis. Gynecol Obstet Invest. 49:98–101. https://doi.org/10.1159/000.010.223
Alves M, Kruger E, Pillay B, van Lierde K, van der Linde J (2019) The effect of hydration on voice quality in adults: a systematic review. J Voice. 33(1):125.e13-125.e28. https://doi.org/10.1016/j.jvoice.2017.10.001
Cassiraga VL, Castellano AV, Abasolo J, Abin EN, Izbizky GH (2012) Pregnancy and voice: changes during the third trimester. J Voice 26(5):584–586
Salturk Z, Kumral TL, Bekiten G, Atar Y, Atac E, Aydoğdu I, Yıldırım G, Kılıc A, Uyar Y (2016) Objective and Subjective Aspects of Voice in Pregnancy. J Voice 30(1):70–73
Ulkumen B, Artunc-Ulkumen B, Celik O (2022) Impact of pregnancy on voice: a prospective observational study. Logoped Phoniatr Vocol 47(3):183–188. https://doi.org/10.1080/14015439.2021.1903076
Hancock AB, Gross HE (2015) Acoustic and aerodynamic measures of voice during pregnancy. J Voice 29:53–58
Bruzzi C, Salsi D, Minghetti D, Negri M, Casolino D, Sessa M (2017) Presbyphonia. Acta. Biomedica 88(1):6–10. https://doi.org/10.23750/abm.v88i1.5266
Hari Kumar K, Garg A, Ajai Chandra NS, Singh SP, Datta R (2016) Voice and endocrinology. Indian J Endocrinol Metab 20:590–594. https://doi.org/10.4103/2230-8210.190523
Amir O, Kishon-Rabin L (2004) Association between birth control pills and voice quality. Laryngoscope 114:1021–1026. https://doi.org/10.1097/00005537-200406000-00012
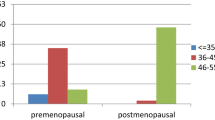
D’haeseleer E, Depypere H, Van Lierde K, (2013) Comparison of speaking fundamental frequency between premenopausal women and postmenopausal women with and without hormone therapy. Folia Phoniatr Logop 65:78–83
Hamdan HL, Tabet G, Fakhri G, Sarieddine D, Btaiche R, Seoud M (2018) Effect of Hormonal Replacement Therapy on Voice. J Voice 32(1):116–121. https://doi.org/10.1016/j.jvoice.2017.02.019. (Epub 2017 Mar 27)
Matsumoto AM (2002) Andropause: clinical implications of the decline in serum testosterone levels with aging in men. The Journals of Gerontology: Series A 57(2):M76-99. https://doi.org/10.1093/gerona/57.2.m76
Zamponi V, Mazzilli R, Mazzilli F, Fantini M (2021) Effect of sex hormones on human voice physiology: from childhood to senescence. Hormones (Athens) 20(4):691–696. https://doi.org/10.1007/s42000-021-00298-y
Sheehan MT (2004) Polycystic ovarian syndrome: diagnosis and management. Clin Med Res. 2:13–27. https://doi.org/10.3121/cmr.2.1.13
Nygren U, Isberg B, Arver S, Hertegård S, Södersten M, Nordenskjöld A (2016) Magnetic resonance imaging of the vocal folds in women with congenital adrenal hyperplasia and virilized voices. J Speech Lang Hear Res 59:713–721. https://doi.org/10.1044/2016_JSLHR-S-14-0191
Hannoun A, Zreik T, Husseini ST, Mahfoud L, Sibai A, Hamdan AL (2011) Vocal changes in patients with polycystic ovary syndrome. J Voice 25:501–504. https://doi.org/10.1016/j.jvoice.2009.12.005
Aydin K, Akbulut S, Demir MG, Demir S, Ozderya A, Temizkan S, Sargin M (2016) Voice characteristics associated with polycystic ovary syndrome. Laryngoscope 126:2067–2072. https://doi.org/10.1002/lary.25818
Alam N, Sinha V, Kumar SS, Katarkar A, Jain A (2012) Efficacy of voice therapy for treatment of Puberphonia: Review of 20 cases. World Articles in Ear, Nose and Throat 5(1)
Kotby MN, Hegazi M (2016) Voice disorders caused by diseases of the endocrinal glands. In: Kotby MN (ed) Clinical vocology (volume II). Published by the Egyptian Society of Phoniatrics and Logopedics (ESPL). El Hariry print, Cairo, Egypt
Morrison M, Rammage L (1994) The Management of Voice Disorders. Chapman & Hall Medical, London
Aronson AE, Bless DM (2009) Clinical voice disorders. Thieme Medical Publishers, New York, NY
Strauss RH, Mariah T, Liggett MS, Lanese RR (1985) Anabolic steroid use and perceived effects in ten-weight-trained women athletes. JAMA 253(19):2871–2873. https://doi.org/10.1001/jama.1985.03350430083032
Bermon S, Vilain E, Fenichel P, Ritzen M (2015) Women with hyperandrogenism in elite sports: scientific and ethical rationales for regulating. J Clin Endocrinol Metab 100(3):828–830. https://doi.org/10.1210/jc.2014-3603
Bourdial J (1970) Les troubles de la voix provoqués par la thérapeutique hormonale androgène. Annales d’oto-laryngologie et de chirurgie cervico faciale 87:725–734
Pahn J, Goretzlehner G (1978) Stimmestrungen durch hormonale Kontrazeptiva. Zentralbl Gynakol 100:341–346
Wentz AC (1988) Dysmenorrhea, premenstrual syndrome and related disorders. In: Jones HW, Wentz AC, Burnett LS (eds) Novak’s Textbook of Gynecology. Williams and Wilkins, Baltimore, MD, pp 240–262
La FMB, Howard DM, Ledger W, Davidson JW, Jones G (2009) Oral contraceptive pill containing drospirenone and the professional voice: an electrolaryngographic analysis. Logoped Phoniatr Vocol 34:11–19. https://doi.org/10.1080/14015430802538879
Amir O, Biron-Shental T, Muchnik C, Kishon-Rabin L (2003) Do oral contraceptives improve vocal quality? Limited trial on low-dose formulations. Obstet Gynecol 101(4):773–777. https://doi.org/10.1016/S0029-7844(02)03126-5
McIvor NP, Flint DJ, Gillibrand J, Morton RP (2000) Thyroid surgery and voice related outcomes. ANZ J Surg 70:179–183. https://doi.org/10.1046/j.1440-1622.2000.01781.x
Stogowska E, Kamiński KA, Ziółko B, Kowalska I (2022) Voice changes in reproductive disorders, thyroid disorders and diabetes: a review. Endocr Connect 11(3):e210505. https://doi.org/10.1530/EC-21-0505
Chaker L, Bianco AC, Jonklaas J, Peeters RP (2017) Hypothyroidism Lancet 390:1550–1562. https://doi.org/10.1016/S0140-6736(17)30703-1
Mohammadzadeh A, Heydari E, Azizi F (2011) Speech impairment in primary hypothyroidism. J Endocrinol Invest 34:431–433. https://doi.org/10.1007/BF03346708
Ritter FN (1973) Endocrinology. In: Paparella M, Shumrick D (eds) Otolaryngology, vol 1. WB Saunders, Philadelphia, PA, pp 727–734
Sorensen JR, Winther KH, Bonnema SJ, Godballe C, Hegedüs L (2016) Respiratory manifestations of hypothyroidism: a systematic review. Thyroid 26(11):1519–1527
Birkent H, Karacalioglu O, Merati AL, Akcam T, Gerek M (2008) Prospective study of the impact of thyroid hormone replacement on objective voice parameters. Ann Otol Rhinol Laryngol 117(7):523–527. https://doi.org/10.1177/000348940811700710
De Leo S, Lee SY, Braverman LE (2016) Hyperthyroidism Lancet 388(10047):906–918. https://doi.org/10.1016/S0140-6736(16)00278-6
Kravets I (2016) Hyperthyroidism: diagnosis and treatment. Am Fam Physician 93:363–370
Stemple JC, Roy N, Klaben BK (2014) Clinical voice pathology: Theory and management (5th ed.). San Diego: Plural Publishing
Kovacic G (2018) Voice and hyperthyroidism: Subjective voice complaints and alterations of the acoustic parameters of the voice. Research and Review Insights 2(1):1–4. https://doi.org/10.15761/RRI.1000129
Afsah O, Khashaba E, Nomir M, Abass N, Elsaeed A, Abou-Elsaad T (2022) Voice Evaluation in Patients with Hyperthyroidism. EJENTAS 23(23):1–7. https://doi.org/10.21608/EJENTAS.2022.130488.1490
Silverberg SJ, Bilezikian JP (2001) Primary hyperparathyroidism. In: Kenneth L et al (eds) Principles and practice of endocrinology and metabolism, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
Jan De Beur SM, Elizabeth A, Streeten EA et al (2001) Hypoparathyroidism and other causes of hypocalcemia. In: Becker KL (ed) Principles and practice of endocrinology and metabolism, 3rd edn. Philadelphia, Lippincott Williams and Wilkins
Schlosser K, Zeuner M, Wagner M, Slater EP, Domínguez Fernández E, Rothmund M, Maschuw K (2007) Laryngoscopy in thyroid surgery – Essential standard or unnecessary routine? Surgery 142:858–864
Fernandez-Ranvier GG, Jensen K, Khanafshar E, Quivey JM, Glastonbury C, Kebebew E, Duh Q, Clark OH (2007) Nonfunctioning parathyroid carcinoma: Case report and review of literature. Endocr Pract 13:750–757. https://doi.org/10.4158/EP.13.7.750
Ho TWT, McMullen TP (2011) Secondary hyperparathyroidism presenting with vocal cord paralysis. World Journal of Endocrine Surgery 3(3):122–124. https://doi.org/10.5005/jp-journals-10002-1073
Timon CI, Hirani SP, Epstein R, Rafferty MA (2010) Investigation of the impact of thyroid surgery on vocal tract steadiness. J Voice 24(5):610–613. https://doi.org/10.1016/j.jvoice.2009.02.003
Randolph GA, Sritharan N, Song P, Franco R Jr, Kamani D, Woodson G (2015) Thyroidectomy in the professional singer-neural monitored surgical outcomes. Thyroid 25(6):665–671. https://doi.org/10.1089/thy.2014.0467
LaBlance GR, Maves MD (1992) Acoustic characteristics of post-thyroplasty patients. Otolaryngol Head Neck Surg 107:558–563
Lundy DS, Casiano RR (1995) ‘Compensatory falsetto’: effects on vocal quality. J Voice 9:439–442
Woodson GE (1993) Configuration of the glottis in laryngeal paralysis I: Clinical study. Laryngoscope. 103(Pt 1):1227–1234
Rosen CA, Simpson CB (2008) Operative techniques in laryngology. Springer-Verlag, Berlin, Heidelberg
Rontal E, Rontal M (2003) Permanent medialization of the paralyzed vocal fold utilizing botulinum toxin and Gelfoam. J Voice 17:434–441
Belafsky PC, Postma GN, Reulbach TR, Holland BW, Koufman JA (2002) Muscle tension dysphonia as a sign of underlying glottal insufficiency. Otolaryngol Head Neck Surg 127:448–451. https://doi.org/10.1067/mhn.2002.128894
Kitzing P (1985) Stroboscopy — a pertinent laryngological examination. J Otolaryngol 14:151–157
Dursun G, Sataloff RT, Spiegel JR, Mandel S, Heuer RJ, Rosen DC (1996) Superior laryngeal nerve paresis and paralysis. J Voice 10:206–211
Aluffi P, Policarpo M, Cherovac C, Olina M, Dosdegani R, Pia F (2001) Post-thyroidectomy superior laryngeal nerve injury. Eur Arch Oto-Rhino-Laryngol 258:451–454. https://doi.org/10.1007/s004050100382
Stojadinovic A, Shana A, Orlikoff R, Nissan A, Kornak M-F, Singh B, Boyle JO, Shah JP, Brennan MF, Kraus DH (2002) Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg 236(6):823–832. https://doi.org/10.1097/00000658-200212000-00015
Soylu L, Ozbas S, Uslu HY, Kocak S (2007) The evaluation of the causes of subjective voice disturbances after thyroid surgery. Am J Surg 194:317–322. https://doi.org/10.1016/j.amjsurg.2006.10.009
Rubin AD, Praneetvatakul V, Heman-Ackah YD, Moyer CA, Mandel S, Sataloff RT (2005) Repetitive phonatory tasks for identifying vocal fold paresis. J Voice 19:679–686. https://doi.org/10.1016/j.jvoice.2004.11.001
Tanaka S, Hirano M, Umeno H (1994) Laryngeal Behavior in Unilateral Superior Laryngeal Nerve Paralysis. Ann Otol Rhinol Laryngol 103:93–97
Roy N, Smith ME, Houtz DR (2011) Laryngeal Features of External Superior Laryngeal Nerve Denervation: Revisiting a Century-Old Controversy. Ann Otol Rhinol Laryngol 120(1):1–8. https://doi.org/10.1177/000348941112000101
Hwan Hong K, Ye M, Mo Kim Y, Kevorkian K, Berke G (1997) The role of strap muscles in phonation—in vivo canine laryngeal model. J Voice 11(1):23–32
Sinagra DL, Montesinos MR, Tacchi VA, Moreno JC, Falco JE, Mezzadri NA, Debonis DL, Curutchet HP (2004) Voice changes after thyroidectomy without recurrent laryngeal nerve injury. J Am Coll Surg 199:556–560. https://doi.org/10.1016/j.jamcollsurg.2004.06.020
Henry LR, Solomon NP, Howard R, Gurevich-Uvena J, Horst LB, Coppit G, Orlikoff R, Libutti SK, Shaha AR, Stojadinovic A (2008) The functional impact on voice of sternothyroid muscle division during thyroidectomy. Ann Surg Oncol 15:2027–2033. https://doi.org/10.1245/s10434-008-9936-8
Williams RG, Richards SH, Mills RG, Eccles R (1994) Voice changes in acromegaly. Laryngoscope 104:484–487
Motta S, Ferone D, Colao A, Merola B, Motta G, Lombardi G (1997) Fixity of vocal cords and laryngocele in acromegaly. J Endocrinol Invest 20:672–674. https://doi.org/10.1007/BF03348030
White PC, Speiser PW (2000) Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocr Rev 21:245–291
Merke DP, Bornstein SR (2005) Congenital adrenal hyperplasia. Lancet 365:2125–2136
Bainbridge KE, Roy N, Losonczy KG, Hoffman HJ, Cohen SM (2017) Voice disorders and associated risk markers among young adults in the United States. Laryngoscope 127:2093–2099. https://doi.org/10.1002/lary.26465
Sommer DD, Freeman JF (1994) Bilateral vocal cord paralysis associated with diabetes mellitus: case reports. J Otolaryngol 23(3):169–171
Hamdan A-L, Dowli A, Barazi R, Jabbour J, Azar S (2014) Laryngeal sensory neuropathy in patients with diabetes mellitus. J Laryngol Otol 128:725–729. https://doi.org/10.1017/S002221511400139X
Acknowledgements
Not applicable.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
OA was responsible for the study idea, data collection, writing the manuscript and submission of the manuscript to the journal.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
No competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Afsah, O. Effects of hormonal changes on the human voice: a review. Egypt J Otolaryngol 40, 22 (2024). https://doi.org/10.1186/s43163-024-00578-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-024-00578-5